Very often, a young mother may be puzzled by an innocent question from a neonatologist observing a child in the maternity hospital about vaccinations. The whole difficulty lies in the fact that you need to make the right decision, on which the future health of the baby depends. Moreover, make this decision thoughtfully, based on WHO recommendations, the advice of the doctor supervising the child, and not the “girl next door”, girlfriend, or TV program.
Unfortunately, it is now fashionable to refuse vaccination, citing the fact that it is useless, that vaccination does not protect 100% from infection, that it “undermines” the child’s immunity, contributes to the occurrence of chronic diseases, and much, much more. Let’s try to figure it out together, decide and understand what it is, this “mysterious” vaccination, what it is needed for, what it protects against.
When a child is born, he or she is usually immune to certain diseases. This is thanks to disease-fighting antibodies that are passed through the placenta from mother to unborn baby. Subsequently, the breastfeeding infant continually receives additional antibodies through breast milk. But such immunity is only temporary.
Vaccination (inoculation, immunization) is the creation of artificial immunity to certain diseases. For this purpose, relatively harmless antigens (protein molecules) are used, which are part of microorganisms that cause diseases. Microorganisms can be viruses or bacteria.
Vaccination is one of the best ways to protect children against infections that caused serious illness before vaccines were available. Unfounded criticism of vaccination in the press was caused by the desire of journalists to inflate sensations from individual cases of post-vaccination complications. Yes, there are side effects that are common to all medications, including vaccines. But the risk of getting a complication from vaccination is much lower than the risk from the consequences of an infectious disease in children who have not been vaccinated.
Vaccines stimulate the immune system to respond as it would during a real infection. The immune system fights the infection and remembers the microorganism that caused it. If the microbe enters the body again, the developed immunity effectively fights it. Currently, there are types of vaccines: live and inactivated.
Inactivated vaccines, in turn, are divided into:
- Corpuscular
They are bacteria or viruses that have been inactivated by chemical or physical action. Examples: pertussis (as a component of DPT and Tetracok), anti-rabies, leptospirosis, whole-virion influenza, vaccines against encephalitis, against hepatitis A (Avaxim), inactivated polio vaccine (Imovax Polio, or as a component of the Tetracok vaccine).
- Chemical
They are created from antigenic components extracted from a microbial cell. Such vaccines include: polysaccharide vaccines (Meningo A+S, Act-HIB, Pneumo 23, Typhim Vi), acellular pertussis vaccines.
- Recombinant
To produce these vaccines, recombinant technology is used, integrating the genetic material of the microorganism into the yeast cells that produce the antigen. After cultivating the yeast, the desired antigen is isolated from it, purified, and a vaccine is prepared. An example of such vaccines is the hepatitis B vaccine (Euvax B).
- Alive
Live vaccines are made from weakened strains of microorganisms with persistently avirulent (harmless) properties. The vaccine strain, after administration, multiplies in the body of the vaccinated person and causes a vaccine infection process and leads to the formation of, as a rule, stable immunity. Examples of live vaccines include vaccines for the prevention of rubella (Rudivax), measles (Ruvax), polio (Polio Sabin Vero), tuberculosis, mumps (Imovax Oreion).
- Anatoxins
These drugs are bacterial toxins inactivated by exposure to formaldehyde at elevated temperatures, followed by purification and concentration.
The doctor caring for your child will explain and tell you that children are vaccinated as part of the national vaccination calendar, which looks like this:
| Age | Name of vaccination |
| 12 hours | First vaccination - hepatitis B |
| 3-7 day | Vaccination - tuberculosis |
| 1 month | Second vaccination - hepatitis B |
| 3 months | First vaccination - diphtheria, whooping cough, tetanus, polio, hemophilus influenzae* |
| 4.5 months | Second vaccination - diphtheria, whooping cough, tetanus, polio, hemophilus influenzae |
| 6 months | The third vaccination is diphtheria, whooping cough, tetanus, polio, hemophilus influenzae. Third vaccination - hepatitis B |
| 12 months | Vaccination - measles, mumps, rubella |
| 18 months | First revaccination - diphtheria, whooping cough, tetanus, polio, hemophilus influenzae |
| 20 months | Second revaccination - polio |
| 6 years | Second vaccination - measles, mumps, rubella |
| 6-7 years old (1st grade) | First revaccination - tuberculosis |
| 7-8 years old (2nd grade) | Second revaccination against diphtheria, tetanus |
| 13 years | Vaccination against hepatitis B (previously not vaccinated). Vaccination against rubella (girls) |
| 14-15 years old (9th grade) | The third revaccination is diphtheria and tetanus, polio. The second revaccination is tuberculosis. |
| 15-16 years old (10th grade) | Revaccination against measles and mumps in those vaccinated once |
If, for certain reasons, a child begins to be vaccinated outside of this schedule, then his supervising pediatrician must create an INDIVIDUAL vaccination plan.
