Vaccination for children today is considered the only proven way to protect against serious infections. WHO research statistics confirm a significant decline in the number of reported cases of many diseases. For example, today there are already 2 cases of paralytic poliomyelitis considered an emergency. Previously, about 7,700 cases were registered in Europe every year. Today, thanks to vaccinations, smallpox has been completely defeated, the last case of which was registered in 1978. The incidence of diphtheria has decreased by 90%. According to WHO, from 2000 to 2015, measles vaccines saved about 20 million lives.
Vaccination of children: pros and cons
The debate between supporters and opponents of vaccines began in 1998, when Dr. Andrew Wakefield published his research in the American medical journal The Lancet. In it, he claimed that children develop autism after receiving the mumps, measles and rubella vaccine. Dr. Wakefield supported his conclusions with the results of observations of 12 patients. However, medical journalist Brian Dear decided to meet with the parents of the observed children. It turned out that three had been diagnosed with autism before vaccination, and another five already had other neurological problems. As a result, it was possible to find out that Dr. Wakefield, before his research, developed and patented a monovaccine against measles. He recommended it instead of the drug used, which helped protect against three diseases at once. Wakefield's article was refuted, but public doubts were never completely dispelled.
Modern opponents of vaccinations cite as one of their arguments the presence of a mercury-based preservative in vaccines, which allegedly causes autism in children. However, the use of this component has been prohibited in the United States since 2002. However, the number of cases of autism is not decreasing. In 2014, Australian scientists examined the medical records of more than a million children belonging to different age groups. It turned out that there is no connection between mercury preservatives and cases of autism.
What may be contraindications for vaccinations?
Modern vaccines are of very high quality and safe. But children, regardless of age, should carefully prepare for their introduction. The following main contraindications exist:
| Vaccine | Contraindications |
| All vaccinations | Swelling at the injection site more than 8 centimeters in diameter, temperature above 40°C and other severe complications after previous vaccinations |
| DTP | History of afebrile seizures and other progressive nervous system disorders |
| All vaccinations with live vaccines | Malignant diseases, immunodeficiency, immunosuppression |
| BCG, BCG-M | Presence of a keloid scar, weight less than 2 kg at birth |
| Hepatitis B | Yeast allergy |
| Flu | Severe allergic reactions to chicken egg white |
| All vaccinations with vaccines against rubella, mumps, measles; double vaccines (mumps-measles); triple vaccines (rubella-measles-mumps) | Allergy to aminoglycosides. For all mumps and measles vaccinations - anaphylactic reaction to chicken egg white |
If a child from birth, up to one year, or at another age has these contraindications, the doctor must select another suitable vaccine, or give a waiver from vaccinations. A deferment from vaccination is given when there are infectious and non-infectious diseases, as well as exacerbations of chronic diseases. If there are intestinal infections or mild acute respiratory viral infections, all vaccinations can be administered after stool and temperature have normalized. When chronic and other diseases are weakened, vaccination is carried out after 2-4 weeks.
Vaccination calendar for children under one year old
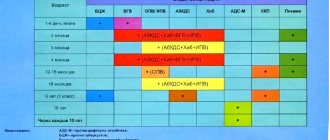
The vaccination calendar for children under one year of age is the period approved by the Russian Ministry of Health for mandatory vaccines (Table 1).
Table 1. Vaccination schedule for children under 1 year of age, according to the National Preventive Vaccination Calendar.
| Infection | Child's age | ||||||||
| First 24 hours | 3–5 days | 1 month | 2 months | 3 months | 4.5 months | 6 months | 9 months | 12 months | |
| Viral hepatitis B | B1 | B2 | B3 | ||||||
| B1 | B2 | B3 | B4 | ||||||
| Tuberculosis | B | ||||||||
| Whooping cough | B1* | B2* | B3* | ||||||
| Diphtheria | |||||||||
| Tetanus | |||||||||
| Polio | B1* IPV | B2*IPV | B3*IPV | ||||||
| Haemophilus influenzae infection | B1* | B2* | B3* | ||||||
| Measles | B1* | ||||||||
| Rubella | |||||||||
| Parotitis | |||||||||
| Pneumococcal infection | B1 | B2 | |||||||
| Flu | B | ||||||||
Legend:
- B1, B2, B3, B4, — serial number of vaccination;
- B - all children of this age group;
- B - children from risk groups, according to indications;
- * - mainly as part of combined vaccines;
- IPV—inactivated polio vaccine;
- OPV - oral polio vaccine.
