In what year and who carried out the first vaccination in the world?
In 1796, the English doctor E. Jenner drew attention to the fact that farmers who work with cows, if infected, suffer from smallpox.
This theory needed to be tested. Having decided to conduct a revolutionary experiment at that time, the doctor injected cowpox into the boy, proving that he had developed immunity to the natural disease.
Attempts were made to infect the guy with smallpox, but they were all unsuccessful.
This is how vaccination appeared. This term began to be used a little later. The English doctor E. Jenner made a revolutionary push in medicine, but only a century later, a scientific approach to vaccination was taken.
In 1881, Louis Pasteur conducted a public experiment on animals to prove the correctness of his discovery. Dozens of sheep and cows were infected with anthrax, and half of them were given the vaccine. After 24 hours, the unvaccinated animals died from the disease, while the others remained alive. This experience was witnessed by many people, which became one of the scientist’s triumphs.
From the history of vaccination: the first vaccination experiences
Even in ancient times, doctors noticed that people who had had smallpox once did not get it again. In connection with this understanding, doctors from different countries began to practice the methods of the first “primitive” vaccinations.
For example, in Ancient China, an immune response to smallpox was produced using smallpox biofragments, which were placed in the patient’s nostrils. The person fell ill in a mild form, and in return received lifelong protection from the disease.
Domestic doctors began to practice a similar method at the beginning of the 18th century. This practice involved rubbing contents extracted from the smallpox blisters of infected people onto the patient's skin. It is interesting to know that Catherine II was one of the first to decide on the experiment. The Great Russian Empress also allowed her son Peter to be vaccinated.
1976 became a turning point in the history of vaccination. The English scientist E. Jenner called on society for mass vaccination. During his speech, the doctor argued: farmers who come into contact with cows suffering from smallpox do not become infected from people. Thus began a new history of vaccinations.
The scientist did something that no one had dared to do before. He inoculated the child with cowpox, and in the future his patient became immune to the disease. The scientific basis for the effectiveness of immunoprophylaxis appeared only a hundred years later, but the first successful attempts, although not interpreted from the point of view of official medicine, saved many lives.
Who created the cholera vaccine
In 1880, Louis Pasteur found a way to protect against infectious diseases by introducing weakened pathogens.
He was the first to prove that infectious diseases arise as a result of the penetration of microbes into the body from the external environment.
Louis Pasteur worked with the bacteria that causes chicken cholera. His preparations contained a high concentration of them, and when administered to birds, they died within the first day.
Once, by mistake, while conducting his experiments, Louis Pasteur used an injection with bacteria that was a week old, which provoked the disease in chickens, but the course of cholera was mild, after which they did not die and recovered.
The scientist considered that the vaccine he had administered was spoiled and made a new one, after which he administered it to the experimental subjects. Further observation of them did not lead to the usual result. Such an experiment made it clear that the process of infecting chickens with weakened bacteria contributed to the development of a protective reaction in them and prevented the development of the disease.
Nowadays, the following cholera vaccines are widely used:
- WC/rBS. This vaccine provides 90% protection against cholera, regardless of age, for 6 months after using two dosages with a one-week break.
- WC/rBS modified. It does not contain a recombinant B-subunit. The vaccine must be used in 2 doses with a 7-day break.
- CVD 103-HgR. A single dose provides strong protection against cholera. After 3 months it was 65%.
The first working vaccines were invented in the late 1800s and became widely used among the population. The cost of vaccination against cholera in different countries varied from 0.1 to 4 dollars.
Trust in the needle
Things were very similar with other diseases. With the only exception that at that time there were no vaccinations against the main “childhood” diseases like whooping cough, measles or diphtheria. Accordingly, the “evil doctors” did not in any way annoy either the disease or the people who lived in such “normal natural conditions.”
