The causative agent of borreliosis is the spirochete Borrelia burgdorferi sensu lato
The causative agent of the infection is the spirochete Borrelia burgdorferi sensu lato complex, transmitted to the patient after a tick bite.
The infectious agent was first identified in the 80s in the USA, due to a massive outbreak of arthritis in children after visiting Lyme Park. The distribution area of borreliosis currently covers almost the entire temperate zone of the Northern Hemisphere. The main natural reservoir of the causative agent of borreliosis are small rodents inhabiting anthropogenic landscapes (primarily forest parks and pastures).
The carriers of borreliosis are ticks of the genus Ixodes. The transmission of the infectious agent is carried out by ticks of the genus Ixodes . In Western Siberia, the carrier is the pasture or taiga tick Ixodes persulcatus - the same one that transmits another dangerous infection - viral tick-borne encephalitis. In the European part of the country, the main vector is the forest tick Ixodes ricinus.
Borreliosis is one of the most common tick-borne infections in the world
Acute development of infection - fever, fever, headaches and muscle pain - is observed quite rarely. Much more often, the acute stage is practically absent, and the disease immediately becomes chronic. Under pressure from the immune system, borrelia go into tissues and organs where the activity of the immune system is reduced - nervous tissue, joints, tendons, heart.
Symptom of borreliosis – erythema migrans
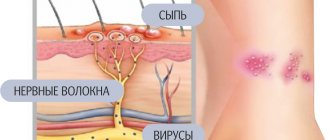
One of the main primary symptoms of borreliosis is erythema - redness of the skin around the bite site that expands over time.
Another defense mechanism for Borrelia is a change in the main antigens, which significantly weakens the effectiveness of the humoral immune response. Strains of Borrelia burgdorferi, found in different parts of the range, differ markedly from each other both in antigenic composition and in the symptoms that can be observed during the development of the disease. For example, B.garinii, which is dominant in the Novosibirsk region, often does not produce clearly defined erythema, which makes the symptomatic diagnosis of borreliosis in Novosibirsk especially difficult.
Currently, the disease is divided into three stages
- The first stage , local, includes local manifestations and usually lasts up to one month - intense erythema is observed at the site of the initial lesion, a vesicle and necrosis appear. In place of the former erythema, increased pigmentation and peeling of the skin often persists, secondary erythema, rash on the face, urticaria, transient pinpoint and small ring-shaped rashes, and conjunctivitis occur.
- After the initial manifestations, the disease enters the second stage , associated with the dissemination of the pathogen into various organs and tissues. In non-erythema forms, the disease often begins with manifestations characteristic of this stage of the disease and is more severe than in patients with erythema. During this period, serous meningitis, meningoencephalitis and syndromes of damage to the peripheral nervous system may be observed: sensory, predominantly algic syndrome in the form of myalgia, neuralgia, plexalgia, radiculoalgia; amyotrophic syndrome, isolated neuritis of the facial nerve, mononeuritis. The most common heart lesions are atrioventricular block (I or II degree, sometimes complete), intraventricular conduction disturbances, and rhythm disturbances.
- After 3-6 months, borreliosis enters the third stage , associated with the persistence of infection in any organ or tissue (unlike stage II, it is manifested by predominant damage to any one organ or system). Recurrent oligoarthritis of large joints is typical. Late lesions of the nervous system include encephalomyelitis, spastic paraparesis, ataxia, memory disorders, axonal radiculopathy, and dementia. Polyneuropathy with radicular pain or distal parasthesias is often observed. Patients report headaches, increased fatigue, and hearing loss. Children experience slower growth and sexual development.
THE INFECTION IS NOT TRANSMITTED FROM A SICK TO A HEALTHY PERSON, however, TRANPLACENTAL TRANSMISSION of Borrelia during pregnancy FROM THE MOTHER TO THE FETUS IS POSSIBLE, which may explain the rather high percentage of patients of preschool and primary school age.
