One of the fundamental principles of drug therapy is that the closer and more accurately the active substance is delivered to the affected area, the higher the effectiveness of the treatment. Therefore, the transportation of active compounds within the body, their pharmacodynamics and pharmacokinetics are key issues when developing instructions for the use of drugs. So, in the vast majority of cases, injections are more effective than tablets, and “targeted” injections have a number of advantages over, so to speak, conventional intramuscular (and even intravenous) injections.
Intravitreal injection refers to the introduction of drugs into the vitreous body, i.e. in close proximity to the zone of development of ophthalmological pathology. Intravitreal drugs are administered, in particular, for the treatment of diseases of the vascular system of the eye, elimination of the consequences of internal hemorrhages, treatment of age-related degenerative changes in the macula (“macula” - the most photosensitive central region of the retina), diabetic macular edema, inflammatory processes in the intraocular media, and etc.
Intravitreal injection technique
Although this procedure is called an injection, in terms of technical subtlety and complexity of execution it differs significantly from conventional injections, rather approaching microsurgical intervention. Therefore, all manipulations of this kind are performed only by an experienced, qualified surgeon in a specially equipped treatment room at an ophthalmology clinic.
Preparation includes treating the skin around the eyes with a disinfectant solution. For pain relief, epibulbar anesthesia is used (drip injection of a drug that blocks sensitivity onto the surface of the sclera).
The injection consists of a through puncture of part of the ciliary body. A special syringe with an ultra-thin needle is used, inserted at a distance of 4 mm from the limbus to a depth of 2-3 mm. To regulate the depth of the puncture, a special limiter is provided on the needle. After precise insertion of the needle, the required drug is injected into the vitreous body by slowly pressing the syringe plunger. The needle is then removed; The microscopic puncture does not require any sutures or other fixation.
At the end of the procedure, intraocular pressure must be measured. If its increase is detected, paracentesis is performed - an additional puncture of the cornea in the limbus area.
The final stage of the operation is the prophylactic instillation of antibacterial and anti-inflammatory drugs.
Intravitreal injections
In some cases, when treating eye diseases, it becomes necessary to prescribe intravitreal administration of the drug.
Intravitreal injection
- a method of administering drugs directly into the vitreous body. This type of injection is used in the treatment of age-related macular degeneration, diabetic macular edema, retinal vascular diseases, intraocular hemorrhages, and inflammation of the inner membranes of the eyeball.
The injection procedure is painless - special pain-relieving drops are instilled before the injection. Of course, when the anesthesia wears off, discomfort may occur. But they are easily tolerated.
Technique of drug administration.
An experienced ophthalmologist surgeon performs the intravitreal injection procedure in an ophthalmic operating room.
In the postoperative period, antibacterial and anti-inflammatory drops are instilled.
Intravitreal administration of the drug Lucentis.
Lucentis is used for:
— Treatment of age-related macular degeneration in adults (neovascular, or wet, form) — Treatment of loss of visual acuity caused by diabetic angiopathy and macular edema. The use of the drug can be independent or carried out in combination or after laser coagulation. — Treatment of decreased vision associated with macular edema due to retinal vein occlusion.
The active ingredient in Lucentis is ranibizumab. The substance is antibodies that prevent the proliferation of blood vessels that accompany diseases. Lucentis is an Anti-VEGF drug. According to studies, the drug prevents vision loss and even improves its sharpness. After the injection, an improvement in the condition of the retina is also observed.
The course of treatment required to stabilize the condition is 3 injections, once a month.
On an individual basis, when analyzing the current state of the patient’s visual functions, the course of treatment can be adjusted by an ophthalmologist. It is strongly recommended that you consult with your eye doctor several times a year.
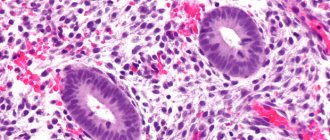
After the operation, the condition of the macula is necessarily monitored using the innovative SOCT Copernicus REVO coherence tomograph with angiography function.
