BRIEF HISTORY OF BCG
The first thoughts about the possibility of creating an anti-tuberculosis vaccine came from the French microbiologist Albert Calmette and veterinarian Camille Guérin when they worked at the Pasteur Institute in Lille in 1908.
Scientists have noticed that on a nutrient medium based on glycerin, bile and potatoes, tuberculosis bacilli of the least virulence grow, and, therefore, you can try to grow a culture of weakened tuberculosis microbes. By 1919, scientists had created a strain that did not cause tuberculosis in experimental animals and were thinking about testing it on humans. But it was only on July 18, 1921 that the first BCG vaccinations were given. In the beginning, it often happened that “something went wrong”: for example, in Lübeck, Germany, all of the 240 vaccinated newborns fell ill with tuberculosis, and 77 of them died. But the investigation showed that it was not the BCG vaccine that was to blame, but the negligence of the doctor who stored it in the same container with a culture of classic tuberculosis microbes.
Albert Calmette, 1930
In 1925, Calmette transferred his vaccine to his Soviet colleagues and the BCG vaccination began to be actively used in the USSR. Just 3 years later, it turned out that mortality from tuberculosis in groups of vaccinated children actually decreased. In 1928, it was recommended to vaccinate newborns from “risk groups” with BCG. Since the mid-1950s, vaccination of newborns has become mandatory in most European countries (except perhaps the Netherlands). Also, in 1948, India was the first non-European country to introduce compulsory vaccination; in 1967-1968, Brazil; vaccination is mandatory in Singapore, Malaysia and many other countries. But since the late 1990s, several European countries have stopped using BCG for mass vaccination, citing low incidence of tuberculosis among their citizens.
I will try to simply and briefly talk about the main vaccinations that must be given to a child in the first years of life according to Russian standards. Everything is very simple.
So, first thing. BCG.
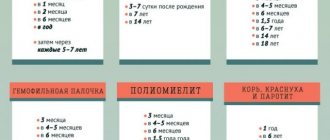
1. Every Russian maternity hospital offers two vaccinations: BCG and the first of three vaccinations against hepatitis B.
2. Then, in the first year, according to the national calendar, the baby will have to receive only 1 more vaccination - whooping cough + diphtheria + boletus + polio (it is done three times in 1.5-2 months). Well, repeat the hepatitis B vaccination if it was done in the maternity hospital (it is also done three times).
3. After a year, vaccination against measles + rubella + mumps is given, and then only revaccinations!
BCG is given in the first 3-7 days, in the absence of contraindications, in the shoulder, and if the Mantoux test is negative, revaccination is repeated at 7 and 14 years of age.
Robert Koch
1. Why do they start with it and how to get infected with it?
They start with BCG because it is believed that there is now a tuberculosis epidemic in our country and there is a very high risk of a newborn baby becoming infected with tuberculosis. It is caused by mycobacteria and is transmitted through the air by sneezing, talking, coughing. Mycobacteria can fly in an elevator, restaurant, airport or subway. In general, the risk of meeting him is high.
Therefore, BCG was traditionally done in the maternity hospital. In addition, it is believed that children more often become ill with tuberculosis during the initial “encounter” with mycobacteria and become more severely ill. In a number of European countries, this vaccination is not carried out because it is believed that the epidemic situation there is favorable (there is currently an ongoing tuberculosis epidemic in Russia).
2. What to do if BCG was not done in the maternity hospital?
Sometimes, for some reason, the child is not given this vaccination in the first days. Then it can be done to the child at your place of residence at any time convenient for you (when you mature, if you are afraid, or when you begin to “go out into the world” with your child). But if you do it after 2 months, you will have to do a Mantoux test first. This is not a vaccination, it is just a test to determine whether the child has already become infected with tuberculosis (in this case, the vaccination is not needed, they will be sent straight to a TB specialist). Sometimes the Mantoux reaction is false-positive, allergic reactions to Mantoux components (to tuberculin) are often observed - then you can do a control so-called Diaskin test, it is more sensitive, and after its result you can decide whether you need to see a phthisiatrician .
