Olga Dmitrieva Heritage June 05, 2020
In 1890, the Imperial Institute of Experimental Medicine was founded in St. Petersburg. In his laboratories, researchers made worldwide scientific discoveries and created vaccines that saved millions of lives. One of these scientists was Anatoly Aleksandrovich Smorodintsev, who connected his life with the institute in 1926.
REPRODUCTION, PHOTO by the author
Virologists are a special caste. Their work is associated with mortal risk, and the life of Academician Smorodintsev can safely be called a war, divided into separate stages - battles with such terrible enemies of humanity as influenza, measles, polio and tick-borne encephalitis.
As for the latter, nothing was known about it until the strange epidemic that broke out in the early 1930s in the Far East. People were afraid to go to the taiga, claiming that evil spirits had settled there, causing death and incurable damage to the body and brain. Doctors called the disease toxic flu, until in 1937 an expedition led by the outstanding scientist Lev Zilber (brother of the writer Veniamin Kaverin) arrived in the taiga region. He managed to establish the nature of the disease and its connection with a previously unknown virus and forest tick bites. But Zilber failed to continue his work: following a false denunciation, he was arrested and sent to a camp.
The next stage of the expedition was led by Academician Evgeny Pavlovsky and Anatoly Smorodintsev. The work was difficult and there were losses: several people became infected, became disabled, and died. But this did not stop scientists, and as a result of their research, a vaccine against tick-borne encephalitis was created, which began to reliably protect everyone who traveled to Siberia and the Far East for the first time.
Related article:
The insidious “influenza”. How Russia and the world fought the flu
Since the early 1950s, Anatoly Smorodintsev studied polio viruses at the IEM. It was then that outbreaks of this disease began to acquire enormous proportions; epidemics most often affected the USA, Sweden, and England. The disease, which affected the respiratory system, claimed thousands of lives, acquiring the character of a global disaster. Therefore, special pressure chambers for artificial ventilation of the lungs - the so-called “iron lungs” - became a symbol of the polio epidemic.
Hope arose when American virologists Jonas Salk and Albert Sabin managed to create vaccines against polio, but Salk's killed vaccine was expensive and its effect was not one hundred percent. Sabin had not yet finalized his live vaccine, and its production in the United States was not authorized.
In the same 1950s, polio first caused a major epidemic in the USSR. Tens of thousands of people fell ill, but information about this was prohibited. No deaths were reported either. The Ministry of Health was powerless; there were no means of combating the disease.
In 1955, with the help of Anastas Mikoyan, the Institute of Poliomyelitis and Viral Encephalitis was created in Moscow. It was headed by academician Mikhail Chumakov. The disease was officially recognized, and a group of scientists was sent to the United States, which included Marina Voroshilova, Mikhail Chumakov and Anatoly Smorodintsev, who had already begun work on obtaining a live polio vaccine, but he was unable to create harmless weakened strains of the virus.
Sabin agreed to provide his strains for testing, and soon after the delegation returned to the IEM, a package containing thermoses with live vaccine viruses arrived. Scientists were faced with a daunting task - to weaken their ability to cause disease, but at the same time maintain the ability to provoke an immune response in the body. Huge work lasted two years, and finally a life-saving live polio vaccine was created.
Smorodintsev had to prove its harmlessness, and virologists traditionally tested it on themselves by drinking a liquid containing vaccine strains. The vaccine should then be tested on young children who had no immunity to the disease. But it was impossible to find a family that would voluntarily provide a child for a dangerous experiment, and then Smorodintsev offered to test the vaccine on his five-year-old granddaughter Lena.
For two weeks of the experiment, everyone waited with trepidation for the appearance of antibodies that would cause an immune response. Finally, when this happened and Lena did not get sick, it was decided to give the vaccine to the children of some other department employees. They also did not get sick and acquired complete immunity to the virus. The live vaccine made it possible to avoid painful injections; they began to place it in pills, which children swallowed like candy. There were some oddities: in some places, pills with the vaccine were sold in confectionery departments, and the little grandchildren of one scientist stole an entire package with a hundred pills from the refrigerator and ate them. Fortunately, no one except the grandmother, who fainted from horror, was injured.
