How to choose injections for back and lower back pain
The information below is not a guide to action, does not replace medical advice, and is intended for general guidance only. All medications must be taken only as prescribed by a specialist, under medical supervision. Self-medication is unacceptable and can lead to serious harm to health.
Kazieva Aminat Ziyavovna
Neurologist
Rostov State Medical University
Experience since 2012
It is safer and more effective to consult a good doctor - an accurate diagnosis and correctly prescribed treatment will help you get rid of back pain with a greater likelihood than self-medication. Remember that many medications have side effects and should therefore only be used when indicated. No article or video about what injections to give for back pain can replace an in-person appointment and consultation with a doctor.
Nonsteroidal anti-inflammatory drugs (NSAIDs) for back pain
Nonsteroidal anti-inflammatory drugs are a group of drugs that have an analgesic effect. The mechanism of action of NSAIDs is the ability of these drugs to block inflammation by preventing the formation of the enzyme cyclooxygenase. Cyclooxygenase, in turn, is involved in the synthesis of prostaglandins - substances that support inflammation. Due to this ability, NSAIDs reduce inflammation, relieve inflammatory swelling, and have antipyretic and analgesic effects. For this reason, NSAIDs are often used in injections as an analgesic for back pain - as symptomatic and pathogenetic therapy.
NSAIDs have serious side effects because prostaglandins have other functions in the body that are not related to inflammation. The most common consequence of taking NSAIDs is drug-induced gastritis or drug-induced stomach ulcers. Gastrointestinal bleeding is possible. The most serious side effect of NSAIDs is chronic renal failure - long-term use of non-steroidal anti-inflammatory drugs leads to kidney failure. Treatment for chronic renal failure consists of hemodialysis or kidney transplantation. For this reason, NSAIDs are contraindicated in persons with peptic ulcers/gastritis or kidney disease.
NSAIDs are recommended to be used only as an injection for severe back pain , in case of a sharp exacerbation of a herniated disc, in case of injury, intercostal neuralgia. If the pain is tolerable, it is better to use local remedies - ointments, gels, patches containing NSAIDs. In this form, they have only a local effect and do not lead to serious side effects on the gastrointestinal tract and kidneys.
The most common drugs from the NSAID group
- Ketorol (ketoprofen);
- Xefocam;
- Texamen;
- Diclofenac;
- Meloxicam;
- Dexalgin.
How physiological dependence is formed
The development of drug addiction has complex biochemical and physiological mechanisms, since opioid analgesics disrupt the functioning of the most important biological substances - dopamine, serotonin, norepinephrine, endorphin, enkephalin, glutamic acid, gamma-aminobutyric acid and glycine. All these substances determine human behavior, his emotions, preferences and pleasure, are responsible for the processes of excitation and inhibition in the brain, for memory and attention. This is a delicate mechanism; if it is violated, serious consequences arise.
The central nervous and endocrine systems operate on the principle of negative feedback. For example, when a person takes testosterone in capsules for a long time, the body decides that it can not produce its own testosterone, since the hormone comes from the outside - testicular atrophy develops (they produce testosterone).
The same applies to brain neurotransmitters, which are responsible for pleasure, feelings of happiness and psychological comfort, joy and good mood. Regular non-medical use of narcotic analgesics, such as morphine and its synthetic and semi-synthetic analogues, leads to a severe deficiency of endorphin, dopamine, serotonin and enkephalin, since the body ceases to produce its own neurotransmitters.
When a person takes narcotic analgesics, the brain does not sense the deficiency of neurotransmitters. However, when the dose is reduced or not delivered at all, a crisis develops - a severe withdrawal syndrome, which occurs in response to a lack of endorphin and dopamine. And when a person stops consuming substances, the body requires the supply of opioid analgesics from the outside - a strong obsessive need for the drug arises. Thus, opioid analgesics are integrated into the internal regulatory system of opioid neurotransmitters and cause physiological dependence.
Muscle relaxants for back pain
Pathological muscle spasm is of great importance in the development of spinal diseases such as ankylosing spondylitis and other spondyloarthritis, spinal osteochondrosis, intervertebral disc herniation, multiple sclerosis and other neurological diseases. By relaxing the back muscles, peripherally acting muscle relaxants help relieve back pain caused by muscle spasms. They also have a weak local anesthetic effect, help improve blood circulation, and increase the range of motion in diseased segments of the spine. The analgesic effect of muscle relaxants is enhanced in combination with NSAIDs, which allows their use in the treatment of acute and chronic back pain as pathogenetic and symptomatic therapy.