3. Complications from vaccination.
BCG is an almost live vaccine, however, the incidence of complications is low even in immunocompromised individuals. Here is what the World Health Organization writes about this: “Complications after BCG vaccination are rare: the incidence of lethal BCG dissemination is estimated at 0.19-1.56 per million vaccinated individuals, and its victims are almost exclusively unintentionally immunized individuals with severe cellular disorders immunity. Significant local reactions, such as extensive local ulceration and regional lymphadenitis, occur in <1:1000 and in the majority of cases (>90%) in immunocompromised individuals. Reports of osteitis have been associated with the use of certain batches of the vaccine, but it is now extremely rare. Because acute adverse events with BCG vaccination are extremely rare, even among HIV-positive infants without clinical signs, all healthy newborns should be vaccinated with BCG, even in HIV-endemic areas.”
4. How does it combine with other vaccinations?
BCG is the only vaccine that is not recommended to be administered together with other vaccines. An interval of approximately 1-1.5 months should be maintained.
Thus, if the vaccination was given to a healthy child in compliance with all the rules for administering the vaccine, it is practically safe, but it greatly reduces the risk of severe forms of tuberculosis in our country, where there is currently an epidemic. If you did not have it done in the maternity hospital, it can be done later, but only after the Mantoux reaction (or Diaskin test) and no earlier than 1 month after/before other vaccinations. The Mantoux test is not a vaccination and is performed after the first year of life every year until adulthood.
Children co-infected with tuberculosis and HIV in Myanmar. © 2012 Matthieu Zellweger (with AIDSpartners.org)
Unfortunately, in society there is very, very little knowledge about tuberculosis, especially regarding the problem of vaccinations against tuberculosis and Mantoux tests (tuberculin diagnostics).
Why is this vaccination needed? And why, despite the fact that everyone is vaccinated, many people get tuberculosis?
BCG vaccination is needed to prevent tuberculosis in children. It does not protect against infection with the causative agent of tuberculosis, but it really protects against the transition of a latent infection into an overt disease (in about 70% of those vaccinated), and almost 100% protects children from severe forms of tuberculosis - from tuberculous meningitis, tuberculosis of bones and joints and severe forms pulmonary tuberculosis. It was the use of the BCG vaccine that made it possible to achieve a significant reduction in the incidence of tuberculosis in children in general, and in particular, for many years, despite the difficult social situation, we have not seen cases of tuberculous meningitis in vaccinated children.
The BCG vaccination, as a rule, is done in the maternity hospital on the fourth day of the child’s life, in the left shoulder, at the border of its upper and middle third.
Why so early? The fact is that, unfortunately, the situation with tuberculosis in society is unfavorable, and not all tuberculosis patients who secrete the pathogen know about their disease, accordingly they do not receive treatment and are contagious. Therefore, a child can encounter Mycobacterium tuberculosis very, very early. And phthisiatricians have long known that the earlier a child is infected, the greater the likelihood of the infection turning into a disease and the more unfavorable the course of the disease will be. That’s why vaccinations are done as early as possible, so that the child has time to develop immunity so as not to get sick. And in this regard, let me remind you of the old rule - you should not show your newborn to any strangers for up to a month.
The BCG vaccine is a weakened vaccine strain that cannot cause tuberculosis, but allows the development of immunity against this disease. Since immunity against tuberculosis is developed only when the pathogen or its vaccine replacement is present in the body, it is impossible to make a killed vaccine, therefore the same BCG vaccine from different manufacturers is used in all countries (many parents often ask about imported vaccines, because they think they are better). Moreover, the domestic vaccine, it seems to me, is better, because both vaccinators and pediatricians have a lot of experience working with it. In addition, imported vaccines may be held in customs for quite a long time or may end up in unsuitable conditions, and since the vaccine is live, its storage conditions must be very strict.
There is a variant of the BCG vaccine - the BCG-M vaccine, which contains half as many microbial bodies as the regular vaccine. The BCG-M vaccine is used to vaccinate weakened and low birth weight premature babies, and usually this vaccine is no longer used in the maternity hospital, but where the child will be transferred from the maternity hospital.
Usually, the BCG vaccine, unlike, say, the DPT vaccine, is well tolerated, but complications of vaccination are possible, and here I will remind you of this so that parents know what to pay attention to.
But first, a few words about the normal course of the post-vaccination process, since there are surprisingly many questions on this topic.
