The Ministry of Health of the Russian Federation regulated the procedure for admitting children to preschool institutions. A medical examination is mandatory for all children. To do this, a card is created for each child, where specialists put their marks and there is a pediatrician’s conclusion about the possibility of attending kindergarten. The medical record is form 026/у-2000. In public clinics, medical examinations are carried out free of charge. Parents must have their own passport, child’s birth certificate and compulsory medical insurance policy. You can also contact specialized children's private medical centers and undergo a commission to enter a kindergarten for a fee.
Laboratory research
First of all, you should make an appointment with a pediatrician at your place of residence. After a preliminary examination of the child, the doctor fills out the cover page of the medical record, and also indicates a complete list of tests and specialists that will need to be completed.
From laboratory tests, children are prescribed:
- Complete blood count (CBC). It gives an assessment of your overall health, as it can help identify many diseases. This is the most common diagnostic procedure, especially in pediatrics, where a small child often cannot pinpoint what is bothering him. OAC in children is taken on an empty stomach in the morning. Blood is taken from a finger or from a vein; the first option is used more often. Indicators of this analysis in children may differ greatly from similar indicators in adults.
- Blood sugar test. Also taken in the morning on an empty stomach.
- General urine analysis. Urine is collected only in the morning, immediately before going to the clinic. Before doing this, it is important to wash the child thoroughly to avoid detecting protein in the urine. To obtain the most accurate result, you should collect an average portion of the first morning urine.
- Feces for worm eggs. It’s good if you can collect it in the morning, but it is quite acceptable to do this during the previous day.
- Scraping for worm eggs. The material is collected at the clinic by a nurse.
- ECG - electrocardiogram.
All of the above tests are carried out very quickly, usually by the end of the working day the results are already known.
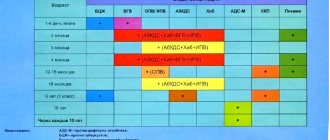
National vaccination calendar
Downloads
Calendar of preventive vaccinations for children from 0 to 18 years old (202.16 Kb)To download the file, use the built-in capabilities of your browser. The PDF file can be read using a free program or built-in browser tools
Additional materials
Vaccination calendar: the Russian path against the backdrop of global experience
The national vaccination calendar is a document approved by order of the Ministry of Health of the Russian Federation, which determines the timing and types of vaccinations (preventive vaccinations) carried out free of charge and on a large scale in accordance with the compulsory health insurance program (CHI).
The vaccination calendar is developed taking into account all age-related characteristics, including the most dangerous infectious diseases in children in the first year of life. Vaccinations, which are given as part of the National Calendar, can significantly reduce the risk of disease in children. And if the child does get sick, then the vaccination given will contribute to the progression of the disease in a milder form and will relieve serious complications, many of which are extremely life-threatening.
The national vaccination calendar is a system for the most rational use of vaccines, ensuring the development of intense immunity at the earliest (vulnerable) age in the shortest possible time. The vaccination calendar can be divided into two parts.
The first part is the National Calendar of Preventive Vaccinations, which provides vaccination against widespread infections that affect almost the entire human population (airborne infections - measles, rubella, mumps, whooping cough, chickenpox, diphtheria, influenza), as well as infections that are characterized by severe course with high mortality (tuberculosis, hepatitis B, diphtheria, tetanus, polio, hemophilus influenzae type b).
The second part is vaccinations for epidemic indications - against natural focal infections (tick-borne encephalitis, leptospirosis, etc.) and zoonotic infections (brucellosis, tularemia, anthrax). This category may also include vaccinations carried out in risk groups - persons with both a high possibility of infection and a high danger to others in the event of their illness (such diseases include hepatitis A, typhoid fever, cholera).
The national calendar is an authoritative source of information that will help parents figure out what diseases they can protect their child from, and when it is best to do this.
Today, more than 1.5 thousand infectious diseases are known in the world, but people have learned to prevent only the 30 most dangerous infections with the help of preventive vaccinations. Of these, 12 infections, which are the most dangerous (including due to their complications) and which easily affect children all over the world, are included in the National Calendar of Preventive Vaccinations of Russia. Another 16 from the list of dangerous diseases are included in the National Vaccination Calendar for epidemic indications.
