More than 90% of people on our planet are carriers of the herpes simplex virus types 1 and 2. This means that vaccination against herpes is necessary for almost every person who has no contraindications. Vaccination against herpes is the administration of an antigen vaccine with the aim of inducing immunity that will prevent the disease or reduce its negative consequences.
At the ON CLINIC International Medical Center, the high-quality drug “Vitagerpavak” is used for vaccination - the world’s only polyvalent vaccine for the treatment of chronic herpesvirus infection (CHI) of the first and second types. Vaccination against the herpes virus will help reduce the frequency of recurrences of herpes infection. A vaccine containing an inactivated virus is injected into the body. As a result of vaccination, long-term resistance (resistance) of the body to herpes viruses is formed.
Who needs vaccination against herpes
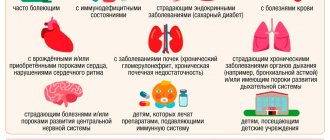
Vaccination against herpes virus types 1 and 2 is indicated:
- patients with frequent relapses of herpes (up to four to six or more times a year);
- patients with a generalized nature of the disease with the spread of the rash to new areas of the body;
- women planning pregnancy, if they have a history of frequent relapses of infection;
- patients without clinical manifestations of herpes, but with a high titer of antibodies to the virus according to a blood test.
Vaccination with Vitagerpavak suppresses the activity of the virus and it goes into a “dormant” state, which prevents the appearance of rashes on the skin, mucous membranes and the development of complications. Often after vaccination, the manifestations of the disease completely stop. If manifestations of herpes do occur, the disease proceeds in a milder form, the rashes disappear faster, and the intervals between relapses of the disease increase significantly.
Methods for preventing herpes zoster
In patients with reduced immunity, in case of contact with a patient with chickenpox, it is recommended to administer human immunoglobulin or immune plasma. The drugs reduce the risk of developing shingles, but they are most effective when used within the first 96 hours after exposure.
Vaccination against herpes zoster with the Zostavax vaccine can be carried out in people over 60 years of age. It is performed once and reduces the risk of developing Herpes zoster by 51%, and also reduces the intensity of pain by 61%, and the likelihood of postherpetic neuralgia by 66.5%.
How is vaccination against herpes carried out?
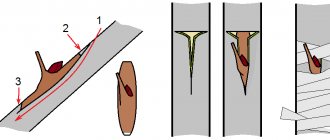
The vaccine against herpes infection is administered intradermally into the inner surface of the forearm in a single dose of 0.2 ml. The main vaccination cycle consists of five injections, which are given at intervals of one week. A repeat cycle is carried out after seven to ten days according to the same scheme. Six months later, a second course of vaccination is carried out, which consists of two cycles of five injections.
Patients with a severe form of herpes infection (when relapses of the disease are observed monthly or once every two to three months) are vaccinated against the herpes virus at intervals of at least ten days.
Contraindications to the use of herpes vaccines
Like any medications, vaccines have their own indications for use and contraindications.
Zostavax and Shingrix are not prescribed to patients with the following conditions:
- ARI/ARVI (respiratory diseases)
Any respiratory disease (including open tuberculosis) or other active infections that are accompanied by fever are a contraindication for vaccination.
The vaccine can be administered to patients with an extremely mild course of acute respiratory infections/ARVI, which are not accompanied by severe symptoms.
The decision to delay vaccination depends on the severity of symptoms and the etiology of the disease.
- Immunodeficiency
Vaccination is not carried out for patients with severe forms of immunodeficiency:
- acquired immunodeficiency syndrome (AIDS)
- Bruton's disease (agammaglobulinemia)
- human immunodeficiency virus (HIV)
- hypogammaglobulinemia
- IgA deficiency
- severe combined immunodeficiency (SCID)
- neoplastic processes
In addition, vaccination is not prescribed to patients undergoing chemotherapy and treatment with corticosteroid drugs.
- Pregnancy
Vaccination with Zostavax and Shingrix is contraindicated for use during pregnancy.