Kazieva Aminat Ziyavovna
Neurologist
Rostov State Medical University
Experience since 2012
Side effects of muscle relaxants are determined by the mechanisms of their action - general weakness, dizziness, and increased fatigue are most often observed. Allergic reactions, cardiac rhythm and conduction disturbances are possible.
The most common muscle relaxants for treating back pain are:
- Tolperisone (Mydocalm);
- Tizanidine (Sirdalud);
- Baclofen (Baclosan);
Hydroxyzine (Atarax) is an antihistamine that is also a weak sedative, tranquilizer, analgesic and muscle relaxant. It is used for the same indications as peripheral muscle relaxants, relieving back pain. The tranquilizing and sedative effect allows the drug to be used to eliminate anxiety, phobias, anxiety and irritability. Due to these effects, Atarax is often used for diseases of the musculoskeletal system.
Three-stage pain correction system
The main method of treating pain in oncology is drug therapy. In the practice of Euroonko, a three-stage pain relief system of non-narcotic and narcotic analgesics is used, which allows you to effectively relieve pain and keep it under control. We take into account the recommendations of the World Institute of Pain (FIPP WIP, USA), the European Federation of the International Association for the Study of Pain (EF IASP).
The method consists of sequential use of analgesics of increasing strength in combination with adjuvant therapy as the pain intensity increases. An important principle is to begin pharmacotherapy immediately when the first signs of pain appear, before a complex chain reaction develops that leads to chronic pain syndrome. The transition to a stronger painkiller is made when all the drugs of the previous step are ineffective in their maximum dosages.
- At the first stage,
non-steroidal anti-inflammatory drugs (NSAIDs) are effective for mild pain. - At the second stage, for moderate pain,
drugs are used that contain a combination of weak opiates and non-narcotic analgesics. The first include dionin, tramadol, promedol, prosedol, tramal. Tramadol is most often used due to its high effectiveness and ease of use. - At the third stage, for severe pain,
narcotic analgesics are prescribed: buprenorphine, morphine, fentanyl, omnopon.
At any stage of pain therapy, analgesics must be taken regularly by the hour. The dose is adjusted taking into account the type and intensity of pain. If the drug becomes ineffective, it is advisable to replace it with an alternative drug of similar strength, but recommend it to the patient as more powerful.
Corticosteroids - preparations of adrenal hormones - are often used as analgesics. They have a powerful anti-inflammatory effect, especially important for pain caused by nerve compression, headaches caused by intracranial hypertension, and bone pain.
Anesthesiologist-resuscitator Vadim Sergeevich Soloviev about opioid analgesics:
Our doctors follow the principles of pain therapy proclaimed by WHO:
- “By mouth” (orally)
means that all injectable forms of analgesics should be excluded and therapy should be carried out using non-invasive dosage forms (tablets, capsules, syrups, transdermal therapeutic systems, rectal forms of drugs, etc.). - “On the clock”
- analgesics should be prescribed regularly according to the schedule, in accordance with the duration of the drug’s effect, without waiting for the development of severe pain, excluding the possibility of “breakthroughs” of pain. - “Ascending”
- the selection of drugs for pain relief is carried out from non-opioid analgesics for mild pain, “mild” opioids for moderate pain and strong opioid analgesics for severe pain, as the pain intensity increases, in accordance with the “WHO pain management ladder” - “Individual approach”
- implies the need for an “individual” selection of an analgesic and is based on the selective selection of the most effective analgesic in the required dose with the least side effects for each individual patient, taking into account the characteristics of his physical condition. - “With attention to detail”
- involves taking into account the characteristics and details of each patient, of course, prescribing co-analgesics and adjuvant agents as the need arises, and monitoring patients.
Steroid drugs for back pain
Steroid drugs are synthetic analogues of adrenal hormones that have a powerful anti-inflammatory effect that significantly exceeds that of NSAIDs. Inflammatory processes in diseases of the spine are the main source of pain. Taking and prescribing steroid hormones as an analgesic is justified only for very severe pain, since this group of drugs has significant side effects.
With prolonged and uncontrolled use, steroid drugs can cause stomach ulcers, gastric bleeding, hormonal disorders, increased blood pressure, Itsenko-Cushing syndrome (obesity, excess hair growth, high blood pressure, infertility), decreased immunity with the occurrence of secondary infections. Possible atrophy of the adrenal cortex, muscle atrophy at the injection site, osteoporosis with pathological fractures, thromboembolism, diabetes mellitus. It is strictly forbidden to use hormonal drugs without a doctor’s prescription and supervision.
Most often, steroids are part of a “cocktail” used for paravertebral or epidural blockades for very severe back pain - the effect after the injection occurs instantly and lasts several days. However, this treatment method is symptomatic therapy and does not affect the outcome and recovery time.