Number of preventable diseases around the world and diseases included in the mandatory National Vaccination Schedules of different countries
Basic Vaccination Calendars and Calendars for Epidemiological Indications
Each WHO member country has its own vaccination schedule. The Russian national vaccination calendar is not fundamentally different from the national vaccination calendars of developed countries. True, some of them provide for vaccinations against hepatitis A, meningococcal infection, human papillomavirus, rotavirus infection (for example, in the USA). Thus, for example, the US national vaccination calendar is more saturated than the Russian calendar. The vaccination calendar in our country is expanding - for example, since 2015, it has included vaccination against pneumococcal infection.
On the other hand, in some countries, the National Calendar does not provide for vaccination against tuberculosis, which in our country is forced by the high incidence of this infection. And to this day, vaccination against tuberculosis is included in the vaccination schedule of more than 100 countries, while many provide for its implementation in the first days after birth, as recommended by the WHO Vaccination Schedule.
National vaccination calendars of different countries
| Infections | Russia | USA | Great Britain | Germany | Number of countries using vaccine in NK |
| Tuberculosis | + | more than 100 | |||
| Diphtheria | + | + | + | + | 194 |
| Tetanus | + | + | + | + | 194 |
| Whooping cough | + | + | + | + | 194 |
| Measles | + | + | + | + | 111 |
| Flu | + | + | + | + | |
| Haemophilus influenzae type b/Hib infection | + (risk groups) | + | + | + | 189 |
| Rubella | + | + | + | + | 137 |
| Hepatitis A | + | ||||
| Hepatitis B | + | + | + | 183 | |
| Polio | + | + | + | + | all countries |
| Mumps | + | + | + | + | 120 |
| Chicken pox | + | + | |||
| Pneumococcus | Since 2015 | + | + | + | 153 |
| Human papillomavirus / CC | + | + | + | 62 | |
| Rotavirus infection | + | 75 | |||
| Meningococcal infection | + | + | + | ||
| Total infections | 12 | 16 | 12 | 14 | |
| Number of injections administered up to 2 years | 14 | 13 | 11 |
In Russia , the National Calendar is less saturated than the vaccination calendars of countries such as the USA and a number of European countries:
- there are no vaccinations against rotavirus infection, HPV, chickenpox;
- vaccinations against Hib are carried out only in risk groups, hepatitis A - according to epidemiological indications;
- there is no 2nd revaccination against whooping cough;
- Combination vaccines are underused.
Order of the Ministry of Health of the Russian Federation dated March 21, 2014 No. 125n “On approval of the national calendar of preventive vaccinations and the calendar of preventive vaccinations for epidemic indications
Registered with the Ministry of Justice of the Russian Federation on April 25, 2014. Registration No. 32115 Published: May 16, 2014 in “RG” - Federal issue No. 6381.
National calendar of preventive vaccinations
| Categories and ages of citizens subject to mandatory vaccination | Name of preventive vaccination |
| Newborns in the first 24 hours of life | First vaccination against viral hepatitis B The first, second and third vaccinations are carried out according to the 0-1-6 scheme (1 dose - at the start of vaccination, 2 dose - a month after 1 vaccination, 3 dose - 6 months after the start of vaccination), for with the exception of children belonging to risk groups, vaccination against viral hepatitis B is carried out according to the 0-1-2-12 scheme (1 dose - at the start of vaccination, 2 dose - a month after 1 vaccination, 2 dose - 2 months from the start vaccination, 3rd dose - 12 months from the start of vaccination). |
| Newborns on the 3rd - 7th day of life | Vaccination against tuberculosis Vaccination is carried out with a vaccine for the prevention of tuberculosis for gentle primary vaccination (BCG-M); in constituent entities of the Russian Federation with incidence rates exceeding 80 per 100 thousand population, as well as in the presence of tuberculosis patients around the newborn - the vaccine for the prevention of tuberculosis (BCG). |
| Children 1 month | Second vaccination against viral hepatitis B The first, second and third vaccinations are carried out according to the 0-1-6 scheme (1 dose - at the start of vaccination, 2 dose - a month after the 1st vaccination, 3 dose - 6 months after the start of vaccination), for with the exception of children belonging to risk groups, vaccination against viral hepatitis B is carried out according to the 0-1-2-12 scheme (1 dose - at the start of vaccination, 2 dose - a month after 1 vaccination, 2 dose - 2 months from the start vaccination, 3rd dose - 12 months from the start of vaccination). |
