General information
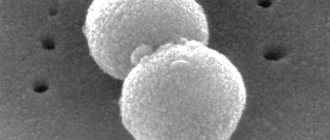
Haemophilus influenzae infection (Hib infection) is caused by Haemophilus influenzae type b. It can cause acute infectious diseases - purulent meningitis, pneumonia (pneumonia), epiglottitis (inflammation of the epiglottis), arthritis (inflammation of the joints), as well as purulent damage to the whole body - sepsis. Hemophilus influenzae infection is characterized by predominant damage to the respiratory system, central nervous system and the development of purulent foci in various organs. The bacterium H. influenzae is localized in the nasopharynx, from where it can be transmitted to other people by airborne droplets. Only a very small number of those in whom the pathogen is localized in the nasopharynx develop a disease with clinical manifestations. However, carriers of H. influenzae in the nasopharynx are an important source of spread of the pathogen.
How does infection occur?
Haemophilus influenzae is an infection whose primary mode of transmission is airborne droplets. Infection occurs when the patient sneezes, coughs or talks, producing mucus or sputum.
In some situations, pathogenic pathogenic flora enters the human body through contact and household contact. We are talking about a towel, toys or dishes. A person is a source of infection from the moment of infection until complete recovery.
Haemophilus influenzae infection enters the human body through the nasopharynx. This is the latent stage when pathogenic flora develops within the ENT organs. Further, the body’s resistance decreases, and pathogenic bacteria grow. This is the manifest stage, when a viral infection occurs.
Hemophilus influenzae spreads throughout the body through the blood or lymph, entering various internal organs and provoking an inflammatory process. In severe situations, even bones and joints are affected. Once in the central nervous system, Haemophilus influenzae affects the meninges, causing the development of meningitis.
Chance of getting sick
There are several risk groups for this disease. Firstly, children most often suffer from this infection. According to various studies, carriage of Haemophilus influenzae in children reaches 50%. Infants 6-12 months of age who are bottle-fed and do not receive small additional amounts of maternal antibodies in breast milk have a particularly high risk of developing the most severe forms of infection - pneumonia and meningitis. For this reason, artificial feeding is an additional indication for vaccination against Hib infection, starting from 3 months of age.
People of extreme ages (children under 2 years of age, the elderly) and people with low socioeconomic status are also susceptible to hemophilus influenzae infection. In addition, people with low socio-economic status, extremely weakened and suffering from alcoholism, patients with lymphogranulomatosis (Hodgkin's disease), sickle cell anemia are susceptible to the disease; persons who have undergone splenectomy (removal of the spleen).
The incidence increases in late winter and spring. In recent years, the incidence of morbidity in adults has increased markedly.
Risk group
Opportunistic microorganisms are always present in the body of a healthy person. They are harmless as long as, for example, the person’s immunity is strong. Against the background of its decrease, favorable conditions are created for the development of infection, so pathogens begin to multiply, which provokes the development of the inflammatory process.
Haemophilus influenzae is a serious and dangerous infection that often occurs in the following segments of the population:
- newborns;
- elderly people;
- persons who live in unfavorable living conditions;
- people with congenital or acquired immunodeficiency pathological conditions;
- children who attend kindergarten;
- persons suffering from chronic alcohol dependence.
Infection with Haemophilus influenzae also threatens patients who take cytostatics and children who are bottle-fed. The same applies to premature babies, preschool workers, and cancer patients. Children from orphanages are also at risk.
Symptoms
The duration of the incubation period is difficult to determine, since the disease is often a consequence of the transition of a latent infection to a manifest one. Both a local inflammatory process of the mucous membrane of the upper respiratory tract and diseases caused by hematogenous dissemination can develop.
Complications after an illness
Often, hemophilus influenzae infection occurs in children in the form of a common respiratory infection with corresponding symptoms. However, cases of more severe forms of infection are not uncommon. The most severe form of Haemophilus influenzae infection is purulent meningitis. According to some data in Russia, in children under 6 years of age, up to a third of all cases of purulent meningitis are caused by Haemophilus influenzae type b. Haemophilus influenzae meningitis is difficult to treat because its causative agent produces enzymes that make it resistant to antibiotics (about 20-30% of Haemophilus influenzae bacilli isolated from patients are not sensitive to many antibiotics). Therefore, treatment results are not always successful, and mortality in severe forms of the disease can reach 16–20%.
A third of patients who have had hemophilic meningitis develop irreversible neurological complications - seizures, delayed neuropsychic development, deafness, blindness, etc.
Pneumonia caused by Haemophilus influenzae type b occurs predominantly in children aged 2 to 8 years, and its course in 60% of cases also has various complications, including those affecting the heart and lungs.