Article on the topic
Gunpowder and worms. How the first pharmacies were set up in Rus' The newspaper “St. Petersburg Vedomosti” for 1869 can tell you what happens in such cases - a significant part of the issues of this publication was devoted to the outbreak of “malignant toad” or diphtheria in the region of the Don Army: “Children from 1 year and even young people up to 18 years old die in three days in huge numbers. In the Khopyorsky district alone, death has kidnapped more than 8,000 children this summer. There are farms where literally the entire younger generation has died out.” This is only among the Cossacks. For ordinary peasants, who lived worse and poorer, things were completely bad - more than half of the children suffered from diphtheria, and exactly a third died. And this is only during the 1869–1870 season. In general, outbreaks of diphtheria were observed approximately every 4 years. And they mowed down the children with terrifying consistency.
When diphtheria serum was finally used in our hospitals 25 years later, the situation improved. Now, out of 100 sick people, not 30–50% died, but only 10–12%. The most interesting thing is that treatment with that serum, unlike the current relatively harmless vaccinations, gave really serious side effects - fever, severe chills, disruption of the heart and even convulsions. But for some reason, the parents of that time put up with these inconveniences. Here is the report of the Chief Medical Inspector for 1903: “Injection of serum was widely used, to which measure the population, more than aspirations, treated with great confidence and willingly went for injections.”
Martyrs of science. How doctors inoculated themselves with diseases Read more
Comparing the situation of those times and the present, one involuntarily asks the question: is it really necessary to convince parents of the benefits of vaccinations either a heavy government hand, or a truly formidable epidemic with the number of deaths no less than half?
Who invented the rabies vaccine
The rabies vaccine was invented in 1885 by French chemist and biologist Louis Pasteur. At that time, this disease ended in death in 100% of cases. After the invention of the vaccine, the scientist for a long time did not dare to test its effect on himself, and when he was about to do this, a nine-year-old boy was brought to him, completely bitten by a dog. He had no chance to survive. No one believed in the child’s recovery, but after vaccination, in front of many people and the press, the patient recovered, which brought the scientist world fame.
Types of immunization and vaccines
Before talking about the types of immunization, it is worth understanding what it is. The very concept of Immunization is understood as inducing a response from the body's immune system to an infection or disease. Now, based on all this, active and passive immunization are divided. With passive, substances or antibodies are introduced into the body that help the immune system fight infection. With active immunization, a mild infection is introduced into the body, which the immune system will overcome on its own.
Read: Giant anteater as an insectivorous animal of America
The essence of the vaccination procedure
The essence of the entire vaccination procedure is to give a vaccine to a sick or healthy body in order to achieve immunization. Vaccinations vary in structure. Most vaccinations are given to a healthy body to prevent it from becoming infected in the future. But there are diseases in which vaccination is used when the body is already infected. For example, rabies in humans. The rabies vaccine is given to a person after the body is infected. Louis Pasteur gave the first vaccination to a child who was bitten by a rabid dog. He noted that after a bite, with the introduction of antibodies at regular intervals for 14 days and proper care of the wounds, the person fully recovers.
Read: Bengal cat as the first domesticated by man
Vaccination methods
Vaccinations can be administered to the body in a variety of ways. Of course, most vaccinations are administered through an injection, but there are other ways. Vaccines that may not be absorbed by the intestines are administered through injection. Some vaccines can enter the body through the mucous membrane. At the same time, there are vaccines that are administered orally, i.e. swallowing. For example, the vaccine against polio and cholera is administered orally because it has been established and proven that the intestines absorb it well.
Read: Goliath frog as the largest frog in the world
Types of vaccines
As for the vaccine itself, it can be of four types depending on the type of antigenic material:
- A vaccine that contains weakened infections, diseases or viruses (tuberculosis, polio);
- Vaccination with dead infections or viruses (rabies, tick-borne encephalitis);
- Weak or altered toxin organisms (diphtheria or tetanus);
- Synthetic or genetically engineered vaccines (whooping cough and meningitis).