This type of study allows you to obtain two- and three-dimensional images of the fundus, the resulting image is almost identical to histological sections, the study is non-contact. This allows the attending ophthalmologist to conduct extended research protocols and obtain an accurate diagnosis of the fundus in the postoperative period.
Intravitreal administration of the drug Eylea.
Dosage form : solution for intraocular administration.
Active substance: aflibercept 40 mg. Excipients: sodium dihydrogen phosphate monohydrate, sodium hydrogen phosphate heptahydrate, sodium chloride, sucrose, polysorbate 20, water for injection.
Eylea.
The drug is intended for the treatment of eye diseases. A drug for the treatment of vascular disorders of the periocular space. An agent that prevents the formation of new blood vessels. Anti-VEGF drug. Antineovascular agent. Aflibercept.
Aflibercept acts as a soluble decoy receptor that binds all VEGF-A and PIGF isoforms more efficiently than their natural receptors, and thus delays the binding and activation of natural VEGF receptors.
VEGF-A is a signaling protein produced by cells to stimulate the formation of the embryonic vascular system (vasculogenesis) and the growth of new vessels in an existing vascular system (angiogenesis)
PIGF - placental growth factor (part of the VEGF-A family)
Indications for use.
— neovascular (wet) age-related macular degeneration (AMD)
- visual impairment due to macular edema caused by occlusion of the retinal veins (central retinal vein (CRVO) and its branches (BRVO))
- visual impairment due to diabetic macular edema (DME)
— visual impairment due to myopic choroidal neovascularization (myopic CNV)
Intravitreal administration of the drug Gemaza.
Gemaza is an injection drug that has a pronounced thrombolytic effect.
The drug contains the following components:
1. Recombinant prourokinase is a well-studied fibrinolytic that provides rapid transformation of fibrin clots into liquid form.
2. Dextran 40 and sodium chloride are used as auxiliary agents.
Once in the blood, Gemaza quickly begins to have a thrombolytic effect. The main task of the drug is to stimulate the transformation of plasminogen into plasmin, which promotes rapid lysis of clots. After injection of Gemaza, the peak concentration of the substance in the eye area is reached after 2 hours.
Indications
The main purpose of the drug is auxiliary therapy of local hemorrhages in the eye area and eye tissues. Gemaza is widely used in ophthalmology.
For intravenous administration: occlusion of coronary vessels (acute myocardial infarction).
For administration subconjunctivally, parabulbarly, into the anterior chamber of the eye, intravitreally: hyphema, hemophthalmos; preretinal, subretinal and intraretinal hemorrhages; fibrinoid syndrome of various origins; occlusion of the central retinal artery and its branches; thrombosis of the central retinal vein and its branches; prevention of adhesions in the postoperative period during antiglaucoma operations.
Medical treatment of age-related macular degeneration, diabetic macular edema, retinal vascular diseases, intraocular hemorrhages, inflammation of the inner membranes of the eyeball using intravitreal injections (Lucentis, Eylea, Gemaza) is carried out under the program of the Territorial Compulsory Insurance Fund of Sevastopol (TFIF) - free of charge.
To make an appointment with a doctor, please contact the Medical Registration Office.
Sevastopol, st. Novorossiyskaya, 43A
Mobile tel.+7(978)202-53-70 Daily 8:00-17:00 Saturday, Sunday - closed
PATIENT NOTE:
- Memo Preoperative preparation for surgery
- Memo List of tests and examinations
- Issues of optimizing treatment with Gemaza for patients with combined fundus pathology in type 2 diabetes mellitus
Possible complications of intravitreal injections
The likelihood of complications after intravitreal injections is low; in any case, the risk is orders of magnitude lower than the benefit brought by targeted administration of drugs directly into the desired area. However, in some cases, either immediately after the intervention or in the long-term period, the following undesirable effects and complications, including very serious ones, may develop:
- retinal detachment;
- formation of synechiae (adhesions);
- increased intraocular pressure;
- “triggering” the development of cataracts;
- subluxation of the lens;
- endophthalmitis;
- uveitis
How does the procedure work?
