The skin test or Mantoux test is an important diagnostic procedure necessary for the early detection of symptoms of tuberculosis. It is characterized by intradermal injection of inactive Koch bacilli with the formation of a small bubble on the surface of the hand. It is given to children in a specific place and after a specific period of time. The injection is done in several stages: first the vaccine is administered, and after 2-3 days the result is read.
Why is Mantoux vaccinated?
As a rule, the tuberculin test is carried out everywhere in all age groups. The main indications for such manipulation are:
- Detection of signs of tuberculosis at the initial stage of development in children and adolescents.
- Tracking the formation of immune status after BCG.
- Timely detection of various changes in the Mantoux reaction, which indicates the presence of tuberculosis disease.
- Selection of a specific group of people who require the introduction of an anti-tuberculosis vaccine.
SIDE EFFECTS, COMPLICATIONS
An excessive response of the patient’s body to the administered drug is the cause of the main side effects. These include:
- Allergy. This reaction is possible in patients of any age, since tuberculin is an allergen.
- Temperature. With high sensitivity to the drug, a slight increase in temperature may be observed.
- Hyperergic reaction. Formation of papules larger than 17 mm in diameter. This answer indicates the presence of tuberculosis infection in the body.
- Cough. Traditionally, this side effect is not associated with the administration of the sample.
- The papule itches. It is necessary to avoid scratching the papule; the tuberculin injection site itself may itch.
Contraindications Mantoux
It is important to meet all requirements and consult with your doctor before performing a skin test. Children must be examined by a pediatrician, since the reaction has some contraindications. These include:
- Dermatological diseases of various nature.
- Chronic inflammatory pathologies in the body in the acute stage.
- Infectious conditions of atomic or bacterial origin
- Epileptic seizures and other mental disorders.
- Any allergic reactions during the period of unstable remission (asthma, rheumatoid arthritis, rhinitis).
If the patient is sick, it is worth waiting for recovery and only 2 months after the clinical signs of infection have disappeared, a test is allowed.
Tuberculin diagnostics (Mantoux test)
Tuberculin diagnostics (Mantoux test)
The Mantoux tuberculin test, colloquially “button”, is a specific diagnostic test (not to be confused with vaccination!), used in mass screening of the population for tuberculosis.
To carry out tuberculin tests, tuberculin is used, which is a complex compound in its composition. It does not contain live or killed tuberculosis mycobacteria, but only their metabolic products, microbial cell elements and part of the medium on which tuberculosis mycobacteria grew.
To the introduction of tuberculin, an allergic response (positive tuberculin test) occurs in those vaccinated with the BCG vaccine against tuberculosis (post-vaccination allergy) and in those infected with Mycobacterium tuberculosis (infectious allergy). In both cases, there are tuberculosis bacilli in the body of the subject. Only in the first case they were introduced with the BCG vaccine and support immunity to tuberculosis, and in the other they entered the body from the environment and are virulent, i.e. under certain conditions can cause disease.
The Mantoux test is not a vaccination, it is a method for detecting the incidence of tuberculosis. It is carried out annually, and for some categories of children (chronic lung diseases, kidney diseases, diabetes mellitus, hormone treatment, HIV infection, etc.) 2 times a year. The Mantoux test is absolutely harmless for both healthy and sick children.
Contraindications to the Mantoux test:
- Skin, acute and chronic infectious and somatic diseases in the period of exacerbation;
- Allergic conditions, rheumatism in the active phase, bronchial asthma in the acute stage;
- In children's groups under quarantine regime;
- 1 month after vaccinations.
The Mantoux test is performed 1 month after the disappearance of clinical symptoms or immediately after quarantine is lifted.
Accounting of results after 72 hours:
- negative test - with complete absence of changes on the skin, or a “prick” reaction;
- doubtful - hyperemia (spot) of any size or papule (tubercle) 2 - 4 mm;
- positive – papule (tubercle) 5 mm or more;
- hyperergic – papule 15 mm or more and/or blistering rash, inflammation of the lymph nodes for any size of papule.
