Vaccination for children today is considered the only proven way to protect against serious infections. WHO research statistics confirm a significant decline in the number of reported cases of many diseases. For example, today there are already 2 cases of paralytic poliomyelitis considered an emergency. Previously, about 7,700 cases were registered in Europe every year. Today, thanks to vaccinations, smallpox has been completely defeated, the last case of which was registered in 1978. The incidence of diphtheria has decreased by 90%. According to WHO, from 2000 to 2015, measles vaccines saved about 20 million lives.
Vaccination of children: pros and cons
The debate between supporters and opponents of vaccines began in 1998, when Dr. Andrew Wakefield published his research in the American medical journal The Lancet. In it, he claimed that children develop autism after receiving the mumps, measles and rubella vaccine. Dr. Wakefield supported his conclusions with the results of observations of 12 patients. However, medical journalist Brian Dear decided to meet with the parents of the observed children. It turned out that three had been diagnosed with autism before vaccination, and another five already had other neurological problems. As a result, it was possible to find out that Dr. Wakefield, before his research, developed and patented a monovaccine against measles. He recommended it instead of the drug used, which helped protect against three diseases at once. Wakefield's article was refuted, but public doubts were never completely dispelled.
Modern opponents of vaccinations cite as one of their arguments the presence of a mercury-based preservative in vaccines, which allegedly causes autism in children. However, the use of this component has been prohibited in the United States since 2002. However, the number of cases of autism is not decreasing. In 2014, Australian scientists examined the medical records of more than a million children belonging to different age groups. It turned out that there is no connection between mercury preservatives and cases of autism.
What is vaccination?
Vaccination is the process of giving people vaccines, drugs that help build immunity against many infectious diseases.
Vaccine prevention begins at birth. In childhood, it is especially important for protection against infection with dangerous infections and for creating strong immunity for life. The World Health Organization (WHO) considers vaccination one of the main ways to combat infections. Thanks to vaccines, it was possible to eliminate some diseases (the last case of smallpox was registered in 1978) and significantly limit the spread of others (tetanus, measles, polio).
In what cases should vaccination not be carried out?
- Acute febrile condition, for example, with ARVI. As soon as the temperature drops, you can wait 3-4 days and get vaccinated. A runny nose and cough without fever are not a contraindication to vaccination!
- Seizures (children with epilepsy who do not show seizures on medications can be vaccinated).
- Exacerbation of chronic diseases. At the same time, atopic dermatitis, anemia, benign neutropenia of childhood and other asymptomatic or easily removable conditions are not contraindications.
- Severe reaction to a previous administration of the same vaccine. At the same time, a vaccine against a specific infection can and should be replaced with an analogue.
- There is one more contraindication for live vaccines: immunodeficiency - primary (congenital), HIV infection or resulting from treatment with hormones or chemotherapy. All these conditions cannot be “accidentally overlooked.”
- It is important that vaccination should not be delayed due to “incorrect” test results. Moreover, the requirement to take tests before vaccination is unlawful, and you can refuse to do so.
What is revaccination?
In some cases, vaccine immunity lasts until the end of life after the first vaccination, but more often, in order to achieve the desired effect, you need to undergo revaccination (repeated administration of the vaccine) in time, sometimes more than one. Revaccination is carried out at strict intervals: a certain amount of time must pass between the first and subsequent applications of the vaccine, depending on the type of vaccination.
Important! Adults also need revaccination against some diseases: annually against influenza, every 10 years against diphtheria and tetanus. Young women planning a pregnancy may need to be vaccinated against rubella and measles if they have not had the disease, were not vaccinated, or received only one dose of the vaccine as a child.
What should a child be vaccinated and when?
We have compiled for you our own extended list of infections against which your baby must be vaccinated.
In some places we also indicate specific vaccines, but at the time of writing this article there are significant difficulties with their supply in St. Petersburg. Most vaccines for a specific disease are interchangeable. When choosing a vaccine, remember that combination vaccines (those that include vaccines against several infections at once) are better than single vaccines. So, vaccinate your baby against the following diseases:
- tuberculosis - in the maternity hospital;
- hepatitis B - first vaccination in the maternity hospital, then at 1 and 6 months;
- rotavirus - from 6 weeks;
- whooping cough, diphtheria, tetanus, polio, hemophilus influenzae. There is a Pentaxim vaccine that protects against all these diseases at once, as well as Infanrix Hexa, which in addition to them also contains a vaccine against hepatitis B. The timing of administration varies depending on the vaccines available to you, but in any case, vaccination against these diseases must be completed by 6 months;
- pneumococcus - (Prevenar, from 2 months);
- influenza - (annually in the fall, from 6 months);
- meningitis - (Menactra, from 9 months);
- measles, rubella, mumps - (Priorix or analogues, from 12 months);
- hepatitis A - from 12 months;
- chickenpox - from 12 months.
