Measles, clinical picture and course of the disease
The disease begins with an incubation period, which on average in children ranges from 10 to 14 days. During this period, the virus develops latently in the body, so the only criterion by which one can suspect that a child could have become infected is if a measles quarantine was declared at school or kindergarten. In this case, you can protect other children and members of your family who have not been vaccinated against measles by separating them from the child after the 8-9th day of the incubation period for a week (or more if the child is sick).
The initial period of measles disease is catarrhal. Since during this period the disease begins acutely with an increase in body temperature to 39 degrees C, a dry, obsessive cough appears in combination with severe conjunctivitis - redness of the mucous membranes of the eyes and “photophobia”. Bright light greatly irritates a person with measles. Cough in the initial period of measles tends to intensify within 3-4 days; in children under 5 years of age there is a high probability of hoarseness, which is the first sign of obstructive laryngitis (in the old terminology - false croup). A cough in a patient with measles is accompanied by a runny nose with copious mucous, and then mucopurulent discharge from the nose, severe general intoxication: weakness, disturbed sleep and decreased appetite.
By the 3rd – 4th day of the disease, the face of a patient with measles takes on a swollen appearance with “swollen” eyelids, red conjunctivae, lacrimation and possible purulent discharge from the eyes.
A typical symptom of measles is described, the so-called Filatov-Koplik spots, which appear at the end of the catarrhal period and 1-2 days before the first skin rash. Filatov-Koplik spots are small whitish-gray dots surrounded by a halo of hyperemia. They are located in the mouth, on the mucous membrane of the cheeks, opposite the molars. In addition to Filatov-Koplik spots in the mouth, red spots may appear on the soft palate, which are called measles enanthema.
The period of rash begins on the 4th – 5th day of the disease with the appearance of maculopapular rash elements on the skin. During this period, intoxication, as a rule, intensifies; the temperature, after some decrease at the end of the catarrhal period, rises again to high numbers. Measles is characterized by a “staged rash.” The first elements of the rash appear behind the ears, on the scalp, as well as on the face and neck. On the 2nd day, the rash covers the torso and arms; on the third day from the onset of the first rash, measles exanthema spreads to the lower part of the torso and legs. The measles rash can be described as bright pink and tends to coalesce into large lesions. The extinction of the elements of the rash also occurs gradually in the same order in which they appeared. In case of late diagnosis, it must be borne in mind that old elements of measles exanthema first turn pale, then acquire a brown color, and remain in this form for quite a long time, up to 10 days. During this final period of measles, the period of pigmentation, fine peeling is also observed on the skin.
In the final period of measles, the symptoms of intoxication and fever subside, and recovery occurs.
Measles
Measles is an anthroponotic acute viral infectious disease with an aspiration mechanism of pathogen transmission, which is characterized by a cyclical course, fever, intoxication, catarrhal respiratory syndrome, the presence of Filatov-Koplik spots and a maculopapular rash.
History and distribution. Measles has been known since ancient times. In the 9th century AD. e. described by the Arab physician Rhazes, who considered it a mild form of smallpox. Therefore, it received the name morbilli - small disease, in contrast to morbus - smallpox (great disease). In the 17th century, a detailed description of the measles clinic in England was given by T. Sydenham and Th. Morton in France. The viral etiology of measles was proven in 1911 by T. Anderson and J. Goldberger by infecting monkeys with blood filtrate and nasopharyngeal mucus of sick people, but the culture of the pathogen was isolated only in 1954 by J. Enders.
Measles in the Middle Ages and at the beginning of the 20th century was one of the most common childhood infectious diseases, which was characterized by a severe course and mortality among children under three years of age up to 40%. When measles was introduced into isolated areas (Faroe Islands, Fiji), up to 80% of the population became ill. The reduction in mortality was achieved thanks to the development of a seroprophylaxis method in 1916–1921. Nicolle (Ch. Nikolle), Conseil (E. Conseil) and Dedkwitz (R. Dedkwitz). Widespread use of the measles vaccine has led to a sharp decrease in the incidence and even its elimination in a number of countries. However, in recent years, cases of the disease have been observed among vaccinated people. According to WHO, up to 30 million cases of measles are registered annually in the world, of which about 50 thousand are fatal.