Inoculation, Vaccination and Immunization are the same in their meaning and ultimate purpose and in their essence are synonymous, but different in their effect on the body.
Read: Wild boar as a representative of mammals of Eurasia
Creator of the polio vaccine
The first vaccination against polio took place on February 23, 1954. Before its appearance, approximately 40% of patients were crippled by paralysis, and 10% died from respiratory failure. To save people's lives, they used chambers where air pressure changed. In such conditions, the patients lived out the rest of their days.
The first polio vaccine was created by American virologist Jonas Salk, but he was not initially interested in polio. After training to become a doctor, the scientist realized that he wanted to become a microbiologist. During the war, Jonas Salk took part in the development of a vaccine against influenza and was able to discover a new strain.
The National Foundation Against Infantile Paralysis helped him conduct a full-scale study. With financial support from them, specialists were able to breed viruses in monkey kidney cells and purify them using antibiotics.
In 1952, Jonas Salk tested the vaccine on himself and his loved ones, filming the entire process. The footage would later be used as a sedative for children being vaccinated against polio. The procedure was successful and did not cause any allergic reactions.
On February 23, 1954, Jonas Salk and several doctors vaccinated 5 thousand schoolchildren in Pittsburgh with an unknown drug. The collected tests showed the presence of antibodies, and on April 26, health officials allowed more than a million children to be vaccinated.
Contributions of other academic doctors
In 1919 Scientists from France first demonstrated a drug that was used as a vaccine against tuberculosis. After testing was completed, five years later, the vaccine was widely distributed. In the Soviet Union, foreign medicine significantly reduced incidence and was used to prevent tuberculosis in the population, starting from the first days of infants’ lives.
At the turn of the 19th century, merciless cholera raged in Russia and Europe. In just one year of the epidemic, the disease claimed the lives of 300 thousand people. Thanks to our compatriot Vladimir Khavkin, known as a follower of Pasteur, society coped with a common disaster. The scientist developed an effective vaccine, which he bravely tested on himself, and then introduced volunteers to the experiments. The result confirmed expectations: the epidemic and deadly cholera has receded.
The history of the creation of vaccinations did not stop there. Scientists later developed vaccines against plague, measles and other deadly diseases.
Who invented a remedy for the prevention of tuberculosis?
BCG is a vaccine against tuberculosis. Its creator is two French scientists: Guerin and Calmette.
The discovery took place in 1923, but the distribution of this remedy occurred only after several years.
The vaccine contains a strain of bovine tuberculosis bacillus grown in an artificial environment.
It causes a mild illness so that a person develops immunity to it.
Prospects for the development of Vaccination
In general, Vaccination brings enormous benefits to society in a variety of ways. According to WHO estimates, today 2-3 million people die from diseases per year, 1.5 million of them are children. They estimate that 29% of the deaths of children aged 1 to 5 years could have been avoided if they had been vaccinated. Vaccination has led to a significant reduction in the prevalence of a large number of infectious diseases. Developing vaccines is extremely expensive. Developing a vaccine for one serious disease costs about $2.8 to $3.7 billion. No matter how sad all this may sound, many diseases and infections still remain invulnerable to medicine. Today, vaccines are being developed for diseases such as HIV, Ebola and many others.
The World Health Organization periodically reports that medicine has completely defeated this or that disease. For example, there have been no cases of smallpox for a very long time, and there have been no cases of polio since 2013. If you face the truth, you will notice that people get sick with serious illnesses from time to time and nothing can be done about it. The only effective way to eradicate diseases and prevent epidemics is vaccination, which must be performed without fail. Take care of your health.
The first specialized immunological institutes
At the end of the 19th century, the first specialized immunology laboratories appeared, and already in the 20th century the first immunological society and departments of research institutes arose.
Immunology developed quite quickly and received public recognition not without the help of many experiments conducted by scientists and external contributions to the development of this field.