In 1959, about two million children in the USSR were vaccinated with the vaccine. Widespread immunization led to a sharp decrease in the incidence, and in some areas to its complete elimination. At the Institute of Poliomyelitis, Mikhail Chumakov established the production of vaccines, and it soon had to be expanded, as desperate requests began to come from many countries to save children. The mothers of Japan even staged a march demanding vaccination with the miraculous “Russian vaccine.”
The Smorodintsev family repeated their feat once again when, under the leadership of a scientist at the Pasteur Leningrad Institute of Epidemiology and Microbiology, a vaccine against measles was created. It is now widely used all over the world, and Anatoly Alexandrovich tested it on his other granddaughter, Lisa.
One can also add to the list of Smorodintsev’s achievements the creation under his leadership of vaccines against mumps and influenza. And in 1967, he founded and headed the Influenza Research Institute: the scientist was rightfully considered one of the world's leading authorities in the field of research on this disease.
…Smorodintsev’s students say that if he had done nothing in his life other than creating a vaccine to fight polio, then even then he would have been worthy of the deepest gratitude of all mankind. But the best assessment of the scientist’s achievements was given by his great-granddaughter Masha. She wrote in the abstract: “Since childhood, I heard that you shouldn’t be afraid of doctors, you shouldn’t cry when you get vaccinated, because almost all of them were invented by grandfather Tolya.”
.
The best essays are collected in the books “Heritage. Favorites" volume I and volume II. They are sold in bookstores in St. Petersburg, in the editorial office on the street. Marata, 25 and in our online store.
Read even more interesting essays on our channel in Yandex.Zen.
#scientists #medicine #discoveries #vaccination
The material was published in the newspaper “St. Petersburg Vedomosti” No. 096 (6694) dated 06/05/2020 under the title “Virus Winner”.
Share on VKontakte Facebook
Cool
Crippling Virus
The infection enters the body through the mouth. If the immune system is strong, the infection quickly capitulates. If not, it penetrates the blood and reaches the nerve cells of the brain and spinal cord. 25% of spinal cord neurons are killed - and the patient develops paresis - partial loss of motor function. 75% is already paralysis. After the death of neurons, the muscles of the limbs (usually the legs) atrophy. Because of this, bones do not grow, and joints stretch unevenly and bend.
Electron micrograph of polio virus. Photo: Public Domain
In 1890, Swedish pediatrician Karl Oskar Medin discovered the infectious nature of polio, but could not find the culprit of the infection. 19 years later, Karl Landsteiner and Erwin Popper . They proved that the causative agent of polio is a virus from the picornavirus family.
Symptoms of polio
Mostly occurs in an asymptomatic or erased form. Sometimes it happens that poliovirus penetrates the central nervous system and multiplies in motor neurons, which leads to their death, irreversible paresis or paralysis of the muscles they innervate.
The polio virus causes signs of intoxication: nausea, vomiting, diarrhea, rash; cold-like disorders: cough, runny nose, sore throat, difficulty breathing and swallowing; fluctuations in blood pressure, fatigue, general poor health, headache; in rare cases - various types of paralysis that can lead to the death of the patient.
The disease with clinical manifestations is classified as abortive poliomyelitis and paralytic or non-paralytic poliomyelitis.
Most clinical cases of abortive polio, especially among young children, are mild: 1–3 days of mild fever, malaise, headache, sore throat, and vomiting that develop 3–5 days after infection. There are no neurological symptoms or signs, and physical examination reveals nothing other than fever.
Approximately 4% of patients with poliovirus infection develop nonparalytic central nervous system involvement with aseptic meningitis. Patients usually complain of neck stiffness and/or back pain, and headaches that appear after several days of prodrome, similar to abortive polio. Manifestations last from 2 to 10 days.
Common manifestations of paralytic poliomyelitis, in addition to aseptic meningitis, include deep muscle pain, hyperesthesia, paresthesia and, with the development of active myelitis, urinary retention and muscle spasms. Asymmetric flaccid paralysis may occur and progresses over 2–3 days. Sometimes signs of encephalitis predominate.
Enemies and allies
Summer 1921. In the USA there is a disaster on a national scale. In the east of the country, two thousand people, most of them children, die from a polio outbreak within three months. Seven thousand patients remain paralyzed. The peak of the epidemic in the United States was 1952. 58 thousand sick! 10% of them, mostly children, died from complications - pneumonia and paralysis of the respiratory muscles.