In Russia, a program for eliminating measles by 2010 was developed (Order No. 270 of the Russian Ministry of Health dated August 19, 2002).
The main principles of measles elimination are: achieving and maintaining a high (95–98%) level of vaccination coverage with live measles vaccine (LMV); implementation of effective epidemiological surveillance of measles, providing for the complete and active detection of all cases of measles and their laboratory confirmation, as well as timely adoption of management decisions and monitoring of their implementation.
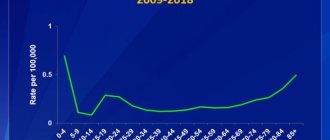
Currently, sporadic cases of the disease are being recorded in some territories of Russia. The incidence rate in 2009 was 0.07 per 100 thousand population; measles cases were recorded only in 10 constituent entities of the Russian Federation. In 2009, measles was not registered in 74 regions of Russia. Of the 100 registered cases of measles, 20 were imported from abroad (Thailand, India, Germany, France, China, Indonesia, Vietnam and Ukraine). The number of adults with measles is 71 people. Adults with measles were not vaccinated against measles (63%) or did not have information about vaccinations. Among those sick with measles: 29 children under the age of 17 years, including 28 under 14 years of age, of which 92% were not vaccinated against measles. In 2010, the incidence of measles increased by 25.9% compared to 2009 and amounted to 0.09 per 100 thousand population. Currently, the main population that determines the incidence of measles is adults. 127 cases of measles were registered in 11 constituent entities of the Russian Federation, including in the Amur region - 77 cases, the Republic of Buryatia - 19, Moscow - 16, Tyumen region - 5, St. Petersburg - 3, Sverdlovsk region - 2, Republics Dagestan and Tatarstan, Samara, Moscow and Belgorod regions - 1 case each.
Etiology. The causative agent of measles belongs to the genus morbillivirus, family of paramyxoviruses, has a spherical shape, a diameter of 120–250 nm, single-stranded RNA. The virion is surrounded by a two-layer lipoprotein envelope. The virus has three main antigens - hemagglutinin, protein F and nucleocapsid protein, and antibodies to hemagglutinin and protein F have a cytotoxic effect against virus-infected cells. The causative agent of measles is an interferon inducer and is antigenically homogeneous. Some variants of the virus are capable of long-term persistence in the human body. The measles virus is unstable in the external environment and quickly dies when exposed to sunlight and UV irradiation. At low temperatures it can persist for several weeks; at temperatures above 60 °C it dies instantly. At room temperature, the virus persists for 3–4 hours.
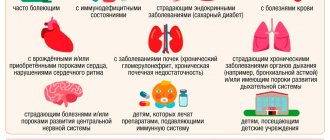
Epidemiology. The source of infection is only a sick person from the last days of the incubation period. The transmission mechanism is aspiration. Patients are especially dangerous in the catarrhal period of the disease, much less in the first 4 days of the rash period; if the disease is complicated by pneumonia, this period can be extended to 10–12 days from the onset of the disease. The route of transmission of measles is airborne. The virus is contained in large quantities in saliva, nasopharyngeal mucus and is released into the environment when coughing, sneezing, or talking. The causative agent of measles is extremely unstable in the external environment, so its spread usually occurs at a distance of about two meters from the source of infection. In some cases, under favorable conditions, an aerosol containing the virus can travel with convection (upward) air currents over long distances (up to 10 meters). Due to the high contagiousness of the measles virus, infection of susceptible people is possible even with fleeting contact with the source of infection, but its likelihood increases sharply when being in the same room with a sick person. Susceptibility to measles is extremely high, therefore, before the start of mass immunization, most people had measles in childhood, starting from 6 months, when the level of maternal neutralizing antibodies decreases, becoming less protective. Lifelong immunity. Recurrent cases were extremely rare. The winter-spring seasonality of the disease was recorded, with increases in incidence occurring every 2–4 years. During the period of routine vaccination against measles as part of the national calendar of preventive vaccinations and sporadic morbidity, seasonality and frequency are less clearly expressed; people of any age group who are not covered by vaccination get sick. At the same time, there is a pronounced trend of “maturation” of measles, so the proportion of people over 14 years old among the sick has reached 80%. The role of imported cases in the formation of measles outbreaks has increased, especially in border areas.