Consult with your pediatrician to schedule vaccines and when to give them.
What do vaccines consist of?
The goal of a vaccine is to mimic a disease without causing its symptoms. In this case, the human immune system reacts to the vaccine as to an infection, developing protection against wild pathogens (Fig. 1).
Figure 1. How vaccines work. A - individual parts of bacteria and viruses (antigens - green triangles in the figure) are recognized by our immune system, after which the body begins to resist infection. B - vaccines contain whole cells of pathogens, or their individual antigens, and the vaccine cannot cause disease. C - when antigens are introduced into the body, our immune system generates specific protective antibodies (Y in the figure). D - if we encounter an infection in the future, the body will be able to quickly recognize the pathogen by its antigens, the disease will not develop. Source
Vaccines can be based on:
- live, weakened viruses or bacteria (wild microorganisms are grown in the laboratory in cell cultures until they lose the ability to cause disease),
- killed whole viruses or bacteria (microorganisms are inactivated with formaldehyde or heating),
- individual antigens are parts of microorganisms that are recognized by our immune system (these can be proteins or polysaccharides of the cell wall of microorganisms or neutralized toxins that bacteria release into the environment).
It is these components that provoke an immune response, “teaching” the body to recognize the pathogen and destroy it. Some vaccines protect against several infections at once (for example, the three-part vaccine against whooping cough, diphtheria and tetanus).
In addition, vaccines may contain adjuvant substances (they are designed to enhance the effect of drugs), stabilizers, preservatives and antibiotics.
Get your child vaccinated. Vaccination.
Today, vaccination is one of the most effective ways to protect against infectious diseases. The principle of vaccination is as follows. An infectious agent (or an artificially synthesized protein identical to the agent’s protein) is introduced into the patient’s body. It should stimulate the formation of antibodies that will fight the infectious agent. This will allow the body to develop lasting immunity to a specific disease.
With the help of vaccination (vaccinations) of children in modern medicine, it is possible to successfully combat various types of viruses (measles, rubella, polio, mumps, hepatitis B viruses) or bacteria - the causative agents of tuberculosis, whooping cough, diphtheria, Haemophilus influenzae, tetanus, etc.
You can find out where and when you can get your child vaccinated by calling our Medical Center.
What is revaccination?
As we know, vaccination can be carried out both once and repeatedly. As a rule, vaccinations against mumps, tuberculosis, measles and other infections are given only once in a lifetime. For example, the DTP vaccine is administered several times.
Revaccination is a procedure essentially aimed at maintaining the immunity that has developed as a result of previous vaccinations. Typically, revaccination is carried out after a strictly defined period of time after the first vaccination against a specific infectious agent.
Types of vaccines
Vaccines introduced into the human body through vaccinations come in different forms. Depending on various parameters, all vaccines are divided into several categories.
- Live vaccines contain a weakened viral agent. These drugs include vaccines against polio, measles, mumps, rubella or tuberculosis. As a rule, they are obtained through selection. When they enter the body, they begin to multiply. In response to this, the human immune system produces antibodies, which form the basis of immunity against this infection. However, vaccination with live vaccines is not recommended for persons with immunodeficiency.
- Inactivated vaccines, or, in simpler terms, killed vaccines. They contain a whole microorganism killed under the influence of physical or chemical factors. Thus, the causative agent of infection is affected by temperature, radiation, ultraviolet light, alcohol, and formaldehyde. These vaccines include drugs against whooping cough and hepatitis A. Such vaccinations are given infrequently.
- Chemical vaccines. They contain components of cell walls or other parts of pathogens. Chemical preparations include some vaccines against whooping cough, Haemophilus influenzae, and meningococcal infection.
- Toxoids are vaccines that contain an inactivated toxin produced by certain bacteria. They undergo special processing and instead of toxic properties they receive immunogenic ones. These are vaccines, for example, against tetanus and diphtheria.
- Recombinant vaccines are sometimes called vector vaccines. These drugs are obtained using genetic engineering methods. The genes of the infectious agent, which are responsible for the production of protective antigens, are implanted into the genome of a harmless microorganism. Subsequently, it is he who produces and accumulates the necessary antigen. Recombinant vaccines against viral hepatitis B and rotavirus infection are known.
- Synthetic vaccines are artificially created recognizers of pathogenic bacteria.
- Associated vaccines are those that combine several components against various viral infections. An example of such a vaccination is DPT.
Why is it important to vaccinate children?
Vaccination is needed to protect a child from dangerous diseases that can cause severe complications, disability or even death. Thus, polio threatens paralysis, measles - encephalitis, pneumococcal infection - pneumonia and meningitis. Many parents, when deciding to vaccinate, are afraid of post-vaccination complications, but they are much less common than the severe consequences of the diseases against which children are vaccinated. Not to mention the drug burden on the liver, kidneys and other internal organs during treatment for vaccine-preventable infections.