Normally, within 2-4 years after BCG vaccination, the Mantoux test is positive, this is the so-called post-vaccination allergy; by the age of 4, the size of the papule decreases and becomes negative. If a child becomes infected with tuberculosis within a year, the size of the papule increases sharply and it becomes positive. Such children need urgent further examination and consultation at an anti-tuberculosis dispensary. The referral is given by a local pediatrician or a doctor at a children's institution.
Skin test schedule
After birth, all children, in the absence of contraindications, receive the BCG vaccine. After this, a mantu test is performed 12 months later. Subsequently, the diagnostic procedure is carried out up to 15 or 18 years inclusive, once a year.
If the child has not been vaccinated with BCG, the test is done at 2 months of the baby’s life. It is very important that the tuberculin injection is given before other routine vaccines and serums. If the latter were carried out, the Mantoux reaction is performed after a month.
As a rule, the test schedule is once a year. However, it is more often recommended to test children who are at risk of developing tuberculosis. These include:
- Previously not vaccinated for various reasons.
- Patients with diabetes.
- HIV-affected.
- Persons undergoing hormonal or anticancer therapy.
- Children after irradiation.
- Patients with severe chronic pathologies of the respiratory and digestive systems.
- Babies who have not yet had their BCG vaccine evaluated.
Such children are tested 2 times a year.
WHAT IS THE MANTOU REACTION
The Mantoux test is designed to provoke an immune response. It has nothing to do with vaccination, so it is incorrect to say that Mantoux is a vaccination. In order for the human body to respond to a microbiological invasion, the immune system must be familiar with these microorganisms. The immune system can only respond to threats with which it is already familiar. The immune system will not be able to recognize new infections until a person is vaccinated or has had a certain disease.
If the immune system is familiar with tuberculin bacteria, when they are introduced, immune cells will attack tuberculin. In this case, a local inflammatory reaction will be observed.
How to read the reaction to manta
The skin test is read 2 days or a maximum of 72 hours from the date of the Mantoux test. The results may have several options:
- Negative - characterized by the absence of any traces of the injection. There is no lump, no hyperemia, just a mark from the injection. The size of the papule does not exceed 2 mm.
- Doubtful - at the test site there is limited redness of varying diameter, without a bump. Size 2-4 mm.
- Positive - determined by the appearance of a lump of more than 5 mm.
Suspicious reaction results that indicate the possibility of developing symptoms of tuberculosis in the body are considered:
- Detection of a papule larger than 5 mm after previous negative ones.
- The appearance of a large tubercle, over 12 mm.
- The test result differs from the previous year by 6 mm or more.
- A huge papule up to 17 mm or more, the presence of necrotic processes, an increase in the size of the lymph nodes and their suspicious compaction.
If such symptoms occur during a skin test, a final diagnosis is not made. The disease must be confirmed by a phthisiatrician; for this, patients are referred for consultation and all necessary medical examinations.
How to evaluate the results of the Mantoux reaction?
Starting from the age of one year, the child is given a tuberculin test annually. The doctor measures the transverse size of the “button” three days after the administration of tuberculin and sums up the results. The “verdict” can be: the reaction is questionable, the reaction is negative, or the reaction is positive. In turn, a positive test can range from “weakly positive” to “strongly expressed”. Based on the results of the Mantoux reaction, doctors identify children who are infected (not sick!) and not infected with Mycobacterium tuberculosis.
Many of you have heard the word “turn” from doctors, what is it?
The Mantoux test is a positive reaction that occurs for the first time (the diameter of the “button” is 5 millimeters or more). Virus occurs in children infected with Koch's bacillus.
If, based on the results of the Mantoux test, the doctor suspects infection with tuberculosis, the child is sent to an anti-tuberculosis dispensary for consultation with a phthisiatrician and additional research.
Complications after the mantoux test
The only and fairly common complication after injection is the development of signs of allergies. This condition is more common in children who suffer from or are at risk for diathesis, helminthic infestations, rheumatism, food allergies, thyroid diseases and any chronic inflammatory processes.