Pathogenesis. The causative agent of measles enters the body through the mucous membranes of the upper respiratory tract, penetrates the regional lymph nodes, where its primary replication occurs. Starting from the third day of the incubation period, the virus circulates in the blood and disseminates hematogenously in the body. In this case, an important role, as a fact of transfer, is played by leukocytes in which the virus multiplies. Further reproduction and accumulation of the virus occurs in all organs of the reticuloendothelial system, lymph nodes, tonsils, lymphoid elements of the whole body, and myeloid tissue of the bone marrow. In this case, proliferation of lymphoid and reticular elements occurs. During the incubation period, stimulation of the immune system begins. Cells affected by the virus are attacked by specific antibodies, killer lymphocytes and other factors of infectious immunity and nonspecific defense, resulting in their damage and lysis. This leads to a number of pathogenetically important stages: repeated intense viremia develops, the virus is fixed by epithelial cells, primarily of the upper respiratory tract, skin, and digestive tract. Once in the central nervous system, the virus infects nerve cells. Fragments of viral particles and lysed cells entering the blood sensitize the body, causing allergic reactions accompanied by vascular damage. It is these elements of pathogenesis that correspond in time to the onset of the disease and determine the symptoms of the disease. An important link in the pathogenesis is the development of immunosuppression, which, along with damage to the epithelial cover, contributes to the development of bacterial complications.
Massive production of interferon, synthesis of antibodies, and an increase in cellular protective reactions lead already by the third day of the rash period to a sharp decrease and cessation of viremia and elimination of the virus from the body. But in some cases, the measles virus can persist in the body for a long time and lead to the development of a slow infection of the central nervous system (subacute sclerosing panencephalitis).
Clinic. The incubation period lasts from 9 to 17 days, and with the prophylactic administration of immunoglobulin it can be extended to 28 days. Measles is characterized by cyclicality during the course of the disease. There are three periods of measles: catarrhal, rash and pigmentation. The disease begins acutely with symptoms of general intoxication (fever, headache, weakness, apathy, insomnia, decreased appetite), and catarrhal symptoms appear at the same time. Intoxication is moderate. Body temperature ranges from subfebrile to 38–39 °C, at the end of the catarrhal period it usually decreases to normal. Children are bothered by cough, sore throat, photophobia, and nasal congestion. Moderate mucous discharge from the nose. Children are irritable and capricious. Hoarseness appears.
When examined on the first day of illness, there was hyperemia and looseness of the mucous membranes of the oropharynx. From the 2nd-3rd day of illness, the cough is rough, “barking”, intrusive, hyperemia of the conjunctiva and sclera appears, swelling of the eyelids, photophobia with lacrimation, the face is puffy, enanthema appears on the soft and hard palate. A pathognomonic symptom of measles is Filatov-Koplik-Belsky spots, which are very small whitish dots surrounded by a halo of hyperemia, located on the transitional fold of the mucous membrane of the cheeks, usually near small molars and can spread to the mucous membrane of the gums and lips. They cannot be removed with a tampon or spatula and represent foci of epithelial necrosis. With more widespread necrosis, upon examination, solid whitish stripes can be seen on the gingival mucosa. By the time the rash appears, the Filatov–Koplik–Belsky spots disappear. In some patients, on days 2–3 of the catarrhal period, a pale pink spotted prodromal rash appears on the face, neck, chest, and arms, which quickly disappears. The duration of the catarrhal period is 3–4 days (from 2 to 8 days).