In the USSR, the polio epidemic began 30 years later. The problem of disease prevention was quickly elevated to the rank of the most important government tasks. In Moscow, the work on creating a vaccine was led by Mikhail Chumakov , director of the new polio institute. In Leningrad, the Department of Virology of the Institute of Experimental Medicine, headed by Academician Anatoly Smorodintsev, . But Soviet scientists received help from where they did not expect - from the USA. In 1953, American virologist Jonas Salk introduced the world to the first “killed”, that is, inactivated, vaccine. It was based on poliovirus grown in the kidney tissue of African monkeys and chemically “turned off” with formaldehyde.
Vaccine against fear. How the USSR and the USA defeated polio together Read more
Mass vaccination in America began in April '54. And it ended in a huge scandal. Hundreds of vaccinated children became infected with polio. The US Public Health Service investigated and found that some batches of vaccines contained live rather than neutralized virus. Obviously, the manufacturers violated the technology. At this moment, another American virologist, Albert Sabin , risked introducing a new type of polyvaccine - live! He was convinced that a live oral vaccine would produce more reliable immunity. But there was no chance of testing, much less vaccination, in the United States after the scandal with the “killed” vaccine. And then Albert Sabin makes a historic decision. At the height of the Cold War, the scientist transferred all his work to his Soviet colleagues - M. Chumakov and A. Smorodintsev. Science turned out to be higher than politics. Work was in full swing at the Leningrad Institute of Experimental Medicine and the Moscow Research Institute of Poliomyelitis. In the fall of 1956, the first tests began.
Photo: Flickr.com
Tested on my granddaughter
While testing a new vaccine, scientists from the Department of Virology at the Leningrad Institute of Experimental Medicine take a risk: they drink a glass of water in which a “tamed” strain of the disease is diluted. The risky experiment is successful, but for the final stage of testing, not an adult is needed, but a child - healthy and not immune to a dangerous disease.
It was impossible to find parents who would voluntarily agree to vaccinate their child with a live experimental vaccine. And then Academician Anatoly Smorodintsev brings the finished drug to his home. At dinner, he drips it onto cookies and treats his six-year-old granddaughter Lena to them... The tense days of waiting begin. Every day the girl is examined by several doctors: they measure her temperature, check her reflexes, conduct tests... After two weeks, antibodies appear in Lena’s blood! She's protected! This day becomes a holiday for Lena’s grandfather, all his colleagues and, of course, the “father” of the live vaccine - Albert Seibin. By 1963, instead of tens of thousands of cases, only a few hundred cases of infection were registered in the USSR. The epidemic is on the decline. Since the mid-60s, the Soviet live vaccine has been exported.
Institute of Poliomyelitis and Viral Encephalitis of the USSR Academy of Medical Sciences (now named after M.P. Chumakov RAS). Production of polio vaccine under completely sterile conditions. 1963 Photo: RIA Novosti/ Lev Ustinov
Vaccination in a new way
Half a century later, the World Health Organization nevertheless took steps to switch from a live vaccine to a “killed” vaccine. There are a number of reasons for this. Firstly, there has been no mass morbidity for a long time. Secondly, the live virus, although weakened, can be released into the environment for another two months and infect unvaccinated people. As a result, the virus mutates, new strains emerge that can cause dangerous disease. The first Russian inactivated polio vaccine is produced by a biotechnological complex in the Kirov region. It is a suspension of “killed” polio viruses and is effective against three types of pathogen at once. It can be combined with any vaccinations of the National Calendar, with the exception of anti-tuberculosis and BCG. Since the drug does not contain a live virus, it can be vaccinated against weakened children, pregnant and lactating women, and even patients with immunodeficiency.
Life-saving vaccine. How are vaccines developed today? More details
There are contraindications. Be sure to consult your doctor.
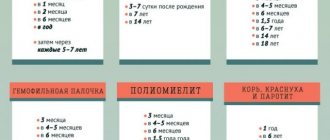
Polio vaccination today
Today in Russia, the National Vaccination Calendar is designed in such a way that the first two polio vaccinations are given with an inactivated vaccine (IPV), and all subsequent ones are given with a live vaccine (OPV). Moreover, if the parents wish, all OPV can be replaced with IPV, but not vice versa.
