Some medications, such as glucocorticoids and immunosuppressants, may suppress the development of vaccine immunity. In such cases, vaccination tactics should be discussed with your doctor.
For vaccines against the new coronavirus infection, the duration of vaccine immunity remains one of the main questions. It is very difficult to predict the duration of protection of a particular vaccine. This is usually determined in practice by recording the frequency of infections in people vaccinated during mass vaccination after different amounts of time, as well as measuring the titer of protective antibodies.
Titer? What other title?
As we have already found out, antibodies are proteins that circulate in the blood. In order to provide effective protection, these proteins must be in the blood at a certain concentration - this is called the titer. Express titer as numbers separated by colons, for example 1:50 or 1:100 (read as “one in fifty” or “one in one hundred”).
Since antibodies are complex proteins, it is extremely difficult to determine them by chemical methods. Therefore, immunological reactions are used to determine antibodies. There are a lot of specific methods, but in the most general form the essence of these reactions is very simple. We take a solution of the desired antigen (for example, the same spike protein of the coronavirus) and mix it with the serum in which we are looking for antibodies. If there are antibodies in the serum, they bind to the antigen and their compound precipitates or the solution becomes cloudy. In practice, carrying out such a reaction looks more complicated; special gel media and different detection methods are often used, but this does not change the essence.
The problem is that this approach only answers the question of whether there are antibodies in the serum or not, but does not tell us anything about the amount of antibodies themselves. How, then, can two different serums be compared with each other? The amount of sediment that fell is not an option, the error is too large. But there is another way - you can dilute the test serum until the reaction (precipitate) is still detectable. And the last, strongest dilution, at which we can still observe the reaction of the serum with the antigen solution, is called the titer of this serum. That is, a titer of 1:50 tells us that this serum can be diluted 50 times and it will still react with the antigen. Accordingly, the larger the second digit in the titer designation, the higher the concentration of antibodies in the serum.
The disadvantage of a titer is that it indicates the relative abundance of antibodies. If we have two sera with titers of 1:50 and 1:100, we can confidently say that the second serum contains 2 times more antibodies than the first. But we do not know what exactly the concentration of antibodies is in each of these sera. In practice, this often happens and is not necessary: it is enough for us to know with what titer of antibodies a person is still protected from infection, and with what titer he is no longer protected. This can be easily determined by measuring antibody titers in vaccinated people who still become infected.
Laboratory test results usually report antibody concentrations in international units (IU) or relative units (RU). The results obtained in IU can be compared with each other - the value will not depend on the laboratory, test system and analysis conditions (there are no such conditions for coronavirus yet). The results, expressed in OE, can be compared with each other only for tests of the same brand, while the laboratory itself and the time of analysis do not play a role, that is, it is possible to track the dynamics of changes in the level of antibodies in one person.
What is the importance of therapeutic serums and preventive vaccinations in the modern world?
The appearance of vaccines and serums is a consequence of concern for the own health of physicians working with patients infected with infectious diseases. For many years, medical representatives were busy searching for remedies that could give them protection against cholera, smallpox, anthrax and rabies.
Research got off the ground only at the end of the 19th century, when L. Pasteur and E. Jenner conducted the first studies aimed at testing the first medicines containing living microbes.
The scientific activity of scientists gave a positive result and was the start for the development of a powerful medical industry. Since then, specialists have created many drugs designed to prevent and treat dangerous infections. These included vaccines against various infections, as well as serums that are actively used in modern medicine.
The use of vaccines and serum has made a real breakthrough in the field of medicine. Thanks to the use of such compounds, it was possible to reduce morbidity by tens of times and reduce the percentage of child mortality and deaths among adults caused by infectious diseases.
Not all antibodies are created equal
To characterize antibodies, it is important to understand their class, type, and which antigen they bind to.