The period of rash is characterized by an increase in body temperature to maximum levels, symptoms of intoxication and catarrhal symptoms increase. Measles is characterized by stages of rash. The rash appears on the face and behind the ears. Within 24 hours, the rash spreads to the neck and chest. On the 2nd day, elements of the rash are detected on the remaining parts of the body, shoulders and thighs, on the 3rd day - on the forearms and legs. At this time, the rash on the face begins to turn pale. The general condition of the patient improves, the severity of intoxication and catarrhal phenomena decreases. The rash initially has the appearance of small papules, which, as the rash progresses, “group” into large maculopapular elements that merge with each other when the rash is profuse. It is typical that the rash is located against a background of pale skin and may be accompanied by mild itching. The period of pigmentation begins on the 4th day from the appearance of the rash. The temperature returns to normal, sleep and appetite are restored. The rash “fades”, loses its papular character, acquires a brown color (pigmentation), and fine pityriasis-like peeling of the skin appears. Pigmentation is an important diagnostic symptom of measles, which lasts up to 2-3 weeks. Against the background of measles rashes, petechiae are often found, especially on the neck and lateral surfaces of the body. In addition to these basic, diagnostically significant signs of the disease, a number of other significant symptoms are observed with measles.
Many patients experience an increase and sensitivity upon palpation of the cervical, occipital, and sometimes other groups of lymph nodes, often an increase in the size of the liver and spleen.
Auscultation of the lungs reveals hard breathing, and sometimes dry wheezing can be heard. There may be a decrease in blood pressure, tachycardia or bradycardia, and muffled heart sounds. If the digestive system is involved in the pathological process, there may be nausea, vomiting, loose stools without pathological impurities, coated tongue, and abdominal pain on palpation. A blood test determines leukopenia, lymphocytosis, and eosinopenia. ESR is normal or moderately elevated.
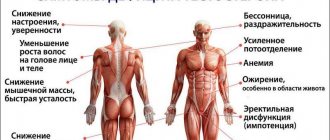
Features of measles in adults. In adults and adolescents, measles is characterized by a number of features: the disease is more severe, the intoxication syndrome is more pronounced (headache, sleep disturbance, vomiting), the catarrhal period is longer than in children - 4-8 days, Filatov-Koplik-Belsky spots are very abundant , often persist during the period of rash, at the same time, catarrhal symptoms are weakly expressed, the rash is profuse, polyadenopathy is more pronounced, the spleen is palpated more often, measles encephalitis develops in 2% of patients (in children 5–10 times less often), complications caused by bacterial flora, are rarely observed.
Mitigated measles
When anti-measles immunoglobulin is administered to contact persons during the incubation period for prophylactic purposes, mitigated measles develops, which is characterized by an extended incubation period of 21–28 days, a short catarrhal period (1–2 days) or its absence, catarrhal symptoms are mild, Filatov’s spots Koplik–Belsky are often absent. The rash is pale, small, not abundant, often not on the extremities. The staged appearance of the rash is not typical. The rash period lasts 1–2 days. Pigmentation after the disappearance of the rash is weak and disappears quickly.
Complications . In children, complications caused by bacterial flora are possible - purulent rhinitis, sinusitis, otitis, bronchitis, pneumonia, especially often in young children. These complications have been reported less frequently in recent years. There may be cases of laryngitis with laryngeal stenosis (measles croup). A severe complication is measles encephalitis or meningoencephalitis, which is most often detected during the period of fading of the rash, but is possible in earlier and later periods - from 3 to 20 days of illness. The beginning is sharp and stormy. The temperature rises, disturbances of consciousness and generalized convulsions appear, and patients often fall into a coma. There may be movement disorders (paresis, paralysis), often pyramidal signs. Some patients have meningeal syndrome, low lymphocytic or mixed pleocytosis is noted in the cerebrospinal fluid, and the protein content is increased. Patients often die during the acute period of the disease due to symptoms of cerebral edema and respiratory dysfunction. In those who have recovered, severe and persistent lesions of the central nervous system (paresis, hyperkinesis, decreased intelligence) are often detected.