| Children 2 months | Third vaccination against viral hepatitis B (risk groups) Vaccination is carried out for children belonging to risk groups (born from mothers who are carriers of HBsAg, patients with viral hepatitis B or who have had viral hepatitis B in the third trimester of pregnancy, who do not have test results for markers of hepatitis B, who consume narcotic drugs or psychotropic substances, from families in which there is a carrier of HBsAg or a patient with acute viral hepatitis B and chronic viral hepatitis). |
| First vaccination against pneumococcal infection | |
| Children 3 months | First vaccination against diphtheria, whooping cough, tetanus |
| First vaccination against polio The first and second vaccinations are carried out with a vaccine for the prevention of polio (inactivated). | |
| First vaccination against hemophilus influenzae infection (risk group) Vaccination is carried out for children belonging to risk groups (with immunodeficiency conditions or anatomical defects leading to a sharply increased risk of hemophilus influenzae infection; with oncohematological diseases and/or long-term recipients of immunosuppressive therapy; children born to mothers with HIV infection; children with HIV infection; children in orphanages). | |
| Children 4.5 months | Second vaccination against diphtheria, whooping cough, tetanus |
| Second vaccination against hemophilus influenzae infection (risk group) Vaccination is carried out for children belonging to risk groups (with immunodeficiency conditions or anatomical defects leading to a sharply increased risk of hemophilus influenzae infection; with oncohematological diseases and/or long-term recipients of immunosuppressive therapy; children born to mothers with HIV infection; children with HIV infection; children in orphanages). | |
| Second vaccination against polio The first and second vaccinations are carried out with a vaccine for the prevention of polio (inactivated). | |
| Second vaccination against pneumococcal infection | |
| Children 6 months | Third vaccination against diphtheria, whooping cough, tetanus |
| Third vaccination against viral hepatitis B The first, second and third vaccinations are carried out according to the 0-1-6 scheme (1 dose - at the start of vaccination, 2 dose - a month after the 1st vaccination, 3 dose - 6 months after the start of vaccination), for with the exception of children belonging to risk groups, vaccination against viral hepatitis B is carried out according to the 0-1-2-12 scheme (1 dose - at the start of vaccination, 2 dose - a month after 1 vaccination, 2 dose - 2 months from the start vaccination, 3rd dose - 12 months from the start of vaccination). | |
| Third vaccination against poliomyelitis The third vaccination and subsequent revaccinations against poliomyelitis are given to children with a vaccine for the prevention of poliomyelitis (live); children born to mothers with HIV infection, children with HIV infection, children in orphanages - a vaccine for the prevention of polio (inactivated). | |
| Third vaccination against hemophilus influenzae infection (risk group) Vaccination is carried out for children belonging to risk groups (with immunodeficiency conditions or anatomical defects leading to a sharply increased risk of hemophilus influenzae infection; with oncohematological diseases and/or long-term immunosuppressive therapy; children born to mothers with HIV infection; children with HIV infection; children in orphanages). | |
| Children 12 months | Vaccination against measles, rubella, mumps |
| Fourth vaccination against viral hepatitis B (risk groups) Vaccination is carried out for children belonging to risk groups (born from mothers who are carriers of HBsAg, patients with viral hepatitis B or who have had viral hepatitis B in the third trimester of pregnancy, who do not have test results for markers of hepatitis B, who consume narcotic drugs or psychotropic substances, from families in which there is a carrier of HBsAg or a patient with acute viral hepatitis B and chronic viral hepatitis). | |
| Children 15 months | Revaccination against pneumococcal infection |
| Children 18 months | The first revaccination against poliomyelitis The third vaccination and subsequent revaccinations against poliomyelitis are given to children with a vaccine for the prevention of poliomyelitis (live); children born to mothers with HIV infection, children with HIV infection, children in orphanages - a vaccine for the prevention of polio (inactivated). |
| First revaccination against diphtheria, whooping cough, tetanus | |
| Revaccination against Haemophilus influenzae infection (risk groups) | |
| Children 20 months | Second revaccination against poliomyelitis The third vaccination and subsequent revaccinations against poliomyelitis are given to children with a vaccine for the prevention of poliomyelitis (live); children born to mothers with HIV infection, children with HIV infection, children in orphanages - a vaccine for the prevention of polio (inactivated). |