The main reason is the lack of adequate studies that could show the effect of drugs on the fetus and the ongoing pregnancy.
- Breastfeeding (lactation)
The manufacturer recommends that vaccination be prescribed to patients during lactation with extreme caution.
Many experts recommend avoiding vaccinations during breastfeeding or temporarily stopping breastfeeding.
Nothing is known about the possibility of the active ingredients passing into breast milk.
- Hypersensitivity to gelatin and neomycin
The vaccines do not contain preservatives, but do contain residual amounts of neomycin.
Therefore, these drugs are not recommended for use in patients with hypersensitivity to neomycin.
Also not recommended for patients allergic to gelatin.
Intramuscular or intravenous administration of smallpox vaccine is not recommended.
The vaccine is intended for subcutaneous administration only, preferably in the shoulder area.
Side effects of the herpes vaccine
After vaccination, local and general reactions may develop. Locals make themselves felt by slight redness of the skin up to two centimeters in diameter, and a slight burning sensation may be felt at the injection site. General reactions to vaccination in rare cases are expressed in the form of a slight increase in body temperature and short-term increased drowsiness. All of these symptoms usually do not require medical attention.
If more pronounced local and general reactions occur or if herpes worsens, you should consult a doctor. Repeated stages of vaccination are carried out only after the complete disappearance of side effects.
Adverse reactions of Zostavax and Shingrix vaccines
The most common side effects of the drugs (which can affect more than 2 in 10 people) are reactions at the injection site, such as pain, redness and swelling.
In rare cases, other manifestations of a general reaction may be observed.
These are chills, fever, muscle pain, fatigue, headache, digestive system upset (nausea, vomiting, diarrhea and stomach pain).
Most of these effects last 2 to 3 days, and usually do not require special treatment.
Complications of herpes
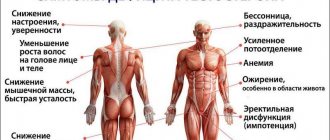
According to World Health Organization estimates, a continuously relapsing form of herpes with clinical manifestations six times a year occurs in 60% of infected people and can lead to the development of secondary immunodeficiency. Complications can affect almost all systems and organs, causing the following diseases:
- keratitis, iridocyclitis, corneal opacity;
- esophagitis;
- pharyngitis;
- encephalitis;
- meningitis;
- peripheral neuritis;
- herpetic urethritis, herpetic cervicitis, erosion of the anterior urethra;
- herpetic pneumonia, herpetic hepatitis.
The development of these diseases can be prevented by timely vaccination against herpes infection.
Trust your health to professionals! ON CLINIC
Vaccination No. 1
The most important vaccinations for people over 60–65 years of age are against influenza. This infection causes severe stress on the body at any age, but it is especially dangerous for older people. After all, their state of health usually leaves much to be desired, and therefore they suffer from the flu more severely. After all, an increase in body temperature and an increase in blood clotting, typical for influenza, contribute to the exacerbation of existing diseases in them.
Article on the topic “The virus behaves viciously.” Why get a flu shot? Unfortunately, there are many prejudices about vaccinations in society. You can often hear stories about people who got vaccinated against the flu, but still got sick. And much stronger than last year, when I was not vaccinated. Such stories are typical misconceptions. During the seasonal epidemic rise in incidence, people suffer not only from the flu, but also from acute viral infections (ARVIs) - they are caused by adenoviruses, rhinoviruses, rhinosyncytial viruses, etc. A person vaccinated against the flu may well get sick from any of these ARVIs. Sometimes they can be similar to the flu. Therefore, people sometimes complain about the uselessness of vaccination, not realizing that they did not have the flu.
My patients often ask: if the influenza virus changes every year, how can a vaccine protect against it? Doesn’t it become outdated? The fact is that the flu vaccine is also updated every year. The flu that comes to us in the Northern Hemisphere originates in the Southern Hemisphere, and epidemics there develop during summer. World Health Organization specialists are tracking which strains of the influenza virus are coming to us from the Southern Hemisphere, and are preparing a vaccine against them.