Separately, I would like to note the fact that parents should know that none of the currently used vaccines can guarantee the absence of adverse reactions. Therefore, measures to prevent post-vaccination complications are extremely important.
- The main preventive measures include: strict implementation of vaccination techniques;
- compliance with contraindications;
- accurate execution of instructions for transportation and storage of vaccines;
- maintaining intervals between vaccinations.
- Factors predisposing to post-vaccination complications include: The presence of damage to the nervous system in the child, especially such as increased intracranial pressure, hydrocephalic and convulsive syndromes.
- Any forms of allergic manifestations.
- Frequency, duration, nature of acute diseases, features of the course of chronic diseases.
- A history of abnormal reactions to previous vaccinations.
- When vaccination, the following provisions must be observed: The minimum interval between vaccination and a previous acute or exacerbation of a chronic disease must be at least 1 month. However, for mild acute diseases (for example, a runny nose), the interval can be reduced to 1 week. Influenza vaccinations with inactivated vaccines can be done immediately after the temperature has returned to normal.
- There should be no patients with acute respiratory diseases in the child’s immediate environment.
- In cases where the doctor for any reason is afraid to vaccinate a child on an outpatient basis, the vaccination can be carried out in a hospital (for example, in cases of severe allergic reactions in the past).
Recommendations
- Before you start getting vaccinated:
- visit children's doctors, including a neurologist;
- Additional consultation with a specialist is necessary if:
the child has any disease, birth injury, diathesis;
o the child is taking any medications;
- o there was a severe reaction to the previous vaccine administration;
- are allergic to anything;
- the child has received gammaglobulin or blood transfusion in the past three months;
- the child or any family member suffers from immunodeficiency, cancer, AIDS or other immune diseases;
- the child or family member is taking steroids, radiation or chemotherapy
- carefully study the general contraindications to vaccination and contraindications to a specific vaccination - make sure that they do not apply to your child.
- stop introducing new types of food at least a week in advance (important for children with allergies);
- Talk to your pediatrician about ways to prevent and mitigate allergic reactions to the vaccine;
- take blood and urine tests, get the results and make sure that they allow you to get vaccinated;
- Avoid taking antibiotics and sulfonamides 1-2 days before vaccination with live vaccines;
- Preparing for vaccinations
- the less time passes between receiving the test result and the actual vaccination, the better;
start giving your child a prophylactic drug if prescribed by a doctor;
- Ask your doctor how long after vaccination you can expect any adverse reactions (and what they are).
- Immediately before vaccination
- assess the child’s condition;
measure the temperature;
- if in doubt, contact your doctor;
- Before vaccination, the child must be examined by a doctor;
- you have the right to read the instructions for the vaccine and check the expiration date of the drug.
- After vaccination
- spend 20-30 minutes after vaccination in the clinic premises - this will allow you to receive quick, qualified help in case of severe allergic reactions;
as prescribed by the doctor, give the child a prophylactic drug;
- if the temperature rises, then give the child more to drink and wipe with warm water;
- if a child experiences local reactions: apply a cool terry cloth washcloth to the sore spot. It is unacceptable to apply compresses and ointments to the injection site yourself! If there is no improvement after 24 hours, call your doctor;
- carefully monitor the slightest changes in the child’s physical and mental condition, especially if you do not use prevention;
- tell your doctor about anything that seems unusual, this will be useful when preparing for the next vaccination;
- at the slightest sign of suffocation, call an ambulance. Be sure to inform the arriving doctors that you were vaccinated today (against what disease and with what vaccine).
- Further:
- continue to give the prophylactic drug for as many days as prescribed by your doctor;
- monitor the child’s condition for as many days as the reaction may last;
- Antibiotics and sulfonamides should be avoided for 7 weeks after vaccination with live vaccines;
- if all the deadlines have passed, but some residual effects remain (the child is nervous, there is inflammation at the site of vaccine administration, etc.), contact your doctor;
- Do not introduce new types of food to your child for a while.