Unfortunately, thoughtless compliance with WHO requirements in our country leads to the fact that the risk of contracting polio does not decrease, but increases. But, as usual, not for everyone. Those at risk include large families, people with low incomes - in general, all those who cannot afford to have their children vaccinated at a cost of several thousand per injection.
To help the reader understand why this happens, let's compare IPV and OPV, and then look at how exactly WHO recommends using these vaccines to combat polio.
OPV
The live polio vaccine has many advantages.
Firstly, the immunity formed as a result of vaccination is very reliable. Unlike IPV, after OPV the body builds protection against the polio virus in the intestines. Therefore, a person vaccinated with OPV not only receives personal immunity to wild poliovirus, but also cannot become its carrier.
Secondly, OPV is extremely convenient for universal vaccination. The work of a nurse is greatly simplified (in the middle of the last century this was especially critical), there is no need to give injections. Moreover, even if there is a small percentage of unvaccinated children in the country, they will receive indirect vaccination from those who have recently received OPV. After all, each vaccinated person secretes the vaccine virus for about two weeks (and up to 60 days) after vaccination. Children playing in the same sandbox will infect each other with vaccine strains, and eventually everyone will develop immunity. By the way, the creators of the vaccine, M.P., were especially proud of this “sandbox immunity.” Chumakov and A. Seibin.
Third, OPV is relatively easy and cheap to produce. In the 1960s, the Polio Research Institute alone provided the vaccine not only to the entire Soviet Union, but also to half the world in addition. IPV is much more expensive and difficult to manufacture, and it is because of this that the latest WHO requirements have caused problems in many regions of the world, including Russia.
Fourthly, with mass vaccination with OPV, the wild virus is forced out of nature and dies out. There are many similar examples in living nature. Thus, the North American Carolina squirrel is now displacing the common squirrel from Europe. Sosnovsky's hogweed is taking over Russian fields, and all wastelands are overgrown with American maple. Typically, such invasive species of animals and plants disturb the biological balance and therefore need to be controlled. But in the case of the polio virus, replacing the harmful wild virus with a vaccine virus is a benefit for all people.
But OPV also has disadvantages.
The first and most important disadvantage of OPV is that vaccinated people are at risk of developing vaccine-associated paralytic polio (VAPP). The likelihood of illness is negligible, but it exists. Different sources provide slightly different information.
WHO provides the following statistics: 1 case of VAPP per 2.7 million newly vaccinated people. (*) Russian sources say that VAPP occurs on average in 1 in 0.7 million, while it is clarified that VAPP occurs more often in children with immunodeficiencies and that very young children, protected by maternal antibodies, almost never get VAPP. Apparently, WHO collected statistics on all vaccinated people without taking into account their age, so according to WHO, VAPP is four times less common. [1][5][19]
(*) After the second dose, OPV is very rare, since immunity to the virus has already been formed. According to WHO, the statistics are 1 case in 6.7 million.
The clarification of Russian scientists means the following: with the first dose of OPV at the age of three months (as was the case in the Soviet vaccination calendar), the likelihood of VAPP is negligible. But if you start vaccinations later - approximately 1: 700,000, children with immunodeficiencies are at risk. Out of 2000 cases of VAPP, only 1 is in a child without immunodeficiency. That is, a healthy, timely vaccinated child without immune disorders is practically not susceptible to VAPP. [19][2][5]
The second drawback of OPV has nothing to do with Russia, but it is worth mentioning. In countries where less than half the population has been vaccinated, the virus from the vaccine can be transmitted for a long time along the chain from one unvaccinated person to another. In Russia, almost everyone has still been vaccinated (mainly thanks to the older generation), so the vaccine virus after vaccination will be transmitted to 1-2 people, and that’s it - the rest are immune, there is no one else to transmit. But if there are few vaccinated people, then the vaccine virus can circulate for a very long time (the key word is long) among the unvaccinated part of the population. This is dangerous because the vaccine strain can degenerate back into a wild virus. In the end, no one has canceled random DNA mutations and the process of evolution. The vaccine obtained in the laboratory is constantly tested, but if the virus begins to travel uncontrollably from one person to another, then there is a possibility of mutation. This probability is negligible and, let us remind you, in countries with a high percentage of vaccinated people, such an event is impossible.