Antibodies come in different classes (A, M, G, E, etc.). The main class of protective antibodies is G and is usually referred to as IgG in laboratory studies and tests. The presence of these antibodies in the blood indicates the presence of immunity after vaccination or illness. IgM is also a protective antibody that begins to be produced first, earlier than IgG. IgM is usually less effective than IgG and disappears almost completely towards the end of the disease. The presence of these antibodies usually indicates an ongoing or very recent disease, or a chronic infection. That is, if we are interested in stable immunity, we look for IgG in tests.
If an antibody binds to some protein on the surface of a virus or bacteria, this does not always mean that the bacteria and virus then become completely harmless. For example, a virus may use a different region of the surface protein to enter the cell than the one to which the antibody binds. Antibodies that bind to pathogens but do not suppress their danger are called binders. If the binding of an antibody completely “neutralizes” the microbe, “neutralizes” its dangerous influence, such an antibody is called neutralizing. Binding antibodies are not completely useless - by attaching to a virus or bacteria, such antibodies make them more visible to cells of the immune system and speed up the immune response. But it is neutralizing antibodies, which can independently neutralize dangerous microbes, that provide the main protection, and it is their level that is important when assessing vaccine or natural immunity. That is, in the tests we need to look for neutralizing IgG.
And finally, antigen. As we discussed above, antibodies have very high specificity and bind only to certain proteins. When the immune system, faced with an infection, selects the desired antibody, it most often begins to synthesize several different types at once, targeting different proteins of the pathogen. After all, cells that synthesize antibodies receive different pieces of a semi-digested microbe for analysis - both surface and internal proteins - and for each of them they look for an antibody. For effective protection, it is those antibodies that bind to proteins on the surface of the virus or bacteria that are important. After all, antibodies are large molecules that cannot penetrate into viral particles or bacteria; only surface proteins are accessible to them. That is why protective immunity is primarily provided by antibodies to surface antigens. For example, in the case of coronavirus infection, at least 2 types of antibodies are produced - to the S-protein (which is on the surface of the viral particle) and to the N-protein (also known as the nucleocapsid protein, which is located inside the viral particle). Since antibodies cannot reach the N-protein, it is antibodies to the S-protein that will provide protection. That is, if you still want to determine the level of protective antibodies after vaccination against Covid, you need to look for a test for neutralizing IgG to the S-protein.
How is the vaccine different from serum?
Both the vaccine and the serum are effective drugs created specifically to build immunity in humans to certain infections. But in fairness, it’s worth mentioning right away that they have different effects and are used in different situations.
A vaccine is a composition containing weakened or killed pathogens . Being in this state, the bacteria are not capable of causing harm to the human body (that is, the development of the disease after ingestion of the vaccine composition is excluded).
But their presence contributes to the development of stable immunity to a specific infectious agent. To develop immunity, sometimes one injection is enough. In some cases, a cycle of vaccinations followed by revaccination is required (for example, DPT).
As for serum, this is a composition that contains ready-made antibodies against a specific disease. Typically, this drug is used precisely when a person is already sick.
In this case, the drug is used for medicinal purposes to help the body cope with the disease. That is, unlike a vaccine, serum is not a prophylactic agent, but a medicine.
Differences in indications for administration
The drugs differ in their composition and manufacturing. This also dictates the differences in indications for administration. The vaccine must include pathogenic organisms, which can be live, dead or weakened.
Therefore, such drugs are used primarily for the prevention of infectious diseases that have not yet occurred. That is, vaccines are recommended to be used before the outbreak of an epidemic or at its height. Injections are given to people who have not yet become infected with an infectious disease.
As for the serum, it is used when a person has already become ill, in order to provide third-party assistance to the immune system. Serums contain ready-made antibodies, which significantly speeds up the patient’s recovery process.
The name of the disease, its nature and the characteristics of its course are not the main criterion determining the doctor’s choice (serum or vaccine). The decisive role in choosing a drug option is played by the presence or absence of an infectious agent in the body.
Serum, used to treat ailments, is used in fewer cases than a vaccine. Accordingly, vaccination can protect a person from a greater number of infections.
