Fear of vaccines is largely due to outdated beliefs about vaccines. Of course, the general principles of their action have remained unchanged since the time of Edward Jenner, who was the first to use vaccination against smallpox in 1796. But medicine has moved very far forward since then. So-called “live” vaccines, which use a weakened virus, are still used today. But this is only one of the types of means designed to prevent dangerous diseases. And every year – in particular, thanks to the achievements of genetic engineering – the arsenal of immunologists is replenished with new types and even types of vaccines.
What is vaccination and vaccination
A vaccination is the introduction of a special substance into the human or animal body that stimulates the production of protective antibodies to a specific disease (for example, diphtheria, smallpox, coronavirus and others). Most often, the vaccine is administered by injection, although there are other methods, such as drops in the mouth.
Vaccination is the process of administering a vaccine, i.e. the same as vaccination. Vaccination is also called a mass event of administering vaccinations, for example, to children against tetanus and other diseases or to adults against coronavirus.
Vaccination is carried out in one or several stages. In this case, the next administration of the vaccine is called revaccination. This event is aimed at maintaining the immunity that was previously formed from the previous vaccine.
A vaccine is a solution that contains a substance or microorganism that stimulates the formation of immunity. As a result of the administration of the vaccine, the immune system begins to actively produce antibodies that will protect the body from the corresponding pathogen - bacteria, virus or fungus.
Dangers of vaccination
A few words should be said about the dangers of vaccination. Indeed, some people, especially children, may experience allergic reactions after receiving the vaccine. They are usually expressed in skin irritation, itching, and redness. However, it should be noted that:
- an extremely small percentage of children (less than 1%) exhibit allergies;
- the composition of vaccines improves every year and becomes more and more hypoallergenic (that is, safe for people with allergies);
- your primary pediatrician knows about all of your child's allergens and can suggest which vaccines he or she may be allergic to;
- an allergic reaction to a vaccine is nothing compared to the real disease.
Types of vaccines
There are several types of vaccines:
- Live means living viruses, bacteria or other microorganisms. They are in a weakened form, so they do not cause disease. However, within a few days after vaccination, a person may feel slightly unwell – fever, weakness and other symptoms.
- Inactivated (killed vaccine) – a solution with killed microorganisms. Today, such vaccines are rarely used.
- Chemical - they contain only individual parts of pathogens, for example, substances from cell walls.
- Toxoids are vaccinations that contain neutralized (inactivated) poison.
- Recombinant – vaccines whose active components are obtained as a result of genetic engineering.
- Synthetic – contain artificial components that stimulate the production of antibodies.
- Associated - vaccines that contain several components at once, for example, weakened and killed microorganisms.
Vaccination, or, as it is also called, inoculation, is the process of introducing a vaccine into the body. Vaccines historically got their name from the Latin word vacca, meaning cow. In 1798, the English physician Jenner noticed that if the contents of a cow's pox were injected into a person's skin, he would not get smallpox.
Vaccines are drugs that help create artificial specific immunity acquired during the vaccination process and necessary to protect the body from a specific pathogen.
Vaccines are made through complex biochemical processes from microorganisms, their metabolic products or individual components of a microbial cell.
A vaccine preparation containing certain doses of the pathogen, once in the human body, collides with blood cells - lymphocytes, resulting in the formation of antibodies - special protective proteins that remain in the body for a certain period of time. This could be a year, five years or more. This is associated with the need for repeated vaccinations - revaccination, after which stable long-term immunity is formed.
During a subsequent “meeting” with a pathogenic microorganism, antibodies recognize it and neutralize it, and the person does not get sick.
Each country in the world has its own calendar of preventive vaccinations. In our country, until recently, it included seven infections: tuberculosis, diphtheria, tetanus, whooping cough, measles, mumps (mumps) and polio. Since 1997, two more vaccines have been added to the compulsory vaccination schedule - against hepatitis B and rubella.
Vaccination is a preventive measure designed to protect against an infectious disease. Thanks to vaccination, many diseases have become completely harmless; we learn about the existence of some of them only from medical textbooks.
The first vaccination was carried out in 1796. The English doctor E. Dhenner inoculated several patients with cowpox, as he noticed that people who had cowpox did not get smallpox. The last case of smallpox was reported in 1977.
Infection is the introduction of pathogens into the human body, accompanied by a complex of reactive processes. After the penetration of microbes, the body begins to “protect itself” - it produces antibodies that actively “fight” pathogens.
After an infection, antibodies remain in the body, i.e. immunity is developed. If pathogens of the same disease enter the body again, antibodies neutralize them. A person who has suffered a certain infectious disease develops immunity to it, i.e. its natural “vaccination” occurs.
After suffering from certain diseases, lifelong immunity is developed. Sometimes vaccination must be repeated several times to develop lasting immunity.
Some vaccines only last for a few years and therefore need to be repeated. Before doing this, you should consult your family doctor.