| Children 6 years old | Revaccination against measles, rubella, mumps |
| Children 6 - 7 years old | The second revaccination against diphtheria, tetanus The second revaccination is carried out with toxoids with a reduced content of antigens. |
| Revaccination against tuberculosis Revaccination is carried out with a vaccine to prevent tuberculosis (BCG). | |
| Children 14 years old | The third revaccination against diphtheria, tetanus The second revaccination is carried out with toxoids with a reduced content of antigens. |
| The third revaccination against poliomyelitis The third vaccination and subsequent revaccinations against poliomyelitis are given to children with a vaccine for the prevention of poliomyelitis (live); children born to mothers with HIV infection, children with HIV infection, children in orphanages - a vaccine for the prevention of polio (inactivated). | |
| Adults over 18 years old | Revaccination against diphtheria, tetanus - every 10 years from the date of the last revaccination |
| Children from 1 year to 18 years old, adults from 18 to 55 years old, not previously vaccinated | Vaccination against viral hepatitis B Vaccination is carried out for children and adults who have not previously been vaccinated against viral hepatitis B, according to the 0-1-6 scheme (1 dose - at the start of vaccination, 2 dose - a month after 1 vaccination, 3 dose - after 6 months from the start of vaccination). |
| Children from 1 year to 18 years, women from 18 to 25 years (inclusive), not sick, not vaccinated, vaccinated once against rubella, who have no information about vaccinations against rubella | Vaccination against rubella |
| Children from 1 year to 18 years inclusive and adults under 35 years of age (inclusive), who have not been sick, not vaccinated, vaccinated once, and have no information about measles vaccinations | Vaccination against measles The interval between the first and second vaccinations should be at least 3 months |
| Children from 6 months, students in grades 1 - 11; students studying in professional educational organizations and educational organizations of higher education; adults working in certain professions and positions (employees of medical and educational organizations, transport, public utilities); pregnant women; adults over 60 years of age; persons subject to conscription for military service; people with chronic diseases, including lung disease, cardiovascular disease, metabolic disorders and obesity | Flu vaccination |
The child receives the first vaccinations according to the National Calendar in the maternity hospital - this is the very first vaccination against hepatitis B, which is given in the first hours of life. Often the first vaccination against tuberculosis is also carried out within the walls of the maternity hospital. Before one year of age, children are vaccinated against hemophilus influenzae, whooping cough, polio, diphtheria, tetanus, and pneumococcal infection. From the age of six months, you can vaccinate your child against influenza. Older children, at the age of 12 months, receive protection against measles, rubella, and mumps through vaccinations.
Vaccinations with polysaccharide vaccines (Pneumo23, meningococcal vaccine, etc.) should begin after 2 years of age, since the child’s body does not respond by producing antibodies to these antigens. For younger children, conjugate vaccines (polysaccharide with protein) are recommended.
Examination by specialists
The speed at which doctors pass through depends on the medical institution. In the process of passing a medical commission to a kindergarten, you need to visit the following specialists:
- Dermatologist. This is a doctor specializing in skin diseases. People visit him for problems with nails, hair, and mucous membranes. A dermatologist examines the child’s skin for rashes and lesions. If something is detected, the cause of the disease is determined. If the disease is not contagious, the child can attend kindergarten and undergo treatment at the same time. If the disease is contagious, then visiting a preschool institution will have to be postponed.
- ENT. This specialist examines the child's ears, nose and throat and tests his hearing. Some pathological processes occur in children completely asymptomatically and can only be detected upon examination. For example, these are sulfur plugs. They do not create discomfort, but contribute to hearing loss.
- Oculist. There are many reasons why visual acuity decreases. It is important to identify them as soon as possible and begin correction.
- Dentist. During this period, the child's baby teeth are actively growing. The doctor must examine the correctness of their location and general condition. In addition, the frenulum of the lips and tongue deserves special attention; the development of a child’s speech directly depends on them.