Difference in duration of immunity
Since the composition and production features of the serum and the vaccine differ, the characteristics of the drug’s effect on the body also differ. The serum has an immediate effect, thereby promoting the patient’s recovery.
However, a quick result does not guarantee long-term resistance to bacteria that provoke the development of infection. Usually the effect caused by the use of the drug lasts for 1-2 months.
As for the vaccine, it produces the required result only after a couple of weeks. However, the effect of the injection lasts for a period of one to several years.
The vaccine is used for preventive purposes when the patient “has time to wait.” The serum is used when there is a need for urgent medical action.
Differences in efficiency
It is impossible to say unequivocally which is more effective.
And it would be completely wrong to compare these two types of compositions in terms of performance. Both a correctly applied vaccine and a well-chosen serum are equally effective . However, the result will vary.
If you need to get a quick effect, use serum.
But if there is a need to obtain long-term protection from an infectious disease, a vaccine is used, the effect of which does not occur immediately, but is in no way inferior in strength and reliability to the result obtained after using the serum.
Other differences
The main difference is also considered to be the raw materials used to make the composition. For example, extracts from pathogenic microflora, antigenic components, extracts from microbial cells, or products obtained using genetic engineering methods can be used to prepare a vaccine.
To produce serum, the blood of animals previously prepared for such manipulations is used.
In this case, biological material from horses, pigs, and rabbits, which already have immunity to certain infectious diseases, is used. To obtain such blood, representatives of the fauna are immunized, after which serum is produced from the resulting material.
Vaccine characteristics
Vaccines consist of weakened or killed viruses or their components that cannot cause harm to humans. When the suspension is administered, the body turns on its defense mechanisms and begins to produce antibodies, forming stable immunity to a particular virus within a month.
The vaccine causes an active response from the body, the effect of which lasts for a period of several years, and with some infections its own antibodies are formed, providing long-term and sometimes lifelong protection (for example, against rubella, chickenpox, mumps, measles).
The vaccine is administered to a healthy person. In case of mild colds or exacerbation of chronic diseases, the procedure is postponed so as not to further burden the body and not cause additional complications. In case of certain contraindications, vaccinations are canceled, the basis is a written refusal of the parents.
What you need to know about the Sinovac-CoronaVac COVID-19 vaccine
The WHO Strategic Advisory Group of Experts on Immunization (SAGE) has issued interim recommendations on the use of the Sinovac-CoronaVac COVID-19 vaccine. This article provides a brief overview of the interim recommendations; The full guidance document is available here.
The following is information you need to know.
This article provides a brief overview of the interim recommendations; The text of the interim recommendations and background document (in English) are available here.
Who should be vaccinated first?
While supplies of COVID-19 vaccines are limited, priority should be given to healthcare workers at high risk of infection and older adults.
To determine the priority for vaccinating different target groups, countries can use the guidance provided in the WHO vaccine priority roadmap and the WHO values document.
Until the results of additional studies are obtained, it is not recommended to vaccinate persons under the age of 18 with the vaccine.
Should pregnant women be vaccinated?
There is currently insufficient data on the use of Sinovac-CoronaVac for the prevention of COVID-19 in pregnant women to evaluate the clinical effectiveness of the vaccine or the potential risks of vaccination during pregnancy. However, the vaccine is inactivated and contains an adjuvant that is widely used in many other vaccines, particularly hepatitis B and tetanus, and has a well-documented safety profile, including in pregnant women. Therefore, the epidemiological efficacy of the Sinovac-CoronaVac vaccine for the prevention of COVID-19 in pregnant women is expected to be comparable to that observed in non-pregnant age-matched individuals. The safety and immunogenicity of the vaccine in pregnant women is planned to be assessed in further studies.
WHO currently recommends the use of the Sinovac-CoronaVac vaccine to prevent COVID-19 in pregnant women when the benefits of vaccination outweigh the potential risks. To help pregnant women make informed decisions, they should be provided with information about the risks associated with COVID-19 during pregnancy; the likely benefits of vaccination taking into account the local epidemiological situation; and limited data on vaccine safety in pregnant women. WHO does not recommend a pregnancy test before vaccination. WHO does not recommend delaying pregnancy or considering termination of pregnancy because of vaccination.