Human susceptibility to Borrelia is very high, and possibly absolute. Primary infections are characterized by spring-summer seasonality, determined by the period of tick activity. Infection occurs during a visit to the forest, in a number of cities - in forest parks within the city limits; summer residents, outdoor barbecue lovers, mushroom pickers, and tourists are at high risk of infection.
In terms of incidence, this infection occupies one of the first places in our country among all natural focal zoonoses. According to indirect estimates, more than 10 thousand people fall ill with borreliosis in Russia every year. As with other spirochetoses, immunity in Lyme disease is non-sterile. Those who have recovered from the disease may be re-infected after 5-7 years.
What to do after a bite?
Initial consultation regarding a tick bite can be obtained by calling an ambulance. If you removed the blood-sucking villain yourself, then put it in a clean box and promptly take it for analysis - this could be a sanitary and epidemiological station (SES) or, for example, hygiene and epidemiology centers.
After a tick bite in areas where encephalitis is endemic, FE immunoglobulin is administered. The necessary course of treatment is prescribed by the doctor, and this must be done promptly.
Lyme disease does not manifest itself immediately, and if left untreated, it can develop into a chronic, serious disease, often leading to disability. Therefore, the first thing that a person bitten by a tick is recommended to do is observe himself.
Lyme disease has a noticeable sign that appears on the skin in approximately 75% of patients with borreliosis: after 3-32 days, annular erythema (a round-shaped spot with a raised edge, inside of which there is a zone of unchanged epidermis) appears at the site of the bite. Then it gradually expands and can reach a diameter of 15–20 cm, and sometimes 50–70 cm. The presence of the disease can be confirmed by taking a blood test two weeks after the bite. You should also be alert to signs: fatigue, lethargy, headache, fever, but these may appear weeks later when you have almost forgotten about the bite.
Antibiotic treatment should be started as early as possible, when there are no signs of damage to the nervous system, heart and joints. In this case, the chances of a full recovery are significantly increased.
Manifestations
Over 30 years of careful study of the disease, a fairly good correlation was established between the strain of the pathogen and the pattern of development of chronic infection:
- B.burgdorferi sensu stricto (mainly a North American isolate, but also found in Europe) mainly manifests itself in the form of arthritis;
- B. afzelii (the main European isolate, in Western Siberia it accounts for about 20%) - most often causes skin manifestations, primarily chronic atrophic dermatitis;
- B.garinii (the main Siberian variant of Borrelia) - most often manifests itself in the form of neuroborreliosis (pain along the nerve fibers, perverted sensitivity, paralysis, damage to the central nervous system).
Almost always, chronic borreliosis is accompanied by various autoimmune manifestations. Establishing a diagnosis based on the described symptoms is complicated not only by their diversity and abundance, but also by its strong dependence on the individual characteristics of the patient, as well as cases of combined forms of infections.
Even one tick can infect two strains of Borrelia at once; with multiple bites this happens quite often. “The Great Hoaxer” among clinical microbiologists .
Is the truth somewhere in the middle?
So are there those who are right and those who are wrong in these “Lime Wars”? In reality, it seems, the situation is much more complicated.
For example, experimental evidence has recently been obtained that patients with post-Lyme syndrome do not suffer from some kind of psychological disorders, but from very specific brain lesions. In their blood, as well as in eight parts of the brain, an increased content of a protein was found, which serves as a marker of the inflammatory process. Moreover, for six months after the course of antibiotic therapy, these people felt severe weakness and inability to concentrate; suffered from memory and cognitive impairment (Coughlin, Yang, Rebman et al
., 2018). Because of the inflammation and damage associated with Borrelia infection, these neurological symptoms can persist for weeks or months even after a long initial course of antibiotics.
But do live borrelia remain in the body? In the vast majority of cases, even very long courses of additional antibiotic therapy did not alleviate the suffering of patients with the chronic form of the disease. So the answer to this question will most often be “no”. Moreover, such courses of antibiotics themselves can have a devastating effect on the health of patients due to the destruction of normal intestinal microflora, allergic reactions and other negative side effects.