Up to half of all purulent infections of the ear, throat, and nose are associated with hemophilus influenzae infection, in particular, recurrent purulent otitis (inflammation of the middle ear) and sinusitis (inflammation of the paranasal sinuses).
Hemophilus influenzae sepsis most often develops in children 6-12 months of age who are predisposed to this disease. It proceeds violently, often like lightning, with septic shock and rapid death of the patient.
Purulent arthritis is a consequence of hematogenous introduction of Haemophilus influenzae and is often accompanied by osteomyelitis.
Symptoms
The duration of the incubation period is not precisely determined. It is believed that it is 2-4 days. All this time the patient is dangerous to others. At the initial stage, the symptoms of hemophilus influenzae infection are similar to colds. The disease in most cases proceeds like a common ARVI. But it happens that the infection becomes the cause of more serious diseases with specific manifestations.
Clinical signs of pathology are determined by the localization of the pathological process. Intoxication and catarrhal syndromes are characteristic of any clinical form of infection. In patients, the temperature rises to 40 degrees, chills, cephalalgia, rhinitis, discomfort in the throat, wet cough, fatigue, lethargy, rumbling and pain in the abdomen, stool disorders, flatulence, pain in muscles and joints occur.
- If the primary source of infection is located in the ear, otitis media develops. Patients complain of throbbing and shooting pain in the ear, hearing loss, and the appearance of mucopurulent discharge.
- With sinusitis, there is discomfort in the nose, bursting pain in the projection of the affected sinus, purulent nasal discharge, impaired nasal breathing, and decreased sense of smell.
- Inflammation of the tissue is manifested by swelling of the face, mainly the cheeks, hyperemia or cyanosis of the skin, pain and fever.
- Epiglottitis is the most severe form of hemophilus influenzae infection, characterized by severe chills, cyanosis, shortness of breath, tachycardia, hypersalivation, stridor, and retraction of the pliable areas of the chest. Patients are in a forced position. The pain makes it difficult to swallow even liquid food. Rapidly progressing croup can lead to the death of the patient from asphyxia.
- Conjunctivitis in newborns is manifested by redness of the eyes, swelling of the eyelids, profuse lacrimation, and the appearance of purulent secretion in the corners of the eyes.
- Arthritis affects the large joints of the upper and lower extremities. The disease is accompanied by redness of the skin, swelling and local hyperthermia.
- Patients with pneumonia complain of chest pain, cough with purulent sputum, and fever.
- Meningitis is manifested by profuse vomiting without previous nausea, fever, chills, loss of consciousness, convulsions, meningeal signs, focal neurological symptoms, lethargy, adynamia, and rapid exhaustion of patients. Less commonly, stupor develops, and in some cases coma.
- Osteomyelitis causes severe pain in the limb, swelling of the tissue over the affected bone and redness of the skin.
- With septicemia - splenomegaly, hypotension, tachycardia, hemorrhages on the skin, lack of appetite, stool disturbances. Patients sleep a lot and restlessly. The disease has a rapid and even lightning-fast course. It often ends in infectious shock and death of the patient.
Haemophilus influenzae can cause simultaneous damage to several organs: meningitis in patients is often combined with arthritis, cellulitis, and epiglottitis.
Hemophilus influenzae infection is a serious medical problem due to the variety of clinical forms, frequent generalization of the process, the development of severe complications and a high risk of death.
Treatment
Haemophilus influenzae Hib infection is difficult to treat, since Haemophilus influenzae is record resistant to antibiotics. For this reason, even timely treatment with modern antibiotics is often ineffective. Penicillin antibiotics, erythromycin, chloramphenicol, tetracycline - the percentage of Haemophilus influenzae resistance to them is 80-100% (of the number of isolated bacterial samples). Without etiotropic therapy, some forms of hemophilus influenzae infection (meningitis, epiglottitis) almost always end in the death of the patient. It is necessary to begin treatment for hemophilus influenzae infection as early as possible.
POSITIVE AND NEGATIVE ASPECTS OF VACCINATION
The number of parents refusing to immunize their children increases every year. Opponents of vaccinations argue that the introduction of vaccine preparations is dangerous for the child’s body and provokes the development of neurological complications and disability.
However, many years of immunization experience have proven the following advantages of vaccination against Haemophilus influenzae:
- High efficiency. The vaccine provides protection for a child for 5 years in 95% of cases;
- Vaccinations have reduced the incidence of haemophilus influenzae meningitis in children by 87% in the UK. There are completely no cases of this infection in the Netherlands;
- Vaccination can reduce the incidence of illness in a child upon entering kindergarten;
- In vaccinated children, if infected, the infection is mild.