Normally, 6-8 weeks after vaccination (that is, at one and a half to two months), a post-vaccination reaction begins - a previously invisible whitish nodule rises on the skin, at first resembling a mosquito bite, and then a bubble filled with a light yellow liquid appears at the site of vaccination, then (usually by 3-4 months) the vesicle bursts, the grafting site becomes covered with a crust, which comes off several times and appears again.
All this is a completely normal process, and not a “terrible abscess”, as some parents describe. No special care is needed for the vaccination site; you cannot lubricate the abscess with any disinfectants, iodine, brilliant green or ointments - this can kill the rather unstable vaccine strain and disrupt the course of the post-vaccination reaction.
What should parents be wary of? The fact is that it is rare, but it happens that the vaccine gets subcutaneously, and not intradermally, and suppuration forms, but under the skin, while outwardly there is no abscess, there is a pea under the bluish skin. There may also be enlargement of the lymph nodes in the left armpit. All of these are signs of a possible complication of BCG vaccination, and you should definitely bring this to the attention of your local doctor.
Now, in the wake of the fashionable anti-vaccination craze, some parents believe that vaccinations are harmful, since they contain phenol, mercury and all that stuff. The fact is that the BCG vaccine does contain preservatives, but without this you cannot make a live vaccine, and one more thing - there is much more rubbish in our tap water than in the vaccine. However, if parents decide that their child does not need vaccination, they have every right to refuse it; this point is clearly stated in our legislation. Such parents sincerely want to say only one thing - this is your child and it is you who take responsibility for refusing vaccinations, in particular BCG. In this case, parents must write in their own hand on the child’s record a refusal to undergo preventive vaccinations and indicate that they had the opportunity to ask all the questions they were interested in and will not have any claims against the medical institution.
Tuberculosis in children
There are the following stages of tuberculosis in children (so, for general information. To know what we are vaccinated against):
- primary infection - local inflammation occurs at the site of infection. From here, the bacteria penetrate the nearest lymph nodes, and the so-called “primary complex” is formed. In most cases, general well-being is only slightly affected. You may experience fatigue, weight loss, loss of appetite, night sweats, and dry skin. In most cases, the infectious focus calcifies and the development of tuberculosis stops at this stage.
- latent (hidden) infection - due to the weakening of the body’s defenses, the pathogen may spread from a fresh or calcified lesion and form numerous lesions in other organs (lungs, spleen, liver, brain, meninges, bones). Tuberculous meningitis (inflammation of the meninges) and bone tuberculosis are especially dangerous for children.
- recurrent tuberculosis of the adult type - manifests itself as tuberculous damage to many organs, accompanied by fever and significant loss of strength. Most often, the lungs are affected with the formation of cavities (cavities), which can break into the bronchi, as a result of which pathogens are released out (open form of tuberculosis).
In 90-95% of cases, the primary infection goes unnoticed, leaving only positive tuberculin tests and latent infection, and the latter can become active at any age (it’s like a time bomb).
Vaccination against tuberculosis.
The main factor determining the occurrence and course of the disease is the state of the body's defenses. Unfavorable social conditions and previous weakening of the body due to other, primarily chronic diseases, contribute to the occurrence of tuberculosis.
Vaccine effectiveness.
Research results are mixed and vary from country to country. In the UK, studies of 50,000 children showed an 80% reduction in the risk of infection after vaccination. The results in the US are not as impressive. However, recent studies have shown that after vaccination, the risk of pulmonary tuberculosis is reduced by 2 times, and mortality by 71%.
The results of Russian studies have shown that unvaccinated children get tuberculosis 15 times more often than those vaccinated in a timely manner and according to all the rules.
Anti-tuberculosis vaccination in vaccinated children induces immunity to tuberculosis infection. When entering the body of a child vaccinated with the BCG vaccine, Mycobacterium tuberculosis usually does not cause severe forms of tuberculosis that develop as a result of primary infection (tuberculous meningitis, miliary tuberculosis, caseous pneumonia, extensive infiltrates in the lung with the formation of a primary cavity). However, the BCG vaccine does not protect against tuberculosis infection, i.e. from the penetration of mycobacteria by aerogenic or elementary routes and the development of primary tuberculosis infection, which is accompanied by the occurrence of local forms of primary tuberculosis in 7–10% of those infected. In vaccinated children, primary infection usually goes unnoticed, and it is often not detected or diagnosed when the tuberculin reaction changes, which in those who have had a primary infection remains positive for life. Such persons are called tuberculosis infected.