In terms of their effectiveness, inravitreal injections are comparable to some types of vitreoretinal operations. The procedure requires sterile conditions and therefore must be performed in a specially equipped suitable room, such as an operating room. To perform injections into the eyeball, local anesthesia is used with eye drops, in order to avoid complications, the patient is prescribed antiseptics.
During the administration of the drug into the eye cavity, an anesthesiologist is present in the operating room, who monitors the patient’s vital functions and ensures the proper level of pain relief for the patient. The requirements for asepsis and antisepsis during intravitreal injection manipulation are the same as when performing vitreoretinal surgery and must comply with international standards for intraocular surgical interventions.
At the initial stage, the patient's eyeball is fixed using an eyelid expander, after which the doctor marks the area for future intraocular injection in the lower outer quadrant of the eyeball, 3.5 mm from the limbus. This allows the doctor to avoid future trauma to intraocular structures (lens, ciliary body, retina) and reduce the likelihood of intraocular complications. The drug is injected directly into the vitreous body of the eye through the outer membranes of the eye; for this purpose, special needles are used to prevent the drug from leaking out when the needle is removed. Due to the fact that the manipulation is carried out using an operating microscope, the doctor controls the process of drug administration and the depth of needle insertion. All of the above points make the procedure safe and minimize the risks of complications. Equally important is strict adherence to the recommendations of the attending physician in the postoperative period and regular postoperative monitoring.
Our clinic is equipped with the most modern equipment; we provide European-level services without queues and at affordable prices. When performing medical procedures, our specialists use the best equipment available today, including disposable instruments.
Intravitreal administration of Lucentis
The drug Lucentis was originally developed for use in ophthalmology, so it is characterized by high and targeted effectiveness. It is prescribed to eliminate the consequences of age-related degenerative processes in the macula, as well as to treat retinal edema in diabetes and venous occlusion. Prevents the formation and suppresses the proliferation of new vascular networks, normalizes the thickness of the retinal layer. When administered intravitreally, it quickly penetrates into the affected areas, localizes and relieves swelling and, in general, provides truly etiopathogenetic (aimed at eliminating the causes) treatment.
Lucentis injections are prescribed only after a thorough and comprehensive examination using computerized diagnostic equipment. The scheme is always strictly individual; in most cases, three injections are prescribed with an interval of one month, however, it should be borne in mind that treatment with Lucentis involves constant monitoring of the dynamics and assessment of the stability of the achieved effect, as well as the general functional state of the visual organs, so adjustments may be made to the prescriptions. In addition, regular examinations by the treating ophthalmologist are required over the next year.
The latest and almost irreplaceable diagnostic tool in such cases are optical coherence tomographs (for example, RTVue-100 made in the USA). Such equipment is capable of displaying fundus structures in both flat and stereoscopic, volumetric modes, featuring high performance, image quality, and speed of computer data analysis.
Intravitreal injection of the drug Ozurdex
An injection of the drug Ozurdex is actually an implantation of the glucocorticosteroid dexamethasone, i.e. creation of a certain depot (reserve) of the active substance, which is gradually, over several months, consumed in the desired area of the intraocular space. Ozurdex is prescribed mainly for macular edema that develops as a result of venous or capillary occlusion (blockage) against the background of atherosclerosis and/or systemic hypertension.
Dexamethasone is a substance with a multifaceted effect. The injection prevents the proliferation of blood vessels and reduces the permeability of their walls, eliminates inflammation and relieves swelling.
The instructions emphasize that implantation of Ozurdex should only be performed by an experienced, highly qualified ophthalmologist. As a rule, a single injection into the affected eye is prescribed. In isolated cases, when, as a paradoxical reaction, visual acuity is slightly reduced, or if the risk/benefit ratio is significantly shifted towards clinical need, a repeat injection may be prescribed. If vision and the general condition of the intraocular structures improve after the first injection, there is no need for a repeat procedure.
The total duration of the prolonged effect from intravitreal injection of Ozurdex reaches six months.