In a number of countries, the national calendar for children under one year of age includes vaccinations against rotavirus infection and meningococcus, and after one year - against chickenpox, hepatitis A, tick-borne encephalitis, and HPV (human papillomavirus). In Russia, these infections are not yet subject to mandatory immunoprophylaxis, although the Union of Pediatricians of Russia recommends them.
The national vaccination calendar for up to a year includes the minimum number of vaccinations required to protect against dangerous infections. If children have certain conditions and parents wish, additional vaccinations may be given.
What parents need to know about the vaccination procedure
All vaccinations must be done according to certain rules under the supervision of a doctor. You should prepare for vaccination every time. To ensure that the baby is healthy before the start of the vaccination cycle at 3 months, blood and urine tests are ordered a few days before the first vaccination. If everything is normal, before the procedure the child’s temperature is measured and examined by a doctor. Particular attention is paid to the presence of allergic manifestations. If they are present, after vaccination, antihistamines are prescribed on the recommendation of a doctor. It is also advisable to give the child an antipyretic in the evening on the day of vaccination.
Before vaccination, the doctor must tell parents in detail about possible side effects and their elimination. At the same time, mom or dad should understand when symptoms after vaccination are not dangerous and can be dealt with using available means, and when it is worth seeking help. After consultation on all age-appropriate vaccinations has been received, parents sign consent to them. Unfortunately, in local clinics the matter is often limited to a signature.
The ampoule with the vaccine for children is removed from the package in the presence of parents. They may also ask you to inspect it for cracks. You must be in or near the clinic for 30 minutes after the procedure. This is a precautionary measure in case of an allergic reaction. It is better to be in the air, because crowds of people and various infections in the air can cause side effects.
How children are vaccinated
Guided by the calendar, the local pediatrician checks the baby’s condition before each procedure. The decision to carry out the next procedure is made based on the results of the examination. The baby's reaction to previously administered vaccinations is also analyzed. If detected:
- vaccine side effects and complications;
- inflammation at the injection site;
- fever in infants after vaccination;
- any uncharacteristic consequences of performing procedures,
The vaccination schedule is being reviewed, shifted, and monitoring continues. Diagnosis of allergic reactions requires the additional involvement of an immunologist in observation. The reason for the transfer may be a complication of the epidemiological situation.
Although, in the context of the 2021 coronavirus pandemic, WHO and US CDC specialists answer in the affirmative when asked whether infants are vaccinated during quarantine. Ideally, only a normal reaction of the child can become the basis for scheduling vaccinations. Consultation with a specialist is necessary.
How do children cope with vaccination?
You need to understand what infants are vaccinated against. Vaccination is intended to help control the spread of disease across the country, not to protect the individual newborn. It is clear that the human body reacts to the vaccine individually, which complicates the task. Today, complications after vaccinations are much less common, but they do happen. After vaccination, children may experience:
- swelling, redness, suppuration at the injection site;
- heat;
- allergic reactions of varying severity.
To prepare for the unexpected, we recommend:
- Avoid vaccination if you have dermatitis, runny nose, or fever;
- postpone the procedure if the child has been in contact with sick people;
- two to three days before the procedure, give the baby antihistamines if he has confirmed allergies;
- keep antipyretic and antiallergic medications at home.
Restoring the vaccination schedule
In case of violation of the vaccination schedule, the specialists of the myMedicus clinic offer the patient to develop an individual schedule of vaccinations for children. The pediatrician draws up a vaccination plan for children, taking into account the characteristics of the immunobiological drug. The standard vaccination schedule is also taken into account. Immunoprophylaxis of a patient with immune diseases and HIV is carried out in a special manner. It uses inactivated vaccines or recombinant drugs that replace the pathogenic protein.
Rubella vaccine
This disease, which usually occurs in childhood, leaves behind a strong immunity.