Who else is suitable for this vaccine?
Vaccination is recommended in the presence of concomitant diseases that have been shown to increase the risk of severe COVID-19; these include obesity, cardiovascular and respiratory diseases.
The vaccine may be offered to people who have previously had COVID-19. These individuals are reported to have a low likelihood of clinically significant reinfection for up to six months after natural infection. Therefore, they may choose to delay vaccination and vaccinate towards the end of this period, especially in the face of vaccine shortages. In areas where variants of concern due to documented immune evasion are circulating, a shorter time period from infection to immunization may be recommended.
The epidemiological effectiveness of the vaccine among lactating women is expected to be similar to that among other adult populations. WHO recommends the use of the Sinovac-CoronaVac vaccine for the prevention of COVID-19 in women during lactation on an equal basis with other adults. WHO does not recommend stopping breastfeeding after vaccination.
People who are infected with the human immunodeficiency virus (HIV) and have compromised immunity are at increased risk of severe illness from COVID-19. Such individuals were not included in the clinical studies used by SAGE in the review, however, as this vaccine is non-replicative, individuals with HIV and immunocompromised status may be vaccinated if they are in the recommended population for vaccination. Where possible, they should be provided with the necessary information and advice to make an individual risk-benefit assessment.
Who is this vaccine not recommended for?
The vaccine is contraindicated if there is a history of anaphylactic reaction to any component of the vaccine.
Acutely ill patients with PCR-confirmed COVID-19 should not be vaccinated until the acute course of the disease has ceased and the requirements have been met to complete the isolation period.
If the body temperature rises above 38.5°C, vaccination should be postponed until the fever subsides.
What is the recommended dosage of the vaccine?
SAGE recommends two doses of Sinovac-CoronaVac vaccine (0.5 ml) intramuscularly. WHO recommends an interval of 2–4 weeks between the first and second dose. A two-dose regimen is recommended for all vaccinated individuals.
If the second dose is given less than two weeks after the first dose, it does not need to be repeated. If the waiting period for the second dose is longer than four weeks, it should be given as soon as possible.
How does this vaccine compare to other vaccines already in use?
Vaccines are not directly comparable due to differences in study design, but in general all vaccines approved by WHO for emergency use are highly effective in protecting against severe disease and hospitalization from COVID-19.
Is the vaccine safe?
SAGE carefully reviewed data on the quality, safety and clinical effectiveness of the vaccine and recommended its use for immunization of persons aged 18 years and over.
There is currently limited data on the safety of the vaccine in people over 60 years of age (due to the small number of participants in clinical trials).
Although there is no evidence to suggest a different safety profile for the vaccine in older people compared to younger age groups, countries considering using the vaccine in people over 60 years of age should actively monitor its safety on an ongoing basis.
As part of the vaccine's emergency authorization process, it has committed to continue to provide data on the safety, effectiveness and quality of the vaccine obtained through ongoing clinical trials and vaccination of the population, including older adults.
How effective is this vaccine?
In a large phase 3 clinical trial in Brazil, two doses given 14 days apart were 51% effective in protecting against symptomatic SARS-CoV-2 infection and 100% effective against severe COVID after 14 days of the second dose. -19 and 100% of hospitalization.
Does the vaccine protect against new variants of the SARS-CoV-2 virus?
In an observational study among healthcare workers in Manaus, Brazil, where the P.1 variant accounted for 75% of SARS-CoV-2 samples, the epidemiological effectiveness of protection against symptomatic infection provided by the Sinovac-CoronaVac vaccine was estimated to be 49. 6% (4). Efficacy data were also obtained from an observational study in Sao Paulo, where the P1 variant is circulating (83% of samples).
In areas of widespread circulation of the significant P.2 variant (also in Brazil), vaccine efficacy was estimated at 49.6% after at least one dose and was reported at 50.7% two weeks after the second dose. WHO intends to update its recommendations as new data becomes available.