The listed facts indicate the need for vaccination if the child has no contraindications.
Effectiveness of vaccination
In 2000, before the widespread introduction of Hib vaccine in resource-limited countries, Hib disease accounted for 8.13 million cases of serious illness in children aged 1–59 months (range, 7.33–13.2 million cases). ) and 371,000 deaths (fluctuation amplitude – 247,000=527,000). By 2008, when 136 WHO Member States introduced the Haemophilus influenzae vaccine, there were an estimated 203 000 deaths due to Hib infection in children under 60 months of age (range 136 000–281 000).
The effectiveness of Hib vaccines is 95-100%; the protective antibody titer lasts for at least 4 years.
Among vaccinated people in 10 European countries, Israel and Australia, Hib infection developed with a frequency of only 2 cases per 1 million; 18% of these children had problems, including prematurity; 33% had low immunoglobulin levels.
TYPES OF VACCINES
The vaccine against Haemophilus influenzae is a drug developed on the basis of polysaccharides of the capsule of the pathogenic microorganism conjugated with tetanus toxoid proteins. This makes it possible to convert microbial particles into an antigen, which contributes to the formation of a pronounced immune response. Conjugation also helps reduce the reactogenicity of the vaccine preparation, making it as safe as possible for the fragile organism of infants.
Important! The vaccine against Haemophilus influenzae has a unique effect, leading to an exponential increase in antibodies against the infectious agent if the drug is administered repeatedly.
The following vaccines against hemophilus influenzae are widely used in Russia:
- Mono-vaccine Act-HIB (manufactured in France). The drug is created exclusively on the basis of Haemophilus influenzae antigens. This vaccine has been used to prevent Haemophilus influenzae for many decades and has proven its effectiveness. Therefore, it is widely used to form stable immunity in children under 12 months;
- Monovaccine Hiberix. The vaccine was manufactured in Belgium and is an analogue of Act-HIB. In Russia, the drug has been used for a relatively short time;
- Polyvalent drug Pentaxim. The French vaccine will protect the child’s body from 5 serious diseases: polio, whooping cough, Haemophilus influenzae, tetanus, diphtheria. However, the pertussis component increases the reactogenicity of the vaccine preparation. Therefore, vaccination against Haemophilus influenzae infection will lead to the development of pronounced side effects;
- Combined vaccine Infanrix penta. The drug, produced in Belgium, is an analogue of Pentaxim.
Due to their ease of use and effectiveness, combination vaccines are widely used for vaccination against Haemophilus influenzae in district clinics. However, parents have to purchase the vaccine themselves at the pharmacy.
Vaccines
Currently, the only way to prevent this infection is vaccination. According to WHO recommendations, vaccination against Haemophilus influenzae is recommended for all children. The effectiveness of vaccination today is estimated at 95-100%. There have been numerous trials of polysaccharide conjugate Hib vaccines in Europe and North America. In particular, a clinical trial in the UK (1991-1993) showed an 87% reduction in the incidence of haemophilus influenzae meningitis. In Holland, during a similar study, a complete absence of cases of meningitis of hemophilic etiology was recorded within 2 years after the start of immunization.
Modern vaccines are chemically linked antigens of the Haemophilus influenzae capsule and tetanus toxoid, which is necessary for the main antigen to produce immunity in children under 18 months of age.
Recommended calendars. WHO recommends one of the following vaccination schedules against Hib infection:
- 3 doses as part of the primary vaccination course without a booster dose (3p+0);
- 2 doses as part of the primary course of vaccination and a booster dose (2p+1);
- 3 doses as part of the primary course of vaccination and a booster dose (3p+1).
In countries where the peak burden of severe disease from Haemophilus influenzae type b occurs in young infants, early administration of 3 doses of vaccine may be beneficial.
By Order of the Ministry of Health of the Russian Federation No. 125 of March 21, 2014, vaccination against hemophilus influenzae type b was introduced into the National Calendar of Preventive Vaccinations of the Russian Federation for children at risk.
More about vaccines
Types of vaccines
The latest generation drugs are used to vaccinate the population:
- "Act-HIB" - manufacturing country France;
- Hiberix - supplied from Belgium.
Conjugate vaccines contain capsular polysaccharides of Hib infection and tetanus toxoid. The latter is well recognized by the human immune system. The action of this vaccination provides a pronounced primary reaction and immunological memory.
Of the combination drugs used in Russia, Pentaxim and Infanrix Hexa. Both drugs contain vaccinations against:
- tetanus;
- whooping cough;
- polio;
- diphtheria;
- polio;
- Haemophilus influenzae.
However, the Infanrix Hexa vaccine contains an additional vaccine against hepatitis B.