A red rash appears on the child’s body (where, in fact, the disease got its name). Rubella is also fraught with serious complications - meningitis, eye damage, etc. If a pregnant woman (who did not have it in childhood and was not vaccinated in adolescence) gets rubella, then there is a serious risk of developing congenital deformities in the fetus. Despite the fact that maternal rubella poses a danger to the unborn child only in the first three, maximum four months of pregnancy.
The procedure for vaccination, explanation of the need for measures
When carrying out any vaccination it is necessary:
- to avoid complications, be healthy and have no contact with infectious diseases in the family, which is why a doctor’s examination is necessary before vaccination;
- When undergoing vaccination, it is necessary to first undergo a clinical blood test and a general urine test to clarify the state of health.
Observation after vaccination is carried out by a doctor for 30-40 minutes because It is known that it is during these periods that the most dangerous complications of vaccination can appear - anaphylactic shock, Quincke's edema, edema of the upper respiratory tract - therapy for which should begin immediately.
However, I would like to remind you that complications after vaccination, according to WHO (World Health Organization), are significantly less than when using, for example, drugs such as ANALGIN and ASPIRIN.
MAKE AN APPOINTMENT PRICES
Calendar of preventive vaccinations for epidemic indications
With changes and additions from: June 16, 2021, April 13, 2017, February 19, 2021.
| Name of preventive vaccination | Categories of citizens subject to mandatory vaccination |
| Against tularemia | Persons living in territories enzootic for tularemia, as well as persons arriving in these territories performing the following work: - agricultural, drainage, construction, other work on excavation and movement of soil, procurement, fishing, geological, survey, expedition, deratization and disinfestation; — logging, clearing and landscaping of forests, health and recreation areas for the population. Persons working with live cultures of the causative agent of tularemia. |
| Against the plague | Persons living in areas enzootic for plague. Persons working with live cultures of the plague pathogen. |
| Against brucellosis | In foci of goat-sheep type brucellosis, persons performing the following work: - procurement, storage, processing of raw materials and livestock products obtained from farms where livestock diseases with brucellosis are registered; — for the slaughter of livestock suffering from brucellosis, the procurement and processing of meat and meat products obtained from it. Livestock breeders, veterinarians, livestock specialists in farms enzootic for brucellosis. Persons working with live cultures of the causative agent of brucellosis. |
| Against anthrax | Persons performing the following work: - livestock workers and other persons professionally engaged in pre-slaughter livestock maintenance, as well as slaughter, skinning and cutting of carcasses; — collection, storage, transportation and primary processing of raw materials of animal origin; - agricultural, drainage, construction, excavation and movement of soil, procurement, fishing, geological, survey, expedition in anthrax-enzootic territories. Persons working with material suspected of being infected with anthrax. |
| Against rabies | For preventive purposes, people who have a high risk of contracting rabies are vaccinated: people working with the “street” rabies virus; veterinary workers; huntsmen, hunters, foresters; persons performing work on catching and keeping animals. |
| Against leptospirosis | Persons performing the following work: - procurement, storage, processing of raw materials and livestock products obtained from farms located in areas enzootic for leptospirosis; — for the slaughter of livestock with leptospirosis, the procurement and processing of meat and meat products obtained from animals with leptospirosis; - on catching and keeping stray animals. Persons working with live cultures of the causative agent of leptospirosis. |
| Against tick-borne viral encephalitis | Persons living in areas where tick-borne viral encephalitis is endemic; persons traveling to areas endemic for tick-borne viral encephalitis, as well as persons arriving in these territories performing the following work: - agricultural, irrigation, construction, excavation and movement of soil, procurement, fishing, geological, survey, expedition, deratization and disinfestation; — logging, clearing and landscaping of forests, health and recreation areas for the population. Persons working with live cultures of tick-borne encephalitis. |
| Against Q fever | Persons performing work on the procurement, storage, processing of raw materials and livestock products obtained from farms where Q fever diseases are registered. Persons performing work on the procurement, storage and processing of agricultural products in enzootic areas with Q fever. Persons working with live cultures of Q fever pathogens. |
| Against yellow fever | Persons traveling outside the Russian Federation to countries (regions) enzootic for yellow fever. Persons working with live cultures of the yellow fever pathogen. |