The work of immunologists was initially carried out in microbiology institutes. The very first specialized immunological institution is the Paul Ehrlich Institute, located in central Germany in Frankfurt.
When did vaccinations begin everywhere?
History of the first mass vaccinations:
- 1957 - it was decided to vaccinate against whooping cough in the first year of a child’s life, and mass vaccinations were carried out for children under five years of age.
- 1960-1961 - mass vaccination of adults and children against polio.
- 1967 - Mandatory tetanus vaccine for children was introduced.
- 1968 - A massive measles vaccination campaign was carried out.
- 1973 - routine vaccination against measles in the first year of a child’s life.
- 1980 - smallpox ceased to exist, and therefore the vaccine that protected against it was completely abolished.
- 1998 - it was decided to introduce a two-time vaccination against rubella, as well as re-vaccinate against measles and hepatitis B.
- Since 2001, adults and children have been re-vaccinated against measles, hepatitis B and rubella.
- 2011 - vaccination of children at risk of hemophilus influenzae infection was carried out.
- 2014 - vaccination against pneumococcal infection.
What pandemics do vaccinations save from today?
Today, medicine has hundreds of vaccines against various diseases. Whooping cough, diphtheria, tetanus, rubella and other infections, thanks to the work of scientists, no longer pose a serious danger.
Tuberculosis
BCG vaccination is given against tuberculosis. Vaccination protects children from infection, but even if a child becomes infected, the disease is mild. The drug is administered according to the National Preventive Vaccination Calendar.
The vaccine was created by French scientists Guerin and Calmette in 1919, who received the Nobel Prize for their work. However, the first drug had errors - in liquid form the vaccine quickly lost its properties. Subsequently, it was refined by Soviet scientists. They managed to create a dry mixture that is dissolved before being administered.
Hepatitis
The main goal of immunization is to prevent viral infection with chronic hepatitis B and severe complications, including liver cirrhosis and the development of cancer.
The infection has a wide geography. According to WHO, more than 2 billion people are infected in the world today. 360 million of this number are chronic carriers of hepatitis.
The vaccine was included in the preventive vaccination calendar in 1991. for children (for adults - in 1995).
Whooping cough, tetanus, diphtheria
DTP is given to all children in Russia. In addition to whooping cough, it is used to prevent tetanus and diphtheria. The drug has imported analogues, which are designed to develop immunity to a larger number of diseases.
The whooping cough vaccine was created by Bordet and Zhangou in 1912. Scientists have invented a drug based on bacteria destroyed by high temperatures.
Pneumococcal infection
In the Russian Federation, vaccination has been mandatory since 2014. With its help, society has developed mass immunity to diseases caused by the pneumococcus bacterium.
Science identified the pathogen in 1881. The infection received its name in 1886. Work on creating a vaccine began in 1911, but the first successful vaccination was injected only half a century later, in 1960.
Rubella
The drug is prepared based on the Wistar RA 27/3 virus strain. The vaccine is grown in the laboratory based on human diploid cells. The body receiving the drug produces IgG antibodies. The rubella vaccine provides protection for 16 years or more.
Before scientists developed the vaccine, the disease killed about 2.6 million people every year.
The pathogen was identified in the period 1961-1962. Scientists Neva, Parkman and Weller worked on this at the same time. Vaccine prototypes appeared in the early 70s.
Measles
The first combination vaccine against measles was created in 1971. In 2005 a component was added to the drug, thanks to which the vaccine today works as a “4 in 1”: against measles, mumps, smallpox, rubella.
Measles vaccination became part of the vaccination schedule in 1994. Until mass immunization began, the incidence of disease in the world was on a global scale: almost every person suffered from the disease.
Haemophilus influenzae infection
Act-HIB is a vaccine created by scientists in France. Today, the main supplier of the drug is Belgium, which produces an analogue of the previous version. In Russia, immunization has been carried out not so long ago.