Types of immunization
The basis of any vaccination is the use of natural mechanisms occurring in the human body’s immune system. A person is injected with either weakened pathogens of a certain infectious disease, as a result of which the body begins to produce antibodies (active immunization), or immediately ready-made antibodies against a given disease (passive immunization).
Active immunization is the administration of a vaccine to form long-term protection for the body. Live vaccines are contraindicated in patients receiving immunosuppressants, fever, or pregnancy.
When carrying out active immunization, the following is used:
- live
- or non-live vaccines.
Live vaccines are pathogens that have retained the ability to reproduce, but their effect is very weak. This vaccine is used against smallpox, polio, tuberculosis, yellow fever, measles, rubella and mumps.
A non-live vaccine contains pathogens that cannot reproduce but remain active enough to produce antibodies in the body. This vaccine is used to vaccinate against cholera, typhoid, paratyphoid, whooping cough and influenza.
There are vaccines against diseases whose pathogens produce poison (toxin). Such pathogens primarily include the pathogens of diphtheria and tetanus. The toxins they produce are neutralized and converted into toxoids used as vaccines.
Passive immunization creates temporary immunity in the body by introducing foreign immune substances such as antibodies. Doctors often use this type of immunization when they suspect tetanus.
Passive immunization weakens a possible infection, while active immunization protects against future infection. If diphtheria is suspected, simultaneous immunization is also used. Sometimes autovaccination is used for infectious diseases. An autovaccine, prepared by isolating bacteria from a sick individual and culturing them, is reintroduced to the patient to stimulate the formation of antibodies.
Passive immunization based on the introduction to the patient of foreign antibodies taken from vaccinated people or animals. The effect of such a vaccine begins in a few hours and ends after four weeks, since foreign antibodies, having entered the human body, are broken down.
Passive immunization is usually used in cases where a person has already become infected with a certain disease or the likelihood of infection is very high. A classic example of the use of passive immunization is vaccination against rabies.
Passive immunization does not protect against a specific disease, but only softens its course. Immune sera used to treat tetanus, measles, rubella, mumps, hepatitis and rabies are obtained from vaccinated people. Animal immune serum is used to treat diphtheria, botulism, gas gangrene, and poisoning by snake venoms.
A combination of immediate but short-lived immunity through passive immunization and long-lasting immunity through active immunization is possible. This type of immunization is called simultaneous immunization.
When is vaccination necessary?
The answer to this question mainly depends on the circumstances of the individual person's life.
At-risk groups
People who have to stay outdoors for a long time need to be vaccinated against tick-borne encephalitis.
Agricultural and forestry workers should be vaccinated not only against tetanus, but also against all zoonotic diseases.
People with weakened immune systems are advised to get flu shots.
If you are going to visit tropical countries, find out what diseases you need to be vaccinated against.
Vaccination of children
Children must be vaccinated against childhood infectious diseases. Vaccinations are recommended in accordance with a special vaccination schedule for children.
Is vaccination dangerous?
In children, the vaccine often causes a mild vaccine reaction, for example, a slight increase in body temperature, moderate soreness, redness and swelling at the injection site, and loss of appetite. Severe lesions are less common and are usually seen in children with chronic illnesses.
Such children are vaccinated in a hospital under the supervision of a doctor.
The most dangerous is passive immunization, when used, a foreign protein enters the patient’s body. If you have hypersensitivity to a foreign protein, serum sickness may occur. In mild cases, symptoms of serum sickness such as enlarged lymph nodes and urticaria are observed. In addition, allergic shock is possible, which is a common cause of death for the patient.
Who pays for vaccination costs?
Some vaccination costs (for example, for routine childhood vaccinations or tetanus vaccine in case of injury, etc.) are partially covered by the health insurance fund. Other special vaccines, for example, when traveling abroad, must be paid for independently.
Vaccination when traveling abroad
Before traveling to exotic tropical destinations (such as African or South American countries), you should obtain detailed information about required and recommended vaccinations.
The World Health Organization annually publishes requirements for the immune status of immigrants for all countries.
To clarify information about vaccinations, you can contact the embassy of a specific country.
National calendar of preventive vaccinations
Approved by Order of the Ministry of Health of the Russian Federation dated March 21, 2014 N 125n “On approval of the national calendar of preventive vaccinations and the calendar of preventive vaccinations for epidemic indications.” Annex 1
Immunization of the population in our institution
In Kerch Hospital No. 1 there is a treatment room No. 29, where immunization of the population is carried out.
All vaccinations are carried out free of charge, after consultation with a specialist doctor.
Invitations for vaccinations are carried out by local services, medical examination rooms, and preventive rooms.