There are no effective treatments for some infections. For other diseases, existing treatment may be ineffective (pathogens are increasingly developing resistance to antibiotics every year), and the child may suffer. Completing mandatory vaccinations is the most reliable prevention of such tragedies.
The baby's first months of life are protected from infections by the mother's antibodies, obtained through the placenta and with milk during breastfeeding, but this protection is not enough and weakens over time. Vaccinating children helps protect them from dangerous diseases. Even if the baby grows up in a safe environment, the risk of contracting dangerous infections remains. It will not be possible to completely control all his contacts, to exclude being with other people in the premises and the transmission of pathogens.
Important! In Russia, vaccines against major diseases are free. They are administered to children according to a specific schedule - the national vaccination calendar. A full course of vaccination allows you to build immunity against the twelve most dangerous infectious diseases. Vaccination of children is carried out under mandatory medical supervision, taking into account a number of conditions: health status, contraindications, allergies. This eliminates the risk of complications and forms stable immunity.
You should not refuse vaccinations also because this entails a number of restrictions:
- In the event of an epidemic threat, schools and kindergartens may refuse to allow unvaccinated children to attend. If quarantines are introduced sequentially for different reasons, and the incubation periods of diseases are long, the period of isolation can be up to several months. Violation of quarantine for a baby who has not been vaccinated is dangerous due to an increased risk of infection;
- a child who has not received polio vaccine should be separated from children vaccinated with oral polio vaccine for 60 days (live polio vaccine virus can be transmitted from child to child and is extremely rarely capable of causing symptoms of the disease if the child has not previously received an inactivated vaccine);
- a child without mandatory vaccinations may be prohibited from entering some countries.
The consequences of refusing vaccination can come back to haunt you in adulthood. When applying for a job that involves a risk of infection, or in an organization that monitors the health of employees, the applicant will not pass a medical examination.
An additional argument in favor of vaccination is the formation of herd immunity. If at least 80-95% of the population is vaccinated, the infection cannot spread, which means that the risk of getting sick is reduced for everyone, including those who cannot get vaccinated due to contraindications (Fig. 2).
Figure 2. How herd immunity is formed. A - there are no vaccinated people, and the infection affects almost everyone. B - There are few vaccinated people, almost all unvaccinated people get sick. C - there are many vaccinated people, the infection does not spread well. Source
Why do children need to be vaccinated so early? Is it possible to postpone vaccination?
Many people do this, but we don’t recommend it.
- Firstly, most vaccinated infections are deadly for young children. Deaths from whooping cough, pneumococcal pneumonia, and diseases caused by Haemophilus influenzae are most often recorded precisely at the age of 2-3 years. At 9-24 months there is a peak incidence of meningococcal meningitis, especially its invasive (most dangerous) form.
- Secondly, parental concerns about “immature immunity” are completely unfounded. The child’s immune system is constantly experiencing some antigenic load, and vaccination does not interfere, but helps it mature. Vaccinations are designed specifically for children. Of course, infant immunity is imperfect, so some vaccines are repeated. But following the correct schedule guarantees reliable protection against infection.
- Thirdly, the older the child, the more pronounced the reactions to vaccinations are, precisely because of the “ripe” immunity. This in itself is not scary, but redness and pain at the injection site, high fever and other “joys” are much more common in children with delayed vaccinations, and are not typical for infants.
Many parents ask the doctor to give them a waiver, and pediatricians follow their lead. In fact, neither colic, nor an umbilical hernia, nor small residual cysts in the baby’s brain, nor even a runny nose without a rise in temperature will in any way affect the child’s condition after vaccination. Such challenges have no medical basis. Unfortunately, most cases of severe childhood infections are detected in children whose parents decided to “just wait six months or a year.”
Are there risks?
Although the safety of each vaccine is strictly monitored, adverse reactions and complications cannot be ruled out when vaccinating children.
The most common undesirable effects after the administration of vaccines are not dangerous, pass quickly and do not require special treatment. This is redness at the injection site, fever, drowsiness, etc.
Complications are very rare (in 1% of cases, and severe ones are even less common) and are usually associated with defects in the immune system, allergic reactions, genetic predisposition, or the fact that the vaccine was given against the background of an acute respiratory viral infection. Before vaccination, the pediatrician must examine the child and only then issue a referral for vaccination.
Contraindications to vaccination may be:
- chronic disease or disease in the acute phase,
- suppressed immunity (for example, due to HIV infection or immunosuppressive therapy),
- neurological disorders,
- poor vaccine tolerance in the past,
- presence of allergies to vaccine components.