It is important to vaccinate children under one year of age against hemophilus influenzae infection. This is a dangerous disease that occurs with the symptoms of a common acute respiratory infection, but has much more serious complications: purulent inflammatory processes in the fatty tissue of the face, arthritis, sepsis, etc.
Coronavirus
In 2021, the history of the development of vaccinations was updated - the database was replenished with drugs used to prevent coronavirus infection.
Russian scientists have developed more than 20 types of coronavirus vaccinations. Most drugs today are at the stage of clinical trials. Among other vaccines, two leaders have emerged - EpiVacCorona and Sputnik V. These drugs have been successfully tested. They are already used for mass immunization of the population in the Russian Federation.
Sputnik V is effective in 91.4 percent of cases. EpiVacCorona is considered safer for patients over 60 years of age, since the drug does not contain viral particles and, accordingly, does not provoke adverse reactions.
Modern methods for creating immunobiological drugs
In recent years, immunologists have discovered new and more effective ways to develop vaccines. Among them:
- Genetic immunization (or DNA vaccination). It involves the introduction into the body not of an antigen protein, but of a nucleic acid in which information about the protein is encoded. The required gene is inserted into a safe virus or DNA ring, after which the carrier enters the cell, where it synthesizes proteins. Next, the cell independently produces vaccines directly inside the body. The effect lasts for up to two years, providing complete immunity with high protection against viral infections.
- Reverse vaccinology. This method is the absolute opposite of the previously used one, when the creation of vaccines proceeded from the whole microorganism to its components. Reverse vaccinology involves a path from the genome to its products. It takes no more than a few weeks to determine the nucleotide sequence of the genome. Thanks to recombinant technologies, a weakened virus can now be obtained in a shorter time. To do this, a gene is cut out from the genome of the virus, which is responsible for pathogenic properties, however, it does not affect immunogenicity or reproduction. The resulting viral strain is used to make a vaccine.
The creation of vaccines is an important stage in the development of medicine. It took a lot of time to develop them, and not so long ago they began to be widely used and became mandatory.
Due to vaccination in childhood, the number of people suffering from certain dangerous infectious diseases has significantly decreased, which further confirms its importance.
Who invented vaccinations?
“Treat like with like” - have any of our readers come across this principle? Surely many people know that this is about homeopathy.
But this is not about her. Try to imagine what else could be said using this approach? Let's not languish: with some assumption - about vaccinations.
“What does something like this have to do with it?” - you ask? Let's find out.
Ancient, even more ancient...
Immediately the question is: what do a vaccine and... a cow have in common? Hint: the Latin word for “cow” is “vacca”. It is from this word that the term “vaccine” originates. It was proposed by the French microbiologist and chemist Louis Pasteur. He did this in honor of the doctor Edward Jenner, known in the world of medicine and in the history of vaccination as the creator of vaccine prevention.
Edward Jenner
The 18th century was drawing to a close. Jenner, while in the village, noticed that farmers who farm cows infected with cowpox do not get smallpox, a terrible infectious disease that “mowed down” millions of people when the epidemic occurred.
Apparently, the doctor made a connection between these facts and decided to inoculate the boy with cowpox. After a bold experiment, the boy also became resistant to this infection.
AGAINST THE BACKGROUND OF EPIDEMIOLOGICAL WELFARE, PEOPLE OFTEN REFUSE VACCINATIONS. AS A RESULT, INFECTIONS THAT WERE CONSIDERED ERADICATE ARE RETURNING
At that time, representatives of the microworld had not yet been studied. The method itself is widely distributed throughout Europe, and later, thanks to it, smallpox is eradicated on a global scale.
A century later, Jenner's idea was developed and improved by Louis Pasteur, who later created a vaccine against rabies.