Diagnostics . The diagnosis of measles is established on the basis of clinical and epidemiological data. If the patient has a previous history of measles and has been vaccinated against it, this completely excludes the diagnosis of measles. Information about contact with a person with measles is of relative importance, since casual contacts are often not identified. Detection of laryngitis, rhinitis, conjunctivitis in a patient, an increase in these symptoms over 2-3 days, and the presence of enanthema allows the doctor to suspect measles. The appearance of Filatov–Koplik–Belsky spots is of great diagnostic importance. During the period of rash, the diagnosis is based on identifying the catarrhal syndrome that precedes the appearance of the rash, the stages of the appearance of the rash, the characteristic appearance of the rash elements against the background of pale skin, and the dynamics of their transformation. Laboratory methods (detection of giant cells in nasal discharge, isolation of a virus culture, immunofluorescent method for detecting viral antigen, detection of antibodies using the hemagglutination inhibition test (HAI), compliment fixation reaction (CRS) or enzyme-linked immunosorbent assay (ELISA)) are rarely used in practice. Viral RNA from the first day of illness can be detected in blood and swabs from the oropharyngeal mucosa using the polymerase chain reaction (PCR).
Treatment . Patients are hospitalized for clinical (severe disease, complications) and epidemiological indications. Bed rest for the entire febrile period. The patient's bed should be positioned with the head end towards the window so that the light does not irritate the eyes; artificial lighting should be dim. The patient's diet must include fruit drinks, fruit juices, and mineral water. Food should be complete, rich in vitamins, and easy to digest. Dairy products should be excluded from the diet. Causal therapy has not been developed. In most cases, treatment is carried out at home and symptomatic and pathogenetic therapy is prescribed. Due to photophobia, the room in which the patient is located should be shaded. The oral cavity is treated with a solution of nitrofuran and chamomile infusion. Vitamin therapy: retinol (100,000 IU/ml) for children aged 1–6 months, 50,000 IU, 7–12 months, 100,000 IU, over one year, 200,000 IU. To alleviate a painful cough, the room air is humidified using damp sheets and antitussives are prescribed. The eyes are washed with warm boiled water several times a day. After removing pus and purulent crusts, a solution of retinol in oil is instilled into the eyes, 1-2 drops 3-4 times a day. Dry, cracked lips are lubricated with boric petroleum jelly or fat. The nose is cleaned with cotton swabs moistened with warm Vaseline oil; if crusts have formed, it is recommended to instill Vaseline oil into the nose, 1-2 drops 3-4 times a day. Antipyretics are prescribed in age-specific doses. Detoxification therapy is carried out in the hospital. There is evidence of the effectiveness of interferon drugs (Leukinferon). If complications develop, therapy is carried out according to the principles of treatment of these diseases. If pneumonia or otitis media develops, antibacterial therapy is prescribed in accordance with the results of sputum culture for sensitivity to antibiotics. With the development of encephalitis, treatment is aimed at maintaining vital functions and combating cerebral edema-swelling (ONS). For weakened patients and children under one year of age, preventive prescription of broad-spectrum antibiotics is possible according to individual indications.
Additional treatments. Physiotherapeutic methods for treating measles are chest massage and breathing exercises (prescribed and supervised by a physical therapy doctor). With the development of croup and pronounced symptoms of laryngotracheitis, inhalations with alkaline solutions, bronchodilators, and mucolytics are performed. For dry cough and dry wheezing in the lungs, microwave and ultra-high-frequency therapy in the chest area is indicated.
Forecast. With an uncomplicated course of the disease, the prognosis is favorable. The mortality rate for measles is currently about 1.5%; previously the mortality rate reached 10%. Fatal cases are recorded in developing countries and are mainly associated with the development of measles encephalitis, in which the mortality rate is 20–30%.