A complete list of contraindications is always indicated in the instructions for the vaccine product.
To further reduce the risk of complications, it is recommended:
- do not introduce new foods into the diet several days before and after vaccination, avoid contact with allergens;
- half an hour after the vaccine is administered, stay near the office or hospital in case an allergy develops, so that medical assistance can be quickly provided;
- follow the recommendations of the pediatrician and other doctors, report problems with the baby’s health after vaccination;
- 2 weeks before vaccination, it is advisable to avoid contact with infectious patients.
Why is hepatitis B vaccinated?
Hepatitis B is a mortal danger for a small child. If an adult, having become infected, can live in remission for decades and not even know about the disease, then in children this virus very quickly causes cirrhosis of the liver and cancer.
The hepatitis B virus lives in the environment for 7 days. Thus, it can live not only on medical instruments, but also on hygiene items, clothing, etc. Microcracks in the skin or mucous membrane are enough to transmit the virus. Thus, there is a risk with any medical procedure, not to mention blood transfusion in the event of a burn or accident.
In addition, 30% of virus carriers do not know about their illness. A mother can pass hepatitis B to her child even if she was tested during pregnancy, and especially if she was not tested. Therefore, it is very important to give your baby the hepatitis B vaccine within the first 24 hours after birth.
What vaccinations should a child have?
From the first day of life, children are routinely vaccinated against the following infections:
- hepatitis B,
- tuberculosis,
- polio,
- whooping cough,
- diphtheria,
- tetanus,
- hemophilus influenzae infection (for risk groups),
- parotitis,
- measles,
- rubella,
- pneumococcal infection,
- flu.
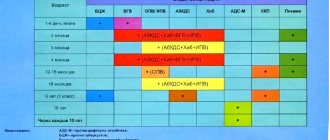
National vaccination calendar
Vaccination is carried out according to the schedule established in the National Preventive Vaccination Calendar (Table 1).
Information about all vaccinations is included in the medical card or vaccination certificate. Table 1. Vaccination schedule for children and adolescents according to the National Preventive Vaccination Calendar.
| Age | Graft | Vaccine |
| Children from birth to 3 years old | ||
| On the first day after birth | First vaccination against hepatitis B | Interchangeable mono-vaccines: Regevak B, Euvax B, etc. |
| 3-7 days of life | Vaccination against tuberculosis | BCG or BCG-M (with a reduced concentration of bacterial cells) |
| 1 month | Second vaccination against hepatitis B | Interchangeable mono-vaccines: Regevak B, Euvax B, etc. |
| 2 months | Risk groups: third vaccination against hepatitis B First vaccination against pneumococcal infection | Interchangeable mono-vaccines: Regevak B, Euvax B, etc. Conjugate vaccines: Prevenar-13 (against 13 serotypes) |
| 3 months | First vaccination against diphtheria, whooping cough, tetanus First polio vaccine Risk groups: first vaccination against Haemophilus influenzae | Contains whole pertussis bacteria: DPT Does not contain whole bacteria: Infanrix, Pentaxim, Tetraxim Does not contain pertussis component: ADS, ADS-M Inactivated vaccines: Polymilex, Poliorix, Imovax Polio, Tetraxim Act-HIB, Hiberix, Pentaxim |
| 4.5 months | Second vaccination against diphtheria, whooping cough, tetanus Risk groups: second vaccination against Haemophilus influenzae Second polio vaccine Second vaccination against pneumococcal infection | Contains whole pertussis bacteria: DPT Does not contain whole bacteria: Infanrix, Pentaxim, Tetraxim Does not contain pertussis component: ADS, ADS-M Act-HIB, Hiberix, Pentaxim Inactivated vaccines: Polymilex, Poliorix, Imovax Polio, Tetraxim Conjugate vaccines: Prevenar-13 (against 13 serotypes) |
| 6 months | Third vaccination against diphtheria, whooping cough, tetanus Third vaccination against viral hepatitis B Third polio vaccine Risk groups: third vaccination against Haemophilus influenzae | Contains whole pertussis bacteria: DTP, DTP-Hep B, Bubo-Kok Does not contain whole bacteria: Infanrix, Pentaxim, Tetraxim, Infanrix-Hexa Does not contain pertussis component: ADS, ADS-M Mono-vaccines: Regevak B, Euvax B, etc. Polyvalent vaccines: Infanrix Hexa, Bubo-Kok, Bubo-M Inactivated vaccines: Polymilex, Poliorix, Imovax Polio, Tetraxim, Infanrix Hexa, Pentaxim Live oral vaccines: BiVac Polio, MonoVac Polio type 2 Act-HIB, Hiberix, Pentaxim, Infanrix Hexa |
| 1 year | First vaccination against measles, rubella, mumps Risk groups: fourth vaccination against hepatitis B | MMR-II, Live measles culture vaccine, Live mumps-measles culture vaccine, Priorix Interchangeable mono-vaccines: Regevak B, Euvax B, etc. |