Read the material on the topic: Living according to your dreams. The great discovery of Louis Pasteur
So it's the 18th century? As it turned out, not quite so. Long before Jenner and Pasteur, so-called inoculation was carried out in India and China - inoculating healthy individuals with liquid from the blisters of patients with a mild form of smallpox. The technique was far from perfect: the virus, although less dangerous, sometimes still led to death. In addition, it also happened that a highly pathogenic pathogen was mistakenly introduced. Later, a similar principle of grafting began to be practiced in Europe and America.
At the beginning of the 18th century, one of the methods of protection against smallpox was brought home from Turkey by the wife of the English ambassador.
Despite the positive reviews, few dared to use the “Turkish protection”: no matter how obvious the benefits of such a “vaccination” were, people were very afraid of getting sick with “real” smallpox. Nevertheless, there were brave men, including persons noted by the authorities.
Our country is also mentioned in the early history of vaccination. At the end of the 60s of the 18th century, the English doctor T. Dimsdal visited Russia. He was invited to administer smallpox vaccinations to Catherine II and her son Paul.
Read material on the topic: Catherine the Great: healthcare organizer, pediatrician and teacher
Thus, the idea of preventing like with like was, as they say, “in the air,” and Jenner was able to catch the “smell” of it.
Another interesting fact. A little more than 20 years before Jenner’s experience, which went down in medical history, an English farmer infected his wife and two of his children with cowpox. The neighbors were indignant. All three began to feel feverish, so a doctor's visit was necessary. However, when a smallpox epidemic occurred in the area, the farmer’s family members were not harmed, even though they had contact with the sick. In the early 90s of the same century, the Englishman’s experience was repeated by his Prussian “colleague,” also a farmer.
So who created the vaccines? As you can see, answering this question is not so easy. However, it was thanks to Jenner’s work that vaccine prevention became widespread. Its principles were later picked up and developed by other scientists.
What happens to the immune system when an infection enters the body: from disease to vaccine prevention
Once a pathogen enters, the cells of the immune system react to it. The components of the agent that are perceived by the body as foreign and cause a specific response from the immune system are called antigens. The products of the immune response are antibodies and immune cells that can attack the infectious agent.
After its elimination, the “trained” immune system remains ready for a new encounter with the infection - with the difference that the next time it will respond immediately to the introduction of a microorganism.
Apparently, the same principle of protection was intuitively used by Jenner’s predecessors - with the difference that they took a cow rather than a human pathogen. Jenner himself wrote that these two varieties of smallpox are two forms of the same disease, and the transfer of cowpox makes one resistant to smallpox.
THE LAST CASE OF NATURAL SMALLPOX INFECTION WAS RECORDED IN SOMALIA IN 1977
A natural question may arise: isn’t such a “frontal” approach to creating immunity to infections in general too risky? If you think about it: a sick person releases pathogens that, when entering the body of another, are likely to cause illness. But this is no longer a vaccination, but a relapse in the literal sense of the word. And then: in the case of farmers and Jenner, the vaccination was done not with a human, but with a cow pathogen. Fortunately, it also caused protection from human ones. But what about other microorganisms, the “relatives” of which, relatively safe for humans, cannot be found in animals?
Change but keep
At the beginning of the 20th century, methods for the stable weakening of pathogens appeared. This eliminated the risk of disease, but retained the effect of creating protection.
Scientific progress has made it possible to obtain vaccines that can be divided into three groups:
- alive. Contain a weakened pathogen that cannot cause disease, but stimulates the immune system;
- inactivated. Contain a killed pathogen or parts thereof;
- toxoids - bacterial toxins in a modified, harmless form.
Further developments in the field of molecular biology and genetic engineering made it possible to create molecular vaccines that contain certain proteins or protein fragments of pathogenic pathogens.
Read the material on the topic: Are unvaccinated children the healthiest?
DNA vaccines. The principle of their operation is as follows. It is not the pathogen itself (weakened or killed) or its antigens that is introduced into the body of a person who is about to be vaccinated against any infection, but a section of its nucleic acid. A specially selected area is one along which the desired antigen protein is formed. In other words, a carrier is introduced in which information about the antigen is encoded. Once in a human cell, this nucleic acid begins to produce the necessary proteins. These vaccines are in the research stage. There are other approaches to vaccine technology.