- Neuropathologist. The state of the nervous system, vestibular apparatus, and general psycho-emotional state should be assessed by this specialist. There are also many hidden pathologies in this area that parents may not even be aware of. As the child grows up, they can manifest themselves and become obvious, and then, as they progress, reduce the quality of life of the baby.
- Orthopedist. The doctor can determine poor posture and flat feet. At this stage of a child’s life, it is necessary to engage in correction if violations are detected.
- Surgeon. Often this specialist combines two functions at once - a surgeon and a urologist-andrologist for examining boys. All children are checked for the presence/absence of a hernia. In boys, the genitals are additionally checked.
- Gynecologist. Only girls are referred to this specialist for examination of the genital organs. It is believed that you should definitely visit a doctor before going to kindergarten.
- Speech therapist. This is a doctor who specializes in speech formation; all children over 3 years of age are referred to him. Speech development depends on many factors. Often a speech therapist has to work together with a neurologist, psychiatrist, and dentist. If a child is diagnosed with any speech disorder or delayed speech development, the most important thing is to quickly and accurately determine the cause. The sooner you start working on eliminating it, the more successful the treatment will be.
As the commission proceeds to the kindergarten, specialists may prescribe additional studies. This is done to study the problem in more detail, make an accurate diagnosis and select appropriate treatment.
Vaccination record
If parents vaccinate their child according to the existing schedule, this makes obtaining a medical card to attend kindergarten much easier. According to the rules for filling out the card, all data on vaccinations performed must be entered into the document.
In the event of an unfavorable epidemiological situation due to some disease for which the child is not vaccinated, he may be temporarily denied access to a child care facility.
It is important to obtain permission from a TB doctor. This specialist will issue a conclusion only if there is a fresh Mantoux reaction. If the parents refuse this, an alternative option is an x-ray of the child’s chest.
After going through all the doctors, taking tests and settling the issue with vaccinations, you should visit the pediatrician again. He signs the medical card and issues a certificate of the child’s health. Based on this, you can begin visiting a preschool institution.
At the First Children's Medical Center you can undergo a medical examination for kindergarten at a competitive price. The center's highly qualified specialists have extensive experience working with children. The center guarantees a high level of medical care.
How are children vaccinated?
A child can be vaccinated only with the consent of the parents. The absence of punishment for refusing vaccination does not relieve the father/mother of responsibility for the health of their baby. It is worth assessing all the risks and taking into account that trips to other countries require vaccination; the list of mandatory vaccinations is specified when applying for a visa.
Vaccination is carried out in public and private medical institutions. The Miracle Doctor clinic has permission to vaccinate children. Our doctors use vaccines approved for use in Russia and strictly follow the rules for storing immune preparations. The vaccination calendar can be adjusted individually, taking into account completed/deferred vaccinations and the child’s health status. The availability of various combined vaccines allows you to safely vaccinate your baby against several diseases at once.
First, the doctor talks with the parents, explaining all the points they are interested in regarding vaccination. A friendly atmosphere has been created in pediatricians' offices, so children react more calmly to vaccinations. A doctor’s appointment, supplemented with game elements, builds confidence in children and relieves them of the fear of an injection. Parents can bring their child's favorite toy to the appointment. When communicating with teenagers, openness and ease are important; information about vaccinations is presented in an accessible form.
Important! Paid vaccination in a private medical center allows you to vaccinate your child with a drug that is not available in public clinics. Communication with the doctor and the injection itself will not cause stress for the child, and parents will be confident in the quality and safety of the drug.
Depending on the type of vaccination, the injection is given intramuscularly (in the thigh for children under 2 years old, in the shoulder for children over 2 years old), intradermal (for example, BCG) or subcutaneously (against measles, rubella, etc.). Some vaccines are given orally (polio oral drops) or intranasally (flu nasal drops).
The adult places his small child on his lap in a “cuddling position.” This way the baby feels protected and worries less, and the injection site is accessible to the doctor. Medical staff in vaccination rooms wear disposable gloves. Before directly administering the vaccine, the nurse/paramedic checks the vial with the vaccine: whether the drug corresponds to the prescribed vaccination, the expiration date and the tightness of the packaging. After vaccination, doctors recommend staying at the clinic for 30 minutes so that in exceptional cases of rapid development of an allergic reaction, the necessary assistance can be provided in a timely manner.