Prevention. The main method of preventing measles is vaccination, the purpose of which is to create immunity in the population to this infection. LCV vaccinations are carried out within the framework of the national calendar of preventive vaccinations and the vaccination calendar for epidemic indications. Routine vaccinations include a single vaccination at 12 months of age and a booster at 6 years of age. Vaccination coverage of children of decreed ages must be at least 95%. Post-vaccination antiviral immunity is formed in 95–97%, the duration of its protective effect is on average 14 years.
The complex of anti-epidemic and preventive measures includes identifying sources of infection, determining the boundaries of epidemic foci that have been in contact with a patient with measles and who are not protected against measles among them.
During the implementation of the measles elimination program in Russia, complete and active detection of all cases of measles becomes important, therefore patients with exanthem diseases at the slightest suspicion of measles must be examined by serological methods to verify the diagnosis. About each case of measles, as well as if there is a suspicion of measles, a doctor at a medical institution or a doctor engaged in private practice sends an emergency notification within 12 hours to the territorial department of Rospotrebnadzor at the patient’s place of residence.
A patient with measles is hospitalized for clinical and epidemiological reasons. The period of isolation of the source of infection determines the duration of the infectious period - 5 days from the moment the rash appears, and in the presence of pneumonia it increases to 10 days.
In order to early identify possible new cases of the disease in epidemic foci, contact children are examined daily in preschool institutions and schools with 2-fold thermometry. Children who have been in contact with the source of infection and were previously vaccinated with LCV are observed for 17 days from the moment of contact with the patient with measles. Children and adults under the age of 25 who are susceptible to measles are vaccinated according to epidemic indications with LCV or other vaccines registered in Russia no later than 72 hours from the moment of expected contact.
Susceptible to measles are considered those who have not had measles and have not been vaccinated against it or have been vaccinated once, as well as persons with an unknown infectious and vaccination history or those who, during a serological examination, do not have antibodies to the measles virus in protective titers (in RTGA - 1 :5, in the reaction of inhibition of passive hemagglutination (RPHA) - 1:10 and above).
Children who have interacted with a patient with measles and have medical exemptions from preventive vaccinations or have not reached vaccination age are advised to administer human immunoglobulin (normal or anti-measles) intramuscularly in a dose of 1.5–3.0 ml no later than the 5th day from the moment of contact with the patient . The administration of immunoglobulin prevents the disease or alleviates its course. They are monitored medically for 21 days from the moment the first case of the disease is detected and are separated from the team from the 8th to the 21st day.
In an epidemic focus of measles, ventilation and wet cleaning are carried out.
It should be noted that achieving sustainable stabilization of the incidence of measles at a sporadic level is only possible due to high coverage of the child population with measles vaccinations at each pediatric site. Moreover, the level of vaccination coverage should not decrease when low incidence rates are registered in the territory or when there is a complete absence of measles cases. It must be borne in mind that the level of vaccination coverage of at least 95% of decreed ages prevents the spread of the pathogen among the population if it is brought from abroad.
The effectiveness of measles vaccine prevention is also determined by strict adherence to the “cold chain” principle, i.e. ensuring temperature conditions for the transportation and storage of LCVs (0–8 °C) from the vaccine manufacturer’s enterprise to the vaccination rooms of medical institutions, which are regulated by Sanitary Rules SP 3.3. 2.028–95 “Conditions for transportation and storage of medical immunobiological preparations.”
As part of the implementation of epidemiological surveillance of measles in conditions of low incidence, a significant role is assigned to serological monitoring, which allows timely identification of risk groups and areas when identifying an increase in the number of individuals seronegative for the measles virus.
Implementation of the principles of epidemiological surveillance of measles, including monitoring the incidence, state of collective immunity, clinical course of infection, circulation of pathogen genotypes, assessment of the effectiveness of preventive and anti-epidemic measures, making operational decisions and control are the basis for achieving the goals of the national measles elimination program in the Russian Federation and certification territories free from this infection.