SAGE currently recommends this vaccine as part of the WHO vaccine priority roadmap.
Does the vaccine prevent infection and transmission of the virus?
There is currently no specific data available on the effect of the Sinovac-CoronaVac vaccine on the transmission of the COVID-19 virus, SARS-CoV-2.
Until such data becomes available, WHO reiterates the need to comply with current guidance and maintain health and social measures as part of a comprehensive approach to preventing infection and transmission. These measures include wearing masks, maintaining distance from others, washing hands, respiratory etiquette and cough hygiene, avoiding crowds and keeping rooms well ventilated, as recommended by local and national authorities.
What does autohemotherapy treat?
There are a number of diseases for which the use of this method has shown the best results.
- Allows you to get rid of purulent processes in soft tissues, including diabetic wounds;
- Chronic inflammation of the respiratory system;
- Skin diseases (psoriasis, furunculosis, acne);
- Joint diseases;
- Sluggish and recurrent gynecological diseases;
- Immunodeficiency diseases, including all colds;
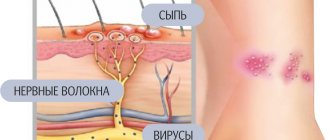
- Herpetic infections;
- Cytomegalovirus infection;
- Menopausal syndrome;
- Recurrent condylomas and papillomas.
REFERENCE. If, after testing, the patient is found to have a low hemoglobin level, autohemotherapy is postponed until the condition normalizes.
Scheme of autohemotherapy
The duration of treatment, the number of injections and the volume of injected biomaterial should be determined by the attending physician. There are several popular treatment regimens:
- Standard. Based on a gradual increase in the administered blood volume. The initial dose is 1 ml, with each subsequent session it increases by 2 ml. When the volume of injected biomaterial reaches 10 ml, the dose is reduced in the reverse order, bringing it to the original volume. On average, this course lasts up to 20 days.
- Stepped. Before repeated administration, the blood is diluted with a homeopathic medicine (depending on the disease). Usually administered at a time, intramuscularly.
- Introduction with ozone. It is believed that blood mixed with ozone increases its beneficial properties. Most often, this method is used in the treatment of gynecological diseases. There are two main schemes:
- Small autohemotherapy. Oxygen and ozone (5 ml) are drawn into the syringe, then venous blood (5 ml) and an intramuscular injection is performed.
- Major autohemotherapy. About 150 ml of venous blood is taken from the patient, placed in a container with a coagulant and up to 300 ml of a mixture of ozone and oxygen is added. The solution is mixed and administered dropwise.
- Hemopuncture. These are subcutaneous injections into reflexogenic zones.
- Blood transfusion using calcium gluconate. Used in dermatology. Only a doctor can select the exact dose to avoid convulsive syndrome.
Vaccinal prevention
Preventive treatment of infections with serum began to actively develop in the 19th century. The first drug was invented by E. Jenner in the 18th century. He found that milkmaids who come into contact with cows that have smallpox blisters on the udder suffer from smallpox less often. Jenner conducted a successful experiment: he rubbed a liquid taken from an animal's chicken pox vesicles under the boy's skin, and 30 days later he infected the child with smallpox. The boy remained healthy and developed antibodies to smallpox in response to exposure to the microbe.
Later, microbiologist Louis Pasteur proved that the causative agents of diseases are microorganisms; a person cannot become infected with an infectious disease again. Scientists have begun to create products from weakened microbes that prevent the occurrence, development, and spread of many dangerous infections.
From the end of the 20th century to the present day, vaccination of citizens in Russia has been mandatory and is regulated by the National Vaccination Calendar.
Vaccine prevention is aimed at improving the health of Russians, their quality of life, reducing mortality and disability from complications caused by infectious diseases. For prevention, doctors use vaccines; to alleviate the conditions of infected patients, they use medicinal serums. Let's take a closer look at the main differences between these drugs.