Most Commonly Used Steroid Drugs for Back Pain
- Betamethasone (Flosteron, Diprospan);
- Hydrocortisone;
- Prednisolone;
- Kenalog.
What is the reason for failure in pain treatment?
Due to the lack of specialized training in pain management, even among oncologists, and due to the perception of cancer as an incurable disease, even medical specialists often do not realize that cancer pain can be managed.
In 80–90% of patients, pain can be completely eliminated, and in the rest, its intensity can be significantly reduced. To do this, the doctor needs to take into account each of the sources and mechanisms of pain to select adequate pain therapy for cancer.
In clinical practice, we constantly encounter typical errors in the treatment of pain: unreasonably early prescription of narcotic analgesics, use of excessive dosages of drugs, non-compliance with the prescription regimen of analgesics.
Chondroprotectors for back pain
Chondroprotectors are drugs that have the ability to stimulate metabolism in cartilage and protect it from damage and premature wear. The mechanism of action of chondroprotectors is the ability to trigger the synthesis of collagen - the main protein of connective tissue, responsible for the strength, elasticity and flexibility of joints, bone tissue, intervertebral discs, ligaments and tendons. Taking chondroprotectors allows you to slow down the destruction of cartilage, reverse degenerative processes, and restore the structure of connective tissue. Thanks to these effects, chondroprotective drugs relieve pain, reduce inflammation, and improve spinal mobility.
Kazieva Aminat Ziyavovna
Neurologist
Rostov State Medical University
Experience since 2012
Most often, chondroprotectors are prescribed orally in the form of tablets and capsules. There are injectable forms of this group of drugs that are administered intramuscularly for back pain caused by degenerative-dystrophic diseases of the spine (osteochondrosis of the spine, intervertebral hernia, spondyloarthritis and spondyloarthrosis, spondylosis). Chondroprotectors are usually well tolerated by patients, do not have significant side effects, and are etiotropic, pathogenetic and symptomatic therapy. The disadvantage is that to obtain any significant effect, long and expensive repeated courses of treatment are required.
Chondroprotective drugs for the treatment of back pain:
- Chondroitin sulfate (Chondrolone);
- Alflutop.
Vitamin preparations of group B
The nature of back pain is often associated with neurological disorders - numbness, crawling sensation, burning sensation on the skin, sensory disturbances, and the pain itself occurs as a result of irritation or pinching of the spinal cord roots. This is especially true for chronic back pain. Acute pain syndrome also occurs as a result of impaired perception of nerve impulses from inflamed or damaged muscles, ligaments, and tendons. B vitamins (B1, B6, B12) are of great importance for the normal function of the nervous system in general and the peripheral nervous system in particular. Thus, a deficiency of these vitamins leads to neuropathies and neuritis.
Thiamine (vitamin B1) plays an important role in nerve regeneration, ensures redox reactions and metabolism in nervous tissue, and regulates the supply of nutrients and biologically active substances. Pyridoxine (vitamin B6) has antioxidant properties and provides the function of transport proteins that carry nutrients and biologically active substances from neurons to nerve fibers. Vitamin B12 (cobalamin) takes part in biochemical processes in nerve tissues, stimulates the synthesis of myelin (a substance that insulates nerve fibers).
Kazieva Aminat Ziyavovna
Neurologist
Rostov State Medical University
Experience since 2012
B complex vitamins in the form of injections are often used as injections for back pain as so-called neurotropic therapy. A course of such drugs has an analgesic effect, stimulates metabolism and regeneration in the affected nerves, and improves the functional state of the entire nervous system as a whole. The effectiveness of the vitamin B complex for back pain has been proven in experiments - the joint administration of this group of drugs with NSAIDs and muscle relaxants allows you to reduce the dose and, accordingly, the likelihood of developing side effects of the latter.
When used correctly, B vitamins are well tolerated by patients and have virtually no serious side effects. It is important to remember that some vitamin B complex injections contain lidocaine; for pain relief, the injection is quite painful. If the patient has an allergy or individual intolerance to lidocaine, it is necessary to choose a drug that does not contain it.
There are many different complex drugs of group B on the market with different names , which are used as injections for back pain (as pathogenetic and symptomatic therapy):
- Milgamma
- Combilipen
- Neurobion
- Trigamma
Mechanism of action of painkillers
In pharmaceutical practice, both natural opiates obtained by processing the seeds of certain varieties of poppy and their synthetic analogues are used. Currently, the latter are used more often, as they have a much more pronounced therapeutic effect.