However, in rare cases of chronic borreliosis, additional antibiotic therapy was still effective. It is likely that in some patients, after a standard or delayed or incomplete course of treatment, live Borrelia may actually remain in the body, i.e. we are talking about a chronic infection. Let us remember that laboratory diagnosis of borreliosis is unreliable today. In addition, in the case of chronic borreliosis, infectious agents may be located mainly inside neurons, i.e., behind the blood-brain barrier. And diagnostic systems have low sensitivity and are unsuitable for use in patients who have a low number of bacteria in the blood.
So it all depends on the situation, and in some cases we can talk about a real chronic infectious disease, and in others we can talk about the development of post-Lyme syndrome after an illness.
Diagnostics
Unfortunately, in Novosibirsk clinics, diagnosing ticks for the presence of Borrelia is the exception rather than the rule. This is primarily due to the lack of certified diagnostic kits for Borrelia antigens. Using PCR tests to determine borreliosis in a patient immediately after a bite is difficult, as it involves taking pieces of skin. Immediately after a bite, there are practically no borrelia in the blood, however, analysis of the presence of borrelia in the blood using PCR reveals the pathogen in 25-30% of cases.
However, at present, the only reliable way to diagnose tick-borne borreliosis is enzyme immunoassay , based on the detection of specific immunoglobulins to the main antigens of Borrelia burgdorferi.
Class “M” immunoglobulins can appear in the patient’s blood within a week (usually 14 days) after infection, IgG - on average after 20-30 days. As the infection progresses, the spectrum of the main antibodies changes, but their overall titer remains high, which makes it possible to establish the presence of the disease with high reliability months and even years after the bite.
In case of a tick bite, we provide all necessary assistance:
- Removing a tick.
- Examination of ticks for carriage of infections.
- Administration of immunoglobulin against tick-borne encephalitis.*
- Selection of therapy for the prevention of borreliosis.
* In clinics at the following addresses: B. Sampsonievsky Ave., 45, st. Lenskaya, 17, st. Shavrova, 26, Staro-Petergofsky Ave., 39.
Anti-tick immunoglobulin is administered to unvaccinated patients no later than the 4th day (96 hours) from the moment of the tick bite.
It is possible to administer anti-tick immunoglobulin in emergency situations 48 hours before leaving for an unfavorable area where contact with the tick-borne encephalitis virus is likely. The protection in this case lasts up to 4 weeks.
Treatment
Like most spirochetes, Borrelia burgdorferi is sensitive to antibiotics, so treatment in the early stages is usually extremely effective and consists of a short course of antibiotic therapy. At the same time, “old” forms are quite difficult to treat, especially when organic changes begin to develop as a result of borreliosis.
It should be remembered that the earlier treatment is started, the simpler it is, the lower the required doses of antibiotics, the shorter the recommended course of therapy, the less the risk of developing the main symptoms of tick-borne borreliosis and its complications. Knowing about the presence of borreliosis infection is in the interests of the patient, therefore, after a tick bite, it is simply necessary to consult with a specialist and, at the appropriate time, analyze the presence of antibodies and DNA of the infectious agent in the blood.
It is important to know!
A consultation with a specialist on tick-borne infections at Medinsky will help you respond competently to an encounter with a tick, minimize the risk of contracting borreliosis, or start treatment on time. take all blood tests for the diagnosis of tick-borne borreliosis (antibodies to Borrelia classes M and G, PCR diagnostics of Borrelia DNA) at the Status MC upon the referral of your doctor or according to a plan prescribed by a specialist at the Status MC.
Swords crossed
The problem of chronic borreliosis is especially acute in the United States, where the Infectious Diseases Society of America
, IDSA) until recently generally denied its existence.