As for contraindications for vaccination, as practice shows, this is one of the most concerning issues for parents. Therefore, I would like to briefly explain what applies to them.
Contraindications to vaccinations are divided into the following categories: permanent (absolute) and temporary (relative); and also true and false.
Permanent (absolute) contraindications:
Permanent contraindications are quite rare and their frequency does not exceed 1% of the total number of children.
- Severe reaction or complication to a previous dose.
- A severe reaction is the presence of a temperature above 40 degrees, at the site of vaccine administration - swelling, hyperemia > 8 cm in diameter. Complications include: anaphylactic shock reaction, collapse, encephalitis and encephalopathy, non-febrile convulsions.
A vaccine that causes a severe reaction is contraindicated. In case of severe systemic allergic reactions to the measles vaccine, the mumps vaccine is also not administered. Live polio vaccine is contraindicated for subsequent administration to children who have had vaccine-associated polio. However, they can be given inactivated polio vaccine.
- Immunodeficiency state (primary). Vaccines are contraindicated: BCG, OPV, measles, mumps, rubella.
- Malignant neoplasms. The following vaccines are contraindicated: BCG, OPV, DPT, measles, mumps, rubella.
- Pregnancy. All live vaccines are contraindicated. The ban on the administration of live vaccines is associated not so much with the danger of their teratogenic effect (assumed only theoretically), but with the possibility of linking, for example, birth defects in a newborn with vaccination. Therefore, contraindications in this part should be considered, first of all, as a means of protecting the medical worker performing vaccination from possible accusations.
How to choose a drug
Imported ones have many components in one injection and are easy to use. Less painful due to thin needles. Domestic ones are more accessible and are shown to everyone.
Vaccination against tetanus and diphtheria is included in the compulsory medical insurance package; you can get vaccinated for free at the clinic.
Can I bring my vaccine to the clinic? From a legal point of view, yes. But not all doctors are ready to meet and take risks, justifying it by the lack of information about the correct storage and transportation.
Relative (temporary) contraindications:
- Acute illness. The most common situations are where children who should receive a routine vaccination suffer from an acute illness at that moment. General recommendations on this matter say that vaccines should be administered 2 weeks after recovery. In some cases, the interval can be shortened to 1 week or extended in case of severe illness to 4-6 weeks. In some cases, a child with a mild illness (for example, a mild runny nose without fever) is not a contraindication to the use of vaccines, especially if the child frequently suffers from upper respiratory infections or allergic rhinitis. Fever in itself is not a contraindication to immunization.
However, if fever or other symptoms indicate a moderate or severe illness, the child should not be vaccinated until complete recovery.
In any case, a doctor should give a conclusion about the severity of the disease and the possibility of vaccination.
If there are epidemiological indications, children are vaccinated at the time of acute illness. Studies have shown that with this approach the number of reactions and complications does not increase. However, the administration of a vaccine to such children is fraught with the risk that the resulting complication of the underlying disease or its unfavorable outcome may be interpreted as a result of the vaccination.
- Exacerbation of a chronic disease. After an exacerbation of a chronic disease, it is necessary to wait for complete or partial remission (after 2-4 weeks from a specialist).
- Administration of immunoglobulins, plasma and blood transfusions. Inactivated vaccines do not interact with circulating antibodies and can therefore be administered simultaneously. Antibodies and vaccines for hepatitis B, rabies, and tetanus are usually used at the same time.
- Live vaccines contain whole, live viruses that must replicate in the body to produce immunity. Antibodies can interfere with this process. Therefore, when using immunoglobulins (or blood products) and vaccines together, the following rules must be observed: after administering the vaccine, you must wait at least 2 weeks before administering the immunoglobulin;
After administration of immunoglobulin, a break of at least 6 weeks (preferably 3 months) is required before administering the vaccine. This is the time it takes for antibodies to be destroyed. The exceptions are vaccines against polio and yellow fever. In the case of these vaccines, no intervals between administration of immunoglobulins or blood products are required.
Drugs
Adasel is an imported alternative to ADS and ADS-M. Contains a pertussis component for children and adults. Placed every 10 years.
Pentaxim is a French vaccine that prevents 5 diseases, consists of three doses, is administered according to the general scheme, with an interval of 1.5 months. It has variability; on the recommendation of a doctor, it can be placed according to a different scheme. Revaccinated once at the age of eighteen.