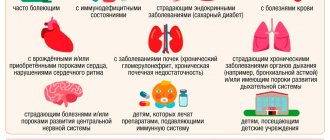
Vaccination is recommended:
— In countries where the number of people infected with tuberculosis is more than 1%.
— Children whose family has tuberculosis patients.
When is BCG done?
BCG vaccination is given to newborns; if the vaccination was not given in the maternity hospital, then it must be taken care of during the first 6 weeks of the baby’s life. Until six weeks of age, a tuberculin test (Mantoux) is not needed. For children over 6 weeks of age, the vaccine is administered only if the reaction to tuberculin is negative, in order to avoid complications due to possible infection.
The BCG TB vaccine is not effective if it is given to someone who is already infected.
Side effects of BCG vaccination.
As a rule, they are local in nature and include subcutaneous “cold” abscesses (ulcers), which occur when the vaccination technique is violated, and inflammation of local lymph nodes. Keloid scars, bone inflammation and widespread BCG infection are very rare, mainly in children with severe immunodeficiency.
During the entire period of use of the vaccine (more than 100 million people were given), only 24 deaths were observed, almost all of the dead suffered from immunodeficiency.
Contraindications to BCG vaccination.
Absolute (constant):
- primary immunodeficiencies - HIV infection - malignant blood diseases - neoplasms - there were severe reactions to the previous administration of BCG. — Tuberculosis
Temporary:
— intrauterine infections — hemolytic disease — severe prematurity (<2000 g). - skin diseases - therapy is carried out with large doses of corticosteroids or immunosuppressants;
Permitted drugs:
BCG, BCG-M Vaccine against tuberculosis. Production: Russia
Ingredients: live weakened mycobacterium tuberculosis strain BCG-I. One dose contains 0.05 mg of the drug (BCG) or 0.025 mg (BCG-M)
Contraindications to vaccination of newborns:
— prematurity II-IV degrees; — intrauterine hypotrophy III-IV degree; - intrauterine infection; — purulent-septic diseases; — hemolytic disease of newborns (moderate and severe forms); - generalized skin lesions; - acute diseases; - generalized BCG infection detected in other children in the family;
Tuberculosis vaccine
The anti-tuberculosis vaccine was created in 1921 by French scientists Calmette and Guerin, hence its name (Bacille Calmette-Guerin, abbreviated as BCG, and in Russian designation BCG). In the first years of use, the vaccine was used to create artificial immunity in newborns by administering it with expressed mother's milk. Subsequently, a cutaneous vaccination method was developed and introduced. Currently, the vaccine is administered intradermally (i.c.) into the forearm in the maternity hospital. Since 1991, the BCG-M vaccine has also been used, in which the dose of the bacterial mass is halved, which makes it possible to use it for immunization of premature newborns and weakened children.
Vaccinations are administered by a specially trained nurse.
In the medical record, the doctor on the day of vaccination (re-vaccination) must make a detailed entry indicating the results of thermometry, a detailed diary, the appointment of administration of the BCG vaccine (BCG-M) indicating the method of administration (i.c.), dose of the vaccine (0.05 or 0.025 ), series, number, expiration date and vaccine manufacturer. The passport data of the drug must be personally read by the doctor on the packaging and on the ampoule with the vaccine (usually, if it is given in a maternity hospital, all the data about the vaccination is written in the discharge summary, you can look it up).
Before vaccination (re-vaccination), the doctor and nurse must read the instructions for using the vaccine, and also inform the parents of the child (adolescent) in advance about immunization and the local reaction to the vaccine. And you must sign informed consent to perform BCG.
Vaccinations at home are allowed in exceptional cases by the decision of the commission, which must be recorded in the medical record, and are carried out in the presence of a doctor. Vaccination of newborns in a maternity hospital (pathology department) is allowed in the children's ward in the presence of a doctor. In these cases, the formation of the vaccination setup is carried out in a special room.
All items necessary for BCG vaccination (tables, boxes, trays, cabinets, etc.) must be labeled. Vaccination in the maternity hospital is carried out in the morning.