The mechanism of the analgesic action of drugs of this group consists of the following components:
- inhibition of the processes of neural transmission of pain impulses in the central nervous system;
- change in subjective emotional perception of pain.
The effect of these medications is due to their selective influence on the functioning of the so-called opioid receptors (“mu”, “delta”, “kappa” located in the brain and other parts of the central nervous system), including inhibition of the activity of neurons localized in the spinal cord.
In addition, opioids are characterized by:
- pronounced sedative effect, which also reduces the intensity of pain impulses; in therapeutic doses, medications normalize the process of falling asleep, however, sleep is superficial and is easily interrupted under the influence of even minor external stimuli;
- inhibition of the activity of the respiratory center (this is especially pronounced for codeine), which leads to the use of some opiates for the symptomatic treatment of cough;
- stopping the gag reflex, which is especially important in oncology (drugs used for chemotherapy of tumors often cause uncontrollable vomiting);
- increased tone of the smooth muscles of the digestive and genitourinary systems;
- decreased heart rate;
- hypothermia.
Paravertebral blockade
This procedure is performed only by a specialist on an outpatient basis, due to the risk of damage to the nerve trunks (paravertebral block) and the spinal cord (paravertebral block). The purpose of the procedure is to eliminate back pain by introducing a solution of medications (local anesthetics, steroid hormones) into the epidural space of the spinal cord. This achieves an immediate analgesic effect, which helps even with unbearable pain in the back, lower back and lower extremities (symptomatic and pathogenetic therapy of back pain).
This procedure, if performed incorrectly, can lead to serious complications. Therefore, this treatment method is used only for severe and unbearable pain. In all other cases, it is better to limit yourself to safer methods.
For paravertebral blockades, it is permissible to use a more complex combination of drugs - NSAIDs, glucocorticosteroids, local anesthetics, chondroprotectors, vitamin B complex. The injection is performed through the muscles running along the spine until it touches the transverse process of the vertebra, 2 cm away from the center of the spine. The roots of the spinal cord pass in close proximity to the tip of the needle, where the drug is injected. The procedure can be performed under the control of an ultrasound machine.
Triad injections
Troychatka is often called a mixture of three drugs - Analgin, Diphenhydramine and Papaverine. However, it is more correct to call this “cocktail” a lytic mixture, since its use leads to a rapid decrease in temperature during fever. Triplet is often suggested to be used for back pain, but its use in this capacity is not only not justified, but also ineffective and unsafe. Firstly, Analgin is recognized throughout the world as a highly toxic drug and has not been used in practice for a long time. Secondly, with frequent use of Analgin, serious side effects are possible, including impaired hematopoiesis and aplastic anemia. Thirdly, in terms of pain relief power, triad is much inferior to other drugs from the NSAID group.
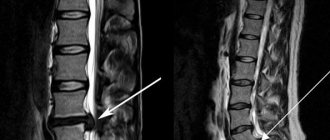
You should not take recommendations from non-specialists, as well as articles on the Internet written by people who do not have a medical education as a guide to action (texts with headings like “ list of the best injections for back and lower back pain ” should be skipped immediately). Pain is a nonspecific symptom that can occur in a variety of diseases. Back pain can be a sign not only of osteochondrosis, but also of serious diseases - spinal cord tumors, spinal tuberculosis, multiple sclerosis. Modern medicine makes it possible to clarify and determine the cause of pain in just one MRI study. And a consultation with a good doctor and the treatment he prescribes will be much more effective than weeks or even months of back pain.
Painkillers for stomach cancer
About 70% of patients suffering from stomach cancer experience discomfort and pain. As a rule, pain is localized in the abdomen, but as the tumor progresses it can also occur in other places: in the back, ribs, bones. Neuropathic pain may occur as a symptom of paraneoplastic syndrome or a side effect of chemotherapy.
In addition to the three-step system, benzodiazepines, antidepressants, adrenal hormones (prednisolone, dexamethasone), sleeping pills, and antipsychotics are used to combat pain and discomfort in stomach cancer. For bone pain and pathological fractures, bisphosphonates are prescribed.
The doctor can perform two types of nerve blocks:
- Celiac plexus block
helps relieve pain in the upper abdomen. The conduction of pain impulses through the nerves of the stomach, liver, pancreas, gall bladder, intestines, and kidneys is blocked. - Hypogastric plexus block
helps relieve pain in the lower abdomen. During it, the nerves of the lower intestine, bladder, testicles, penis, prostate, uterus, ovaries, and vagina are blocked.
Plexus blocks can be performed using anesthetics and drugs that temporarily damage the nerves. With neurolysis, a drug is administered that destroys the plexus.