Head outpatient department of clinical hospital No. 1 - Sharonova Irina Nikolaevna
Read also:
- Vaccination safety
- The procedure for professional vaccinations for citizens
- Vaccination. What you need to know
- Immunoprophylaxis of infectious diseases. Memo
- WHO. False ideas about vaccination
- “On immunoprophylaxis of infectious diseases”
- Recommendations for travelers
- National calendar of preventive vaccinations
- April 24-30 – World Immunization Week 2021
- Vaccine-preventable diseases
- Legislation on vaccine prevention for adults in the Russian Federation
- List of works requiring mandatory professional vaccinations
- Refusal to vaccinate
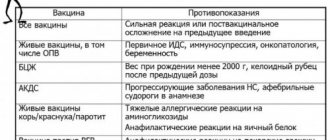
- Contraindications to vaccination
- Risk factors of the labor process and vaccination of the adult working population
- Vaccination against measles, rubella, chickenpox
- Vaccination against tick-borne encephalitis
- Vaccination against hepatitis B
- Vaccination against diphtheria and tetanus
- Vaccination against hepatitis A
- Vaccination against pneumococcal infection
- Flu vaccination
- Do you know what a vaccination is?
- European Immunization Week 2021: Vaccines deliver results!
- Vaccination against measles, rubella, chickenpox
Intramuscular vaccinations
In most cases, vaccinations are given intramuscularly. Muscle tissue is well supplied with blood, due to which the development of immunity begins very quickly. In addition, this method of administration practically does not cause allergic reactions or other side effects. Although the patient may feel some stiffness in movements for 1-2 days.
As a rule, intramuscular vaccinations are given in the anterior surface of the thigh (in the middle third). Injections are also given in the deltoid muscle, which is located above the head of the humerus bone. The injection is placed at a right angle (perpendicular) to the surface of the skin.
Limitations in the use of the vaccine
An attenuated vaccine is one that is contraindicated in the following cases:
- The period of bearing a child.
- Acute diseases of infectious and non-infectious nature.
- Exacerbation of chronic pathologies.
- Immunodeficiency states.
- Blood cancer, the appearance of malignant neoplasms.
- Undergoing radiation therapy.
- Taking immunosuppressants.
- Tendency to severe allergic reactions.
- Development of complications from the previous vaccination.
Oral vaccination
The vaccine can also be taken orally. In this case, the patient takes the vaccine in the form of drops. The method is used to develop immunity against diseases such as polio and typhoid fever. In some cases, the drops have an unpleasant taste. They are diluted with water or dripped onto a piece of cookie or sugar to be eaten.
The advantages of this method are obvious - painlessness, quick administration, convenience for the patient and the doctor. However, the accuracy of the dosage is difficult to calculate, since part of the vaccine can be excreted in the feces.
Safety
An attenuated vaccine is one that activates all components of the immune system, which provides long-term protection against infectious diseases. Since it contains living microbes, there is a certain risk of developing pathologies. Of course, the risk of microbes becoming able to return to a pathogenic form and provoke the development of the disease is quite small, but in extremely rare cases the following side effects may appear:
- VAPP or vaccine-associated paralytic polio.
- Poliovirus.
- Local lymphadenitis, disseminated BCG infection.
- Retrovirus.
People with HIV cannot respond adequately to vaccination; their risk of developing adverse reactions is quite high. It is not recommended for women to get vaccinated while pregnant.
An attenuated vaccine is one that has a high risk of vaccination errors. Some vaccines, for example, come in dry powder form. They must be diluted with a special solvent before administration. In this case, doctors may make a mistake by using the wrong solvent or medication. Many vaccines require medical attention to maintain the cold chain in order for them to remain active.
Thus, the risk of developing pathologies comes down to the following:
- The ability of microbes to return to a pathogenic form.
- Possibility of using time for people with HIV.
- Risk of developing infections.
- Procedural errors.
- Vaccine administration during pregnancy.
Intradermal and cutaneous vaccinations
These are vaccinations that are administered using a syringe. But the injection is not given into a muscle, but into skin tissue, for example, in the forearm. As a rule, a similar method is used to develop immunity against such diseases:
- smallpox;
- BCE;
- tularemia.
When administering the vaccine, the needle is directed along the skin (parallel) so as not to get into the underlying tissue. As a result, the skin at the injection site becomes whitish. If there are no such signs, it means that the vaccine was administered incorrectly.
The intradermal vaccine is administered almost painlessly. But the vaccination technique itself is complex and requires the experience of a medical professional. If the vaccine is administered incorrectly, complications may occur.
Subcutaneous vaccination
This is an injection of the “under the shoulder blade” type. The method is used for vaccination against diseases such as yellow fever, measles-rubella-mumps and others. Subcutaneous vaccination is performed for patients with blood clotting problems. If the vaccine is administered intramuscularly, it may cause bleeding.
The vaccination is quite simple and relatively painless, the dosage can be determined quite accurately. At the same time, the rate of formation of immunity is low, redness, thickening of the skin and other local reactions are possible.