| Against cholera | Persons traveling to cholera-prone countries (regions). The population of the constituent entities of the Russian Federation in the event of complications of the sanitary and epidemiological situation regarding cholera in neighboring countries, as well as on the territory of the Russian Federation. |
| Against typhoid fever | Persons engaged in the field of municipal improvement (workers servicing sewer networks, structures and equipment, as well as organizations carrying out sanitary cleaning of populated areas, collection, transportation and disposal of household waste). Persons working with live cultures of typhoid pathogens. Population living in areas with chronic water epidemics of typhoid fever. Persons traveling to hyperendemic countries (regions) for typhoid fever. Contact persons in areas of typhoid fever for epidemic indications. According to epidemic indications, vaccinations are carried out when there is a threat of an epidemic or outbreak (natural disasters, major accidents in the water supply and sewerage networks), as well as during an epidemic, while mass vaccination of the population is carried out in the threatened region. |
| Against viral hepatitis A | Persons living in regions disadvantaged by the incidence of hepatitis A, as well as persons at occupational risk of infection (medical workers, public service workers employed in food industry enterprises, as well as those servicing water supply and sewerage facilities, equipment and networks). Persons traveling to disadvantaged countries (regions) where outbreaks of hepatitis A are registered. Contact persons in hepatitis A outbreaks. |
| Against shigellosis | Employees of medical organizations (their structural divisions) with an infectious disease profile. Persons engaged in the field of public catering and municipal improvement. Children attending preschool educational organizations and going to organizations providing treatment, rehabilitation and (or) recreation (as indicated). According to epidemic indications, vaccinations are carried out when there is a threat of an epidemic or outbreak (natural disasters, major accidents in the water supply and sewerage networks), as well as during an epidemic, while mass vaccination of the population is carried out in the threatened region. Preventive vaccinations are preferably carried out before the seasonal increase in the incidence of shigellosis. |
| Against meningococcal infection | Children and adults in areas of meningococcal infection caused by meningococcal serogroups A or C. Vaccination is carried out in endemic regions, as well as in the event of an epidemic caused by meningococcal serogroups A or C. Persons subject to conscription for military service. |
| Against measles | Contact persons without age restrictions from the outbreaks of the disease, who have not previously been ill, have not been vaccinated and do not have information about preventive vaccinations against measles or have been vaccinated once. |
| Against viral hepatitis B | Contact persons from the outbreaks of the disease who have not been sick, have not been vaccinated and do not have information about preventive vaccinations against viral hepatitis B. |
| Against diphtheria | Contact persons from the outbreaks of the disease who have not been sick, have not been vaccinated and do not have information about preventive vaccinations against diphtheria. |
| Against mumps | Contact persons from the foci of the disease who have not been sick, have not been vaccinated and do not have information about preventive vaccinations against mumps. |
| Against polio | Contact persons in foci of polio, including those caused by wild poliovirus (or if the disease is suspected): - children from 3 months to 18 years - once; - medical workers - once; - children arriving from polio-endemic (polio-affected) countries (regions), from 3 months to 15 years - once (if there is reliable data on previous vaccinations) or three times (if they are absent); - persons without a fixed place of residence (if identified) from 3 months to 15 years - once (if there is reliable data on previous vaccinations) or three times (if they are absent); persons who had contact with people arriving from countries (regions) endemic (unaffected) with polio, from 3 months of life without age limit - once; persons working with live poliovirus, with materials infected (potentially infected) with wild poliovirus without age restrictions - once upon hiring. |
| Against pneumococcal infection | Children aged 2 to 5 years, adults belonging to risk groups (persons subject to conscription for military service, people over 60 years old, suffering from chronic lung diseases, people over working age, living in social service organizations). |
| Against rotavirus infection | Children for active vaccination to prevent diseases caused by rotaviruses. |
| Against chicken pox | Children and adults from risk groups, including those subject to conscription for military service, who have not previously been vaccinated and have not had chickenpox. |
| Against hemophilus influenzae | Children who were not vaccinated against hemophilus influenzae in the first year of life. |