So, the main disadvantage of OPV is the likelihood of VAPP. It may be insignificant, but in one out of several million cases it still happens. WHO suggests combating VAPP with IPV. In theory this is absolutely correct, but in practice it leads to sad consequences. This will be discussed after a brief reminder about IPV and its properties.
IPV
Many years have passed since the Salk vaccine, and the technology for making IPV has been improved. If previously the vaccine worked for two out of three children, today almost all vaccinated people are protected. Immunity lasts for life. Therefore, if we talk only about the protection of a particular child, it does not matter whether the child is vaccinated with OPV or IPV.
The main advantage of IPV over OPV is the zero risk of VAPP. If after vaccination with OPV paralytic poliomyelitis occurs in one case out of several million vaccinated people, then after IPV it never occurs. Moreover, it is enough to get one IPV vaccine before all other OPVs and that’s it, VAPP will definitely not happen.
The main disadvantage of IPV is that this vaccine does not form local immunity in the intestine: specific intestinal IgA is not formed (unlike OPV). That is, a child vaccinated with IPV can spread the virus, although he will not get polio himself. Studies have shown that children who were vaccinated with OPV after IPV shed the vaccine virus for a slightly shorter time than children vaccinated with OPV alone. But the spread of the virus still occurs, although it is worse than without IPV at all.
Minor disadvantages of IPV compared to OPV - an injection is needed, a vaccinated person cannot “share” his immunity with unvaccinated people.
This is where the purely medical differences between IPV and OPV end. Before moving on to the so-called “economic” differences, let’s consider the use of IPV in the case when the following conditions are met:
- There are no, not even the slightest, flaws in the production of the vaccine;
- The vaccine is available to everyone, without exception, in every country in the world.
Considering the high cost and complexity of producing IPV, this case is far from reality. However, it should be considered to understand WHO's intentions.
WHO's polio eradication strategy can be boiled down to three steps.
- We vaccinate everyone with OPV. A harmless vaccine strain displaces the wild virus. As a result, only vaccine strains circulate in society, and the wild virus dies out.
- Let's move on to IPV. Distribution of the remaining vaccine strains in the world is difficult. They too are gradually dying out.
- Now you can completely forget about vaccination. Polio, like smallpox, is a thing of the past.
In the “ideal” case under consideration, there seems to be no catch. From a scientific point of view, every step of the WHO strategy is fully justified. The catch here lies precisely in the peculiarities of the production of IPV.
The first and most important disadvantage of IPV is the high cost and complexity of production. There are not many pharmaceutical companies in the world that produce IPV. (*) Scarcity and monopoly lead to higher vaccine prices in addition to high production costs.
(*) There are several reasons why pharmaceutical companies refuse to manufacture IPV. The first is associated with the tragedy at the production of the Salkov vaccine in 1955, when more than 200 vaccinated children fell ill with polio due to an error by the pharmaceutical companies Cutter and Vieth. Since then, not everyone is ready to take responsibility for the production of such a complex drug: in America, every defect is punishable by huge compensation to the victims. Another reason is that IPV manufacturing companies do not want to lose their monopoly on production.
The second disadvantage of IPV is related to possible errors in production. Of course, after the tragic mistakes of the pharmaceutical companies Cutter and Viet in 1955, quality control of finished products became very serious. The likelihood that wild polio virus will get into the vaccine is almost zero. The problem here is different. If a live wild virus is encountered at least somewhere in the production of a vaccine (and it cannot be found there), then this virus can simply “escape” from the laboratory. There is always the possibility of such an error. There have already been two cases of detection of laboratory viruses outside of production. One of them is the son of a factory worker who produces IPV. I would like to note that we are talking about 1997, and not about the 1950s, when production was just beginning and mistakes could not be avoided. [20]
The problem of wild virus in production has already begun to be solved in Japan. Since 2012, they have been producing IPV based on harmless Seibin strains.
Of the three problems with IPV—scarcity, high cost, and the danger of the wild virus—the first two are the main ones. Specifically in our country, the thoughtless policy of the Ministry of Health, coupled with a shortage of IPV, has led to the fact that very few children in Russia receive the necessary polio vaccinations on time.