Flu nuances. What misconceptions about this ARVI are still strong? More details
Difficult vaccination against herpes simplex
The third vaccination, which should be given in old age, is against the herpes simplex virus. This is very important for many reasons, including protecting blood vessels. Such vaccination is necessary primarily for those who have manifestations of herpes infection. Most of us are carriers of the herpes virus, but not everyone gets it. Symptoms of the disease develop when the virus fits a person's immune system like a key to a lock. And if you get vaccinated, the vaccine makes the virus inactive. And this is very important, because the herpes pathogen, among other things, is in active form in the wall of blood vessels, contributing to the progress of atherosclerosis. Therefore, it is important to be vaccinated against the herpes simplex virus not only for cosmetic reasons (to avoid rashes on the lips), but also to prevent atherosclerotic damage to the arteries, and therefore to avoid heart attacks and strokes.
Article on the topic
The virus is omnipresent. Herpes is the cause of Alzheimer's disease, heart attack and stroke. Another important effect of such vaccination is protection against chronic fatigue syndrome. According to the latest data, it is also caused by the herpes virus. This syndrome is not just fatigue that goes away after rest or vacation, but a real infectious disease.
It is characterized by an acute onset, like the flu. People usually think it's really the flu or a bad cold. After such viral infections, a so-called asthenic “tail” remains - for a week or more a person feels weak, tired, and easily fatigued. But gradually the condition improves and the person returns to normal. And with chronic fatigue syndrome, asthenia lasts for years. And getting vaccinated against herpes helps prevent it.
It is important to understand that the decision about such vaccination should be made by a doctor, a herpes specialist, since there are special restrictions when prescribing these vaccinations. And they are introduced repeatedly, and not once, like others. The vaccination process itself sometimes lasts more than six months, but its effect is very important for the health of older people.
How to prepare for vaccination?
Vaccination against herpes does not require special preparation. The main stages are:
- consultation with a therapist to identify possible contraindications;
- taking tests to detect antibodies;
- visiting additional specialists if indicated.
Vaccination at the Pediatrician and Me clinic is carried out by qualified doctors. All patients are required to undergo a preliminary examination. If there are contraindications, vaccination is postponed until the person recovers.
Possible side effects
Vaccination against herpes is easily tolerated by patients. Side effects may include the development of a local reaction. In this case, painful redness occurs at the injection site, which can reach a couple of centimeters in diameter. A small percentage of patients may experience a slight increase in temperature and a feeling of drowsiness. All of these symptoms do not require medical intervention and go away on their own within a couple of days. It is necessary to seek help only if the reaction to the vaccine lasts much longer or is accompanied by an intensification of the reaction. Re-administration of the vaccine is possible only after all negative symptoms have completely disappeared.
How does the herpes virus types 1 and 2 manifest?
The herpes virus type 1 in most cases causes rashes on the lips and under the nose. It can also cause the formation of ulcers around the eyes and even near the nail plate. The second type of herpes is called genital. It manifests itself in the form of rashes on the genitals and groin. In this case, the patient experiences severe itching. However, as research shows, different types of herpes can change their location. For example, genital herpes can affect the area around the mouth, causing a "cold" and causing severe discomfort.
Possible complications
The herpes virus is not as harmless as it might seem at first glance. In 60% of the population, the disease develops into a recurrent form with clinical manifestations more than 6 times a year. In this case, the risk of developing secondary immunodeficiency increases several times. Complications can affect a variety of organs and systems. In this case, the following diseases may develop:
- pharyngitis;
- encephalitis;
- esophagitis;
- meningitis;
- damage to the cornea of the eye;
- neuritis;
- pneumonia;
- hepatitis, etc.
The introduction of a herpes vaccine will allow you to avoid these complications. The Pediatrician and Me clinic invites you and your children to get vaccinated at any time convenient for you.