| 15 months | Revaccination (third dose) against pneumococcal infection | Conjugate vaccines: Prevenar-13 (against 13 serotypes) |
| 18 months | First revaccination (fourth dose) against polio First revaccination (fourth dose) against diphtheria, whooping cough, tetanus Risk groups: revaccination (fourth dose) against Haemophilus influenzae | Inactivated vaccines: Polymilex, Poliorix, Imovax Polio, Tetraxim Live oral vaccines: BiVac Polio, MonoVac Polio type 2 Contains whole pertussis bacteria: DPT Does not contain whole bacteria: Infanrix, Pentaxim, Tetraxim Does not contain pertussis component: ADS, ADS-M Act-HIB, Hiberix, Pentaxim |
| 20 months | Second revaccination (fifth dose) against polio | Inactivated vaccines: Polimilex, Poliorix, Imovax Polio Live oral vaccines: BiVac Polio, MonoVac Polio type 2 |
| Annually, starting from 6 months | Flu shot | Vaxigrip, Influvac and others |
| Children from 3 to 7 years old | ||
| 6 years | Revaccination (second dose) against measles, rubella, mumps | MMR-II, Live measles culture vaccine, Live mumps-measles culture vaccine, Priorix |
| 6-7 years | Second revaccination (fifth dose) against diphtheria and tetanus Revaccination against tuberculosis | ADS, ADS-M BCG or BCG-M (with a reduced concentration of bacterial cells) |
| Annually | Flu shot | Vaxigrip, Influvac and others |
| Pupils | ||
| Annually | Flu shot | Vaxigrip, Influvac and others |
| 14 years | Third revaccination (sixth dose) against diphtheria, tetanus Third revaccination (sixth dose) against polio | ADS, ADS-M Inactivated vaccines: Polimilex, Poliorix, Imovax Polio Live oral vaccines: BiVac Polio, MonoVac Polio type 2 |
The risk group for hepatitis B includes children: those born to carrier mothers who have viral hepatitis B or who have had viral hepatitis B in the third trimester of pregnancy, who do not have test results for hepatitis B markers, who use narcotic drugs or psychotropic substances, from families in which there is a carrier of the hepatitis B virus or a patient with acute viral hepatitis B and chronic viral hepatitis.
Children at risk for hemophilus influenzae include:
- with diseases of the nervous system, immunodeficiency states or anatomical defects leading to a sharply increased risk of contracting hemophilus influenzae infection;
- with intestinal development abnormalities;
- with cancer and/or receiving immunosuppressive therapy for a long time,
- with HIV infection,
- born from mothers with HIV infection,
- premature and low birth weight,
- located in children's homes.
What vaccinations do you need to get before kindergarten?
In Russia, children aged 2.5-3 years go to kindergarten. Therefore, before kindergarten, the child should already have vaccinations against:
- tuberculosis - 1 vaccination out of 2,
- hepatitis B - 3 vaccinations or 4 - for children at risk,
- pneumococcal infection - 3 vaccinations,
- hemophilus influenzae infection - 4 vaccinations for children at risk,
- polio - 5 out of 6 vaccinations (3-5 doses - oral polio vaccine),
- whooping cough, diphtheria and tetanus - 4 out of 6 vaccinations,
- measles, rubella and mumps - 1 vaccine out of 2,
- influenza - annual vaccination from 6 months.
According to the law, if a child has not been vaccinated against these diseases, he will still be accepted into kindergarten. An organization’s refusal to visit the garden can only be justified by the worsening epidemiological situation in the region and the threat of an outbreak of a particular infection. But it is better to do everything necessary to reduce the risk of disease. You can get vaccinated and continue to attend kindergarten.
Every year, children attending educational organizations up to the age of 7 undergo a Mantoux test (tuberculin test) to detect tuberculosis. If the child is not vaccinated with the BCG vaccine, the test is done twice a year. You can avoid the test, but then to visit the kindergarten you will need a conclusion from a TB doctor confirming that the child is healthy. In this case, you may need: fluorography of both parents, x-ray of the child’s chest, passing other diagnostic tests for the presence of infection (Diaskintest, T-stop test).
Parents of children unvaccinated against polio face a different problem. If someone in the garden is vaccinated with the oral vaccine (which contains live polio virus), that child should be separated from those who have not yet received the live vaccine (children are vaccinated with OPV for the first time at 6 months of age as the third polio vaccine) for a period of time less than 60 days. Otherwise, unvaccinated children may get sick.