False contraindications to preventive vaccinations:
In addition to infections for which delaying vaccination until recovery is justified, there is a wide range of conditions (such as perinatal encephalopathy, allergies, anemia) that are the main unjustified reasons for delays in vaccination.
- An acute illness of mild severity, without fever.
- Prematurity. An exception is BCG vaccination if the child was born weighing less than 2000 grams. All other vaccinations are carried out according to the generally accepted schedule.
- Malnutrition, anemia
- Dysbacteriosis as a diagnosis is justified in a patient whose stool disorder is associated with the massive use of broad-spectrum antibiotics; Obviously, in these cases, vaccination is postponed until recovery. In a child with normal stool, the diagnosis of “dysbacteriosis” does not have any basis, so the fact of quantitative or qualitative deviations of the microbial flora of feces from the “norm” is not a reason to cancel or delay vaccination).
- Perinatal encephalopathy is a collective term denoting damage to the central nervous system of traumatic or hypoxic origin, the acute period of which ends during the first month of life. In practice, however, this term is often used as a diagnosis to designate non-progressive residual disorders (changes in muscle tone, delayed development of mental and motor functions, disturbances in the periodicity of sleep and wakefulness), which in some regions is diagnosed in 80-90% of children in the first months life. There is no need to postpone vaccinations in these cases. Naturally, if there is no clarity about the nature of the change in the central nervous system, then it is better to postpone vaccination until an additional consultation with a neurologist to make a final diagnosis and decide on vaccination.
- Stable neurological conditions (Down syndrome and other chromosomal diseases, cerebral palsy, obstetric paralysis and paresis, consequences of injuries and acute diseases) do not carry the risk of adverse effects of vaccination
- Allergies, asthma, eczema, and other atopic manifestations are indications for vaccination rather than contraindications, since in these children infections are especially severe (for example, whooping cough in a patient with asthma). Before vaccination, it is advisable to consult an allergist in order to choose the optimal time of vaccination and select the necessary drug protection.
- Congenital malformations, including heart defects, in the compensation stage are not a contraindication to vaccination.
- Chronic diseases of the heart, lungs, kidneys, and liver are not a contraindication for vaccination if the disease is in remission.
- Topical treatment with steroids in the form of ointments, eye drops, sprays or inhalations is not accompanied by immunosuppression and does not interfere with vaccination.
- Maintenance therapy for chronic diseases (antibiotics, endocrine, cardiac, antiallergic drugs) provided to children with the corresponding disease is not in itself a contraindication to vaccination.
- An enlarged thymic shadow on a radiograph is either an anatomical variant or the result of stress hyperplasia. such children tolerate vaccinations well, give a normal immune response, and the frequency of post-vaccination reactions in them is no greater than in children without a visible thymus shadow on a radiograph.
- Conditions that existed before vaccination, but are no longer present (in history) are also not a contraindication for vaccination: Moderate local reactions to the previous administration of the vaccine
- Prematurity
- Perinatal encephalopathy
- Hemolytic disease (jaundice) of newborns
- Sepsis, hyaline membrane disease
- Unfavorable family history (allergy in the family, epilepsy and complications after vaccination in relatives, sudden death in the family). An exception is an indication of the presence in the family of a patient with symptoms of immunodeficiency (in this case, instead of a live polio vaccine, an inactivated one is used and the newborn is additionally examined before BCG is administered to him).
I hope this article will help parents decide whether to vaccinate their child or not, because his health is in your hands.
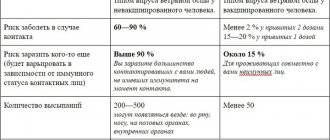
Adverse reaction of the body to vaccination and statistics of complications
General (within normal limits): fever, loose stools, nausea, lump and lump from an injection, cough that goes away within a day. The appearance and worsening of reactions after 24 hours are local manifestations (additional, coinciding with medical manipulation) and can lead to complications, in which case it is necessary to consult a doctor.
Complications directly from DTP - allergic manifestations, convulsions without fever, shock, neurological symptoms - 1-3 cases per 100,000 vaccinated people. The remaining complications are local, based on concomitant diseases.
Is it possible to refuse vaccinations every 10 years? Yes, but it has consequences. The lack of specific immunity to infections forces the body to fight an unknown enemy blindly, increasing risks, causing complications and burdens.
Reasons for refusal: contraindications, intolerance to a previously used vaccine (you can choose a similar one).