Injection techniques in ophthalmology
Injection algorithm
1. Comprehensive diagnostics
The decision to use injections is made based on the results of a comprehensive diagnosis by an ophthalmologist, which includes:
- Consultation with an ophthalmologist;
- Physical examination;
- Taking anamnesis;
- Visometry (visual acuity test);
- Skiascopy (determination of eye refraction);
- Ophthalmoscopy (examination of the fundus of the eye);
- Autorefractometry (determination of the optical power of the eye);
- Biomicroscopy (examination using a slit lamp).
The cost of comprehensive diagnostics is 6,000 tenge.
2. The procedure itself
- Before the procedure, a local allergy test is performed for anesthetics (painkillers) and, in the case of anti-inflammatory therapy, for antibiotics.
- The injection area is carefully treated with a disinfectant.
- If the injection is administered into the temporal region, then an anesthetic cream is first applied to the skin of the temple. In the case of subocular and subconjunctival injections, an anesthetic is administered along with the drug.
- If the injection is performed on the right eye, the patient should look up to the left and vice versa.
- The injection is administered using an insulin syringe into the selected area to a depth of about 10 mm. The length of the insulin needle itself is 13 mm. This stage takes no more than 2 minutes.
- After removing the needle, the injection site is pressed intermittently with an alcohol swab for several minutes.
The whole procedure does not take much time and lasts on average 5-10 minutes, including all preparation. The full course of treatment consists of 7-10 daily procedures.
Important: Each procedure is carried out under 100% sterility conditions and in accordance with international protocols. All consumables are disposable and are unpacked in front of the patient. The doctor performs the procedure in a sterile disposable gown, mask, gloves and cap.
As a rule, intravitreal injections are part of a comprehensive treatment program, which may also include physiotherapeutic procedures (ALMAG and Darsonval) and drug therapy. During the treatment process, the patient is given the entire necessary package of drugs from the On Clinic personal drug bank. The doctor outlines a personal treatment plan for the patient, down to the daily routine and exercise, taking into account his individual characteristics. After completing the course, the patient can be observed by his treating doctor for free for a year.
Intravitreal injection of Gemaza
Gemaza is another specialized, purely ophthalmic drug that has a pronounced thrombo- and fibrinolytic effect. Gemaza can be prescribed for any (sub-, intra-, pre-) retinal hemorrhages, for occlusions of the central retinal artery and venous thrombosis, for extensive hemorrhages in the anterior chamber of the eye and vitreous body, as well as for the prevention of adhesions after ophthalmic surgical interventions (for example , in connection with glaucoma).
Gemaza can be combined within the same therapeutic regimen with dexamethasone and emoxypine.
Intravitreal antibiotic injection
As is known, antibiotic substances are prescribed to inhibit (suppress) infectious and inflammatory processes caused by pathogenic bacteria. The correct choice and dosage of an antibiotic is a whole science, or at least a methodology that requires a thorough understanding of the mechanisms of what is happening and precise adherence to calculation algorithms. The volume and concentration of the active substance must be, on the one hand, sufficient for the total destruction of the pathogen (therefore, the intensity of the inflammatory process is one of the most important among numerous factors taken into account, along with the general immune status of the patient, the presence of an allergic history, etc.), and on the other hand, do not exceed the permissible level of toxic damage to cells and tissues.
In the case of antibiotic therapy, the injection procedure is somewhat modified and more complicated. With a standard puncture, first of all, material is selected for laboratory microbiological culture and analysis (microscopic volume of the vitreous body, not exceeding 0.1 ml), then the syringe is replaced and a similar volume of antibiotic solution is injected through the same needle (most often a broad-spectrum antibiotic is used ), after which the needle is withdrawn.
As a rule, the effective concentration of the antibiotic in the vitreous remains for up to three days; This is taken into account when setting the date for the next injection.
It is important to consider that the maximum antibiotic effect is achieved at the very first, acute stage of development of the infectious-inflammatory process; at subsequent stages, the predicted effect decreases until intravitreal injection of the antibiotic is inappropriate.