The main differences between vaccines in composition
Different vaccines differ from each other in composition, and therefore have different properties. Thus, whole-cell pertussis vaccines (DTP, DTP-Hep B, Bubo-Kok) are more difficult to tolerate than acellular ones (Infanrix, Pentaxim, Tetraxim, Infanrix-Gexa), but protect better against infection. If children do not tolerate the pertussis vaccine well, they can be vaccinated with drugs only against diphtheria and tetanus (ADS, ADS-M).
Live oral polio vaccines (BiVac Polio, MonoVac Polio type 2), known to very rarely cause polio, are not recommended for children of HIV-positive mothers and children in orphanages. They are vaccinated only with inactivated vaccines (Polimilex, Poliorix, Imovax Polio). At the request of the parents, all doses of the live vaccine can also be replaced with an inactivated one.
Sometimes vaccines vary in effectiveness and duration of action. For example, in addition to conjugate vaccines against pneumococcus (Prevenar-13), polysaccharide vaccines (Pneumo 23, Pneumovax 23) are used in Russia. Children under 2 years of age cannot be vaccinated with them, and protection after them lasts less time (3-5 years versus 8-10 years), but they protect against a larger number of pathogen serotypes.
Important! There is also a Calendar of preventive vaccinations for epidemic indications (if there is a possibility of the spread of certain infections, if the child is at risk).
Among others, it includes vaccination against tick-borne encephalitis, recommended for children and adults living in endemic regions (Urals, Siberia).
What vaccinations are there for whooping cough, diphtheria and tetanus?
- DTP is the most widely used vaccine in our country. It includes toxoid (neutralized toxin) of tetanus and diphtheria, as well as killed pertussis bacteria. In addition to the main components, the vaccine includes adjuvants, antiseptics and preservatives, as well as the main medium - a diluent.
- ADS and ADS-M are vaccines without a pertussis component. The ADS-M vaccine contains a reduced amount of diphtheria toxoid. These vaccines are used for revaccination in children after 7 years of age and in adults when whooping cough vaccination is no longer indicated.
- “Bubo-Kok” - in addition to the DTP components, this vaccine contains part of the hepatitis B viral protein. This is done in order to avoid giving the baby two injections at the same time, because Vaccinations according to the calendar are done together.
- "Bubo-M" is a vaccine without a pertussis component.
- "Pentaxim" - contains tetanus, diphtheria and pertussis toxoids, particles of the pertussis microbe. Additionally, polio has been added to this vaccine for ease of use. According to the vaccination calendar, the DTP and polio vaccination schedules coincide. A component against Haemophilus influenzae can be added to this vaccine from a separate vial. The decision about the need to administer it is made by the doctor. The vaccine is distinguished by the absence of whole pertussis cells - this causes fewer side effects.
- "Infanrix" is identical in composition to "Pentaxim", with the exception of the polio component - it is absent in it.
- "Infanrix hexa" - in addition to the components of "Infanrix", includes inactivated polio viruses and part of the hepatitis B virus protein.
- "Adasel" - includes: diphtheria, tetanus, pertussis toxoids and fragments of pertussis bacteria.
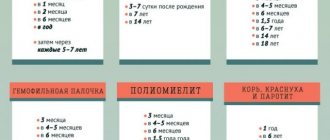
What vaccinations are not in the Calendar?
Today, in many developed countries, mass vaccination is carried out against a larger number of infections than in Russia. The Union of Pediatricians of Russia also advises children to have additional vaccinations against:
- rotavirus infection (three vaccinations at 2, 3 and 4.5 months),
- meningococcal infection (two vaccinations at 9 and 12 months),
- chickenpox (two vaccinations at 12-15 months and at 6 years),
- viral hepatitis A (two vaccinations at 20 months and 2-3 years),
- human papillomavirus infection (1 or 2 doses per 12-13 years).
Emergency vaccination
Sometimes children need emergency vaccinations.
If a child is bitten by a dog or other animal, he needs to receive a course of vaccinations against rabies (Fig. 3). If an unvaccinated child is scratched or injured, he should be vaccinated against tetanus. After exposure to people with hepatitis A and B, measles, mumps or chickenpox, immediate vaccination can help avoid complications. In any of these cases, contact the clinic as soon as possible.
Figure 3. What to do to eliminate the risk of rabies after a bite. Source
Why get vaccinated at such an early age?
In Soviet times, there was no question about the need for vaccination - it was mandatory. Now the situation has changed, and a child cannot be vaccinated without the consent of the parents, issued according to certain rules. Some are categorically against immunization, others postpone it to a later time, usually until they reach two years of age. Pediatricians, in turn, believe that the developed vaccination calendar takes into account all age-related characteristics, and the two-month procedure does not pose any danger; on the contrary, it is a step towards the formation of immunity.