Only in 2019 was it officially recognized that after treatment for Lyme disease, a number of nonspecific symptoms may persist for a long time in some patients. However, without clinical evidence of the presence of live Borrelia in a patient, IDSA does not recommend attributing such symptoms directly to the previous disease and conducting additional courses of antibiotic therapy. Accordingly, insurance companies refuse to pay for treatment for people suffering from a “non-existent disease.” HOW TO REMOVE WITH YOUR HAND
The problem of chronic borreliosis in the USA is complicated by the activity of “healers”, “specialists in chronic Lyme disease”, artificially whipping up fears and making money from patients. Having intimidated patients experiencing ailments of various natures that are not confirmed by a clear diagnosis, and having convinced them that they have chronic borreliosis, healers prescribe them long-term, expensive treatment according to their own regimens. But many months of antibiotic therapy can be destructive for a weakened body. In addition, by wasting time communicating with charlatans, patients are not treating a real disease, such as Alzheimer's disease. Ultimately, the patient returns to the specialist after spending countless hours on pointless procedures and losing thousands of dollars. In Russia, the situation with chronic borreliosis and complications after this disease is not too different: the same unreliable diagnosis, scientifically unfounded recommendations for the prevention and treatment of borreliosis. Obviously, we also have many patients suffering from chronic infections that were not diagnosed and treated in time. There are also plenty of charlatans offering to cure any disease for a fee. Not to mention representatives of official medicine who are trying to treat diseases such as tick-borne encephalitis with the help of homeopathic remedies, drugs with unproven activity that have not undergone appropriate testing, such as iodantipyrine. Or even dummy drugs that do not contain any active substance at all, such as Anaferon produced by NPF Materia Medica Holding LLC, which is headed by O. I. Epstein, the hero of recent investigations of the Commission for Combating Pseudoscience of the Russian Academy of Sciences
Thousands of people in the United States, who have suffered for years from serious illnesses that they associate with the consequences of tick-borne infections, do not agree with this position. Chronic Lyme disease was first noted in the United States 45 years ago: according to some estimates, the number of such patients today reaches 400 thousand people. These people, together with some doctors, organized the International Society for the Control of Lyme Disease and Associated Diseases, which proposes the use of aggressive antibiotic therapy when it is suspected that the observed painful symptoms are caused by a borreliosis infection.
Defenders of the official point of view believe that chronic Lyme disease itself was invented by unscrupulous doctors exploiting the desperate condition of patients with an uncertain diagnosis. In their opinion, those patients in whom modern diagnostic methods do not detect Borrelia do not need additional treatment, but the help of a psychiatrist. As a result, people who consider themselves chronically ill are forced to turn to doctors who disagree with the position of the medical authorities and receive treatment at their own expense.
However, most doctors in the USA and Canada follow the instructions of official medicine, which has led to real “Lyme wars”. According to some experts, research into the pathology of Lyme disease has become so politicized that it has made it difficult for American medical journals to publish work on chronic borreliosis and to fund research aimed at studying it.
And remember:
- Viral encephalitis and tick-borne borreliosis are two completely different infections that require separate diagnostics and completely different treatment methods.
- The so-called “ tick vaccination ”, which many wisely give themselves before the tick season, is a vaccination ONLY AGAINST VIRAL ENCEPHALITIS AND DOES NOT PROTECT FROM BORRELIOSIS IN ANY WAY. There are simply no vaccinations against tick-borne borreliosis.
- Immunoglobulin injections, which are given after a tick bite, protect ONLY AGAINST VIRAL ENCEPHALITIS and are absolutely useless in the case of BORRELIOSIS.
- The drugs that are prescribed for the treatment of viral encephalitis (viferon, iodantipirin, etc.) are almost USELESS AGAINST TICK-BORNE BORRELIOSIS.
- The same tick can infect you with ENCEPHALITIS AND BORRELIOSIS AT THE SAME TIME (or even encephalitis and two different strains of borreliosis). Therefore, if an encephalitis virus is found in a tick, this does not mean that borreliosis is absent there.
- According to long-term studies, the infection of ticks with encephalitis in the NSO rarely exceeds 5%, and the infection of ticks with BORRELIOSIS IS ABOUT 30% (in some areas it reaches 60%!).
Consultations and registration by phone: (383) 347-75-80, 8-951-365-83-66 630102, Novosibirsk, Meditsinsky, st. Zyryanovskaya 61 e-mail