After vaccination
Once in a previously vaccinated body, the pathogen has no chance, since the attack begins as early as possible after its penetration. Therefore, the body either will not get sick at all, or will suffer a mild form of the disease and without complications.
Practical results
Those of our readers who were born in the late 70s and later probably no longer have traces of the smallpox vaccine. Do you know why?
The last case of natural smallpox infection was recorded in Somalia in 1977. The next case was the last case of laboratory infection. And in the 80s it was announced that this infection had been eliminated. In the Soviet Union, vaccination was stopped in 1978-1982. Thanks to vaccinations, polio was completely eradicated in the United States by the end of the 70s.
Read the material on the topic: Polio is coming back?
Millennium
We all like closure on problematic issues. The total eradication of smallpox is one of these. However, in the early 2000s, US President George W. Bush ordered a vaccination campaign against smallpox among all military personnel. The reason is the distribution of anthrax spores (one of the most dangerous infections) and the threat of using smallpox as a biological weapon.
THANKS TO VACCINATIONS, BY THE END OF THE 70'S POLIOMYELITIS WAS COMPLETELY ELIMINATED IN THE USA
To date, only a few laboratories around the world are working with variola virus for research purposes.
Is it just an infection? Is it just prevention?
As it turns out, no. Today, vaccines are being developed for the treatment of chronic infectious pathologies (in particular, those caused by hepatitis B and C viruses, papilloma, human immunodeficiency), neoplasms (melanoma, breast or colorectal cancer), allergic or autoimmune diseases (multiple sclerosis, type I diabetes, rheumatoid arthritis).
When leaving, the disease looks back
Even if the present and future generations do not have to face the devastating epidemics of the past, the current situation is also far from ideal. Some respiratory tract infections, viral hepatitis B and C, tuberculosis, malaria, as well as relatively recently emerging threats in the form of the Ebola virus, HIV, coronaviruses and a number of other pathogens still pose a danger.
The situation is complicated by the fact that, against the backdrop of epidemiological well-being, people often refuse vaccinations. As a result, infections that were thought to be eradicated return.
IN THE MID-90s, AN OUTBREAK OF DIPTHERIA OCCURRED IN RUSSIA. AS A RESULT OF THE ANTI-VACCINATION CAMPAIGN, MORE THAN 100 THOUSAND WERE INFECTED. PEOPLE, SEVERAL THOUSAND OF THEM DIE
Over the past few decades, diseases of whooping cough, diphtheria, polio, and measles have been reported in Japan, Russia and some other CIS countries, and in certain Latin American countries. In 2011, almost all US states did not provide the required number of whooping cough vaccinations. As a result, 42 thousand people fell ill the next year. In the mid-1990s, Russia experienced an outbreak of diphtheria, which had previously only occurred occasionally. As a result of the “anti-vaccination” campaign, more than 100 thousand people became infected, several thousand of them died. The epidemic was stopped only thanks to mass vaccination of children.
Warn? Yes! Current state of the issue
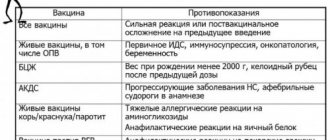
To date, a national vaccination calendar has been developed and is in effect. It regulates the frequency of vaccination of children depending on their age. The calendar includes vaccinations against infections such as viral hepatitis B, tuberculosis, polio, whooping cough, tetanus and a number of others.
Here's what the calendar looks like today:
Afterword
The progress of medicine in the field of prevention of dangerous infections makes it possible to avoid infection with them, or to suffer from a mild form of the disease. National vaccination calendars are periodically updated and supplemented. Largely thanks to vaccination, society is free from epidemics of one or another infection. Therefore, is it worth playing dice with fate by refusing vaccinations?
Text: Enver Aliyev