Symptoms of an allergic reaction after mantoux are: skin rash, itching and flushing. Rarely there is a cough, swelling of the neck and face. Malaise, headache and weakness may occur. These signs do not pose a threat to health and after a certain time disappear on their own without treatment.
REACTION TO TEST BY DAY
A reaction to Mantoux is observed in patients on the second day after the test. The body may react with the formation of a papule and/or redness. The maximum immune response can most often be noted on the third day. The reaction can be negative, false negative or positive, false positive:
- Negative. The absence of any reaction indicates that the immune system is not familiar with tuberculosis pathogens. The patient does not suffer from tuberculosis in any form. If a child has had less than 5 years since vaccination, a negative reaction is a bad signal. He reports that the immune system does not remember danger. If more than 5 years have passed, then the lack of reaction is a plus. This is a sign that the child is not sick. The same rule works for adults.
- False negative. This reaction can be observed in cases where a person’s immune system stops responding to injected tuberculin over the years.
- Positive. We can talk about such a reaction to the test if the papule is larger than 5 mm in diameter. It is necessary to analyze a positive result in children based on a combination of factors. It is necessary to evaluate the dynamics of the sample over the past years, the very nature of the papule, the size of the scar, and how long ago the vaccination was performed. If the reaction is positive in an adult, this is a signal of almost 100% probability of infection.
- False positive. This category includes questionable answers - redness of any size, papules with a diameter of less than 4 mm. A false positive reaction can occur in a number of cases. For example, when a person has recently undergone any vaccination or has had an infectious disease. Also, a questionable reaction occurs with a skin allergic reaction, etc. To make sure that there is no need to panic in case of a false positive result, it is necessary to check whether the patient has contacts with tuberculosis patients, the situation in the region, and whether the incidence threshold has been exceeded.
Evaluation of Mantoux test results
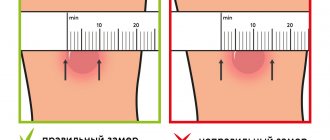
The test result is assessed by a doctor or trained nurse 72 hours after the test. A reaction to tuberculin is possible in the form of hyperemia (redness of the skin) and the formation of a papule (a dense round area rising above the skin). Assessment of the Mantoux test consists of taking into account the size of the papule and assessing the severity of hyperemia. The measurement is carried out in a direction transverse to the axis of the hand, the result is taken into account in millimeters. Only the size of the papule is measured, and not the size of the area of hyperemia (redness). The size of the redness is taken into account only when the papule has not occurred.
Reaction options for the Mantoux test:
- negative - there are no changes on the skin;
- doubtful - there is redness of any size without a papule, or a papule no more than 2-4 mm;
- positive mild - papule size 5-9 mm;
- positive of medium intensity - papule size 10-14 mm;
- positive pronounced - papule size 15-16 mm;
- excessive (hyperergic) - the size of the papule exceeds 17 mm or there are pronounced signs of inflammation (reaction of the lymph nodes, skin ulceration, etc.).
- A negative Mantoux reaction indicates that the body does not have antibodies that are “familiar” with the tuberculosis bacterium. This means that the child is not infected, or there is no immune reaction to BCG vaccination.
- A questionable sample is considered negative.
- A positive test can be either a consequence of BCG vaccination or a sign of infection.
To assess the likelihood of infection, you need to look at the turn of the tuberculin test - the transition of a negative Mantoux reaction to a positive one (not associated with previous vaccination) or an increase in the diameter of the papule compared to the result of the previous test by 6 millimeters or more.
Also signs of infection are:
- hyperergic reaction;
- persistent (more than 4 years) persistent reaction with a papule of 12 mm or more;
- gradual (over several years) increase in sensitivity to tuberculin with the formation of an infiltrate measuring 12 mm or more.
A positive Mantoux test result without taking into account other diagnostic criteria is not a basis for making a diagnosis or starting any treatment.
Only a doctor can evaluate the reaction; if necessary, the child will be referred for additional examination to a TB specialist.