Vaccination is the prevention of serious diseases. Thanks to it, it was possible to defeat such dangerous mass infections as tuberculosis or measles and avoid their epidemics. Timely immunization saves millions of children's lives every year.
The essence of the procedure is the introduction of weakened, killed or fragmented cells of viruses and bacteria into the body. The immune system reacts and begins to develop a tool to destroy them. This is how immunity is formed. The next time a real infectious agent attacks a person, the body will know how to defeat it.
Vaccinations for a child at 2 months are one of the stages of developing immunity.
Where and how are vaccinations given?
Children in Russia are vaccinated free of charge in clinics, kindergartens or schools (vaccination is carried out by health workers of medical, preschool or educational institutions). The health worker informs parents about which vaccines will be administered, as well as about possible vaccine reactions, complications after vaccination and the consequences of refusing it. Parents sign voluntary informed consent for the procedure.
The pediatrician examines the child, measures the temperature, interviews parents about previous diseases, including chronic diseases, allergies, etc. The results of the examination are entered into the medical record along with permission to administer the vaccine.
How is the procedure done?
In the vaccination or treatment room, the direction for vaccination and admission to it are checked. Before administering the vaccine, the nurse checks the name and expiration date of the drug, the integrity of the ampoule or other packaging. Vaccination is carried out according to the instructions for the drug and in compliance with the rules of antisepsis and asepsis. For half an hour after administration of the drug, it is necessary to remain near the vaccination office or medical facility in case an acute allergic reaction to the administered drug occurs.
What types of vaccinations are there?
During immunization, the drug can be administered in different ways:
- intramuscularly. The injection is given in the anterolateral thigh or upper arm. This method of administration is considered the most effective: the drug spreads better, immunity is formed faster, and the risk of allergies is minimal;
- orally. The vaccine must be swallowed. In this way they vaccinate against polio and enterovirus infections;
- intradermally. The injection is made with a thin needle into the upper arm or forearm (the area between the wrist and elbow). If the dose of the drug is administered correctly and not too deeply, the skin should turn whitish at the injection site;
- subcutaneously The injection is performed under the shoulder blade, in the front of the thigh or in the side of the shoulder, grasping a fold of skin with two fingers and “lifting” it;
- intranasally - through the nose (by spraying an aerosol, using ointments or creams). Such vaccines are rarely used; they usually do not form systemic immunity and are recommended for seasonal protection against infections that are transmitted by airborne droplets.
How to vaccinate correctly: what mothers need to know
The first thing to remember is how the vaccine is administered. There are several of them:
- intramuscularly;
- subcutaneously;
- cutaneously;
- intravenously;
- orally.
Infants are vaccinated intramuscularly or subcutaneously. In this case, intramuscular injection is carried out in the thigh or shoulder, since the procedure has been proven to be ineffective when injected into the buttock. The polio vaccine can be given in the form of drops that are placed in the baby's mouth.
The next, no less important, question is the place where the procedure will be carried out. This is either a clinic or a private center. In the first case, vaccination is completely free, using available drugs. If parents are not satisfied with the proposed remedy, they can purchase the necessary drug and bring it to the doctor. It is important to follow the rules of storage and transportation. Everything is simpler in the center. Vaccination is paid; the tariff includes the price of the desired vaccine and the cost of the procedure.
There are also rules that are important for every mother to remember.
- Immunization is carried out in accordance with the vaccination calendar. In essence, this is a list of mandatory vaccinations. Those not included in it are recommended. The calendar contains vaccination dates, which can be changed and selected individually if the baby was born premature, was sick at the time of the procedure, or had a blood transfusion.
- Before vaccination, the child must be examined by a doctor. The specialist will not only assess the condition of the little patient, but will also tell the mother about the features of the drug, possible reactions and remind her of what needs to be done to prevent the development of complications.
- The choice of vaccine is the right of parents.
- The vaccination is carried out by a specially trained specialist in the vaccination room, where all the necessary equipment is available to provide assistance to the child if necessary.
- You can refuse vaccinations.
How to prepare a child for vaccination?
Proper preparation for vaccination will help reduce the risk of adverse reactions and complications. To do this you need:
- take blood and urine tests;
- reduce the likelihood of contact with infectious patients 2–3 weeks before immunization;
- do not change your diet dramatically, do not introduce new products, so as not to provoke an allergy;
- Monitor the child’s well-being several days before the procedure. Tell your doctor if there are changes in behavior, lethargy or drowsiness, problems with bowel movements or appetite, fever, skin rash, or other symptoms.
An allergy sufferer may need antihistamines a few days before vaccination. They are given to children only as prescribed by a pediatrician. If a child takes allergy medications or any other medications during the vaccination period, the doctor should be informed about this. On the day of vaccination, the child must undergo a general medical examination.