Literature
- Yushchuk N. D., Vengerov Yu. Ya. Lectures on infectious diseases. 3rd ed., revised. and additional M.: OJSC “Publishing House “Medicine”, 2007. 1032 p.
- Pozdeev O.K. Medical microbiology. Under. ed. V. I. Pokrovsky. 2nd ed., rev. M.: GEOTAR-MED. 2004. 768 p.: ill. (Series “XXI Century”.)
- Infectious and parasitic diseases in diagrams and tables. Ed. N. D. Yushchuk. M.: FGOU "VUNMC Roszdrav", 2008. 448 p.
- Infectious diseases: National guidelines. Under. ed. N. D. Yushchuk, Yu. Ya. Vengerova. M.: GEOTAR-Media, 2009. 1056 p. (National Guides Series.)
- Yushchuk N.D., Vengerov Yu.Ya. Kryazheva S.S. Infectious human diseases: Handbook. M.: OJSC “Publishing House “Medicine”, 2009. 264 p.
G. K. Alikeeva, Candidate of Medical Sciences N. D. Yushchuk, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Medical Sciences A. V. Sundukov, Doctor of Medical Sciences, Professor G. M. Kozhevnikova, Doctor of Medical Sciences, Professor N. Kh. Safiullina , Candidate of Medical Sciences E. V. Kukhtevich, Candidate of Medical Sciences MGMSU, Moscow
Contact information for authors for correspondence
Preventing measles
The main method of preventing measles is active immunization, that is, measles vaccination, which, according to the mandatory vaccination calendar approved in the Russian Federation, is carried out in children aged 12 months and 6 years, as well as adults under 35 years of age who have not had measles.
Unfortunately, the practice of “unreasonable medical withdrawals”, and frankly speaking, the unwillingness of some parents to get vaccinated in the case of measles, is already leading to very negative consequences. In 2011, an outbreak of measles was recorded in Moscow, the source of which was an adult who worked in a children's team (not a health worker), and as a result, children with young mothers were infected in several children's hospitals, where infants were taken from a children's institution in the catarrhal period of measles infections with a diagnosis of ARVI, when measles-specific rashes on the skin and mucous membranes, as you and I now know, do not yet exist. Every year, cases of epidemic outbreaks of measles are recorded in cities of the Russian Federation. Given the high mobility of the population, including children in large cities, unfortunately, no one is immune from contact with a person with measles. A timely measles vaccination significantly reduces the risk of getting sick from accidental contact in public places, but if, by an unfortunate coincidence, there is close contact with a relative or friend who is at an early stage of measles infection, then the presence of post-vaccination immunity reduces the likelihood of a moderate or severe course measles in a vaccinated person is approximately 80%, and in a child with good immunity it is almost 100%. In other words, vaccinated children usually suffer from measles in a mild form, unlike unvaccinated children, who always get seriously ill, and some also suffer the serious complications mentioned above.
Measles vaccination schedule for children
| Child's age | Indications |
| 12 months | All children in this age group |
| 12-18 months | Previously unvaccinated or lacking information about vaccination |
| 6 years | All persons at this age |
| 7-17 years old | Previously unvaccinated, not sick, not having information and vaccinated once |
Measles vaccination is universal and occurs at an early age. It is carried out in two stages. The first vaccination is given to one-year-old children; a delay of several months is acceptable. The second time the procedure is carried out at the age of 4 to 6 years. It is immunization in two stages that makes it possible to ensure the body’s resistance to the measles pathogen. The effect of the drug can be combined, i.e. it can also prevent infection with rubella and mumps. Thus, the measles vaccine provides comprehensive protection against a number of unpleasant and dangerous infections.
Adult vaccination schedule
Vaccination against measles is no less important for adults. It is better to have it at an older age than to avoid it altogether. The need for this is due to the severity of the symptoms of the disease in adult patients. In addition, such manipulation is prescribed for medical workers and military personnel. For adults, there are also two stages of the procedure. The interval between them is three months. In this case, the vaccination is combined with the following vaccines:
- rubella,
- chicken pox,
- mumps.