Psychological preparation is also important. The calmer parents perceive the upcoming vaccination, the easier it will be for the baby to endure it. Immediately after the injection, small children may cry, and at this moment it is better to quickly distract them and redirect their attention, including so that negative associations with the doctor’s office are not reinforced.
What should be the intervals between vaccinations?
It has been established that longer than recommended intervals between vaccine doses do not significantly reduce the antibody response. In this regard, interruption of the immunization schedule does not require the restoration of the full vaccination series or the addition of additional doses of the vaccine. However, administering doses of vaccines or toxoids at shorter than recommended intervals may reduce the antibody response and should therefore be avoided. This is especially important for primary immunization.
The minimum interval is 1 month; after the administration of some live vaccines, the next vaccination can be administered only after 2 months; the correct sequence and duration of intervals is determined by the doctor in each specific situation.
What should you pay attention to after vaccination?
In the first 30 minutes after administration of the drug, it is important to carefully monitor the child’s well-being. Monitor activity, breathing, skin color (Fig. 4). There should be no signs of allergies, sudden increases or decreases in body temperature. If alarming symptoms appear, contact the vaccination office immediately.
You need to monitor your well-being for 1–2 days, checking:
- body temperature. It may be elevated after the administration of some vaccines, but normally becomes normal the next day (rarely every other day);
- skin condition. There may be slight redness and an injection mark at the injection site. There should be no rash, swelling or large area of redness.
- stool regularity, color and consistency;
- appetite is reduced on the first day after vaccination, but should return to normal;
- signs of allergies. There should be no itching, signs of breathing problems, or other symptoms of an allergic reaction;
- the general condition may deteriorate slightly in the first day or two after immunization, but then returns to normal.
Figure 4. Common side effects after receiving the influenza vaccine.
Source Important! If any unusual or alarming symptoms appear after vaccination, you should consult a doctor or call an ambulance.
Vaccination calendar for children
The pediatrician decides whether vaccinations can be done. A number of contraindications:
- immunodeficiency;
- chronic diseases;
- complications from vaccinations;
- allergic reaction to yeast;
- newborn weight up to 2 kg;
- allergy to egg white;
- convulsions;
- some diseases of the central nervous system.
Injections are given to the child only after the parents have signed the necessary documents. They must be signed before each vaccination. Parents may avoid the necessary injections, but then the health of their child is jeopardized.
Vaccinations for children under one year of age:
- In the first days after birth, the baby is vaccinated against hepatitis B;
- On days 3-7 an injection against tuberculosis is provided;
- In the first month, a second vaccination against hepatitis B is given;
- In the second month, a third vaccination against hepatitis B may be given for children at risk;
- In the third month, injections are given for whooping cough, tetanus, diphtheria and polio;
- On the fourth, a second vaccination against whooping cough, tetanus, diphtheria and polio is given;
- Two months later, the child is vaccinated against the same diseases for the third time;
- One-year-old babies are already vaccinated against mumps, measles and rubella.
Vaccination schedule for children from 1 year to 3 years:
- At the age of 1 year and 3 months, an injection is given for pneumococcal infection;
- At one and a half years, another vaccination is administered against whooping cough, tetanus, diphtheria and polio;
- A child aged 1 year and 8 months is vaccinated against polio.
List of vaccines for children aged 3 to 18 years:
During this period, repeated vaccinations and revaccinations are provided. This is necessary because the drugs used do not provide lifelong immunity.
- At 6 years old, the child is vaccinated again against mumps, measles and rubella;
- A year later, an injection is given for tetanus, diphtheria and BCG;
- At the age of 13, another vaccination against hepatitis B and rubella is provided;
- At age 14, children are vaccinated against tetanus, diphtheria and polio.
Pros and cons
The decision to vaccinate is made by parents. They have the right to refuse to vaccinate their child, regardless of all possible consequences.
Vaccination is opposed by parents who are afraid of serious complications or associate the development of certain diseases with vaccination. The risk of complications does exist, but it is very low. Doctors further reduce it by monitoring the child’s health before vaccination. At the slightest risk of allergies or other undesirable consequences, the doctor is obliged to adjust the child’s immunization program.
There are many arguments in favor of vaccinating children. This is protection from dangerous diseases with terrible, serious consequences, from infections that, in principle, cannot be cured. At the same time, the risk of complications is not comparable with the threat of infection.
What is a vaccination calendar?
The national vaccination calendar is a list of all vaccinations that the state provides to people free of charge to the entire population. As a rule, this calendar includes vaccines from domestic manufacturers, although there are exceptions. It is important that the national calendar is not a “list of all necessary vaccinations.” This list itself is broader, and it may include completely different vaccines. If parents have the opportunity to get vaccinated for a fee, they can supplement the calendar with those vaccines that are not included in it and replace the free vaccine options with paid ones.
All about the vaccination calendar