In connection with early discharge from obstetric hospitals, in the absence of contraindications, vaccination of newborns against tuberculosis can be carried out from the third day of life; discharge is possible an hour after vaccination if there is no reaction to it. Monitoring of vaccinated and revaccinated children, adolescents and adults is carried out by doctors and nurses of the general medical network. 1 - 12 months after vaccination, they should check the vaccination reaction, recording the size and nature of the local reaction (papule, pustule with crust formation, with or without discharge, scar, pigmentation, etc.).
These details must be recorded:
- for children and adolescents attending children's institutions in registration forms No. 063/u (child's card in the clinic) and No. 026/u (child's card in the kindergarten or school); - for unorganized children - in registration form No. 063/u and in the history of the child’s development (form No. 112).
Organization of vaccination of newborns.
The chief physician of the maternity hospital (head of the department) organizes vaccination of newborns. The chief physician of the maternity hospital (department) allocates at least two nurses to undergo special training in the technique of administering the vaccine.
When sending an exchange card (registration form No. 0113/u) to the children's clinic, the maternity hospital (department) notes on it the date of intradermal vaccination, the series of the vaccine, its expiration date and the name of the manufacturing institute.
The maternity hospital (department) informs parents that 4–6 weeks after intradermal vaccination, the child should develop a local vaccination reaction, upon the appearance of which the child must be shown to the local pediatrician. It is strictly forbidden to treat the reaction site with any solutions or lubricate it with various ointments.
Children born outside the maternity hospital, as well as newborns who for some reason were not vaccinated, are vaccinated in a children's clinic (in the children's department of a hospital, at a medical and obstetric station) by a nurse (paramedic) specially trained in the intradermal vaccination technique. To vaccinate newborns using the intradermal method in the children's room of the maternity hospital (ward), you must have:
— Refrigerator for storing BCG and BCG-M vaccines at a temperature not exceeding +8° C. — 2–5 gram disposable syringes for diluting the vaccine — 2–3 pcs. — Disposable tuberculin syringes with a well-fitting piston and a thin short needle with a short oblique cut — at least 10–15 pcs. for one day of work. — Injection needles No. 840 for diluting the vaccine — 2–3 pcs. — Ethyl alcohol (70%) registration No. 74\614\11(12). — Chloramine (5%). registration number 67\554\250. Prepared on the day of vaccination.
All items necessary for intradermal vaccination should be stored under lock and key in a separate locker. Their use for any other purposes is strictly prohibited.
When vaccinating children who were not vaccinated during the neonatal period, the clinic must additionally have instruments for checking the Mantoux tuberculin test.
“FOR WHITES ONLY?”
When researching the effectiveness of the BCG vaccination, a strange feature was discovered: it “works” effectively only in countries with a temperate climate. Thus, clinical studies conducted in the UK have proven a protective effect of 60% to 80%. But the further south you go, the worse it is, and in countries with an equatorial climate, the effectiveness of BCG turned out to be quite insignificant.
In global statistics, infectious diseases are still the leading cause of death. But in countries with developed healthcare, the average person has already forgotten about the destructive epidemics of the past, and only specialists and lovers of the classics are aware of the horrors of smallpox, cholera or tetanus.
Just a hundred years ago, most children did not live to adulthood, dying from infectious diseases, and only extensive reproduction saved humanity from extinction. Today, in the Russian mortality structure, 1.6% of people die from infections.
While diseases of the cardiovascular system claim the lives of 57% of Russians (according to Rosstat for 2010). Overall life expectancy has increased significantly over the past hundred years, so that in developed countries most people die of “old age” (i.e. cancer, heart attacks and strokes). To what do we owe such happiness? Where did the old epidemics go?
Two women speaking through flu masks during an epidemic, 1918 © Keystone/Getty Images
Sanitary and hygienic measures played a significant role. The incidence of many fecal-oral infections (cholera, typhoid fever, etc.) was minimized when the population began to be supplied with chlorinated water. Outbreaks of the same cholera occur from time to time today, affecting up to 5 million people and killing up to 100 thousand annually, but today this problem concerns almost exclusively 3rd world countries (in 2010, large outbreaks were noted in Nigeria, Chad, Cameroon and Haiti). Only fiction and film classics remind us of past cholera epidemics in Europe (for example, “Death in Venice” by Luchino Visconti).
Antibiotics, which began to be widely used since the 40s of the last century, also played a huge role in the fight against bacterial infections. Wonderful drugs have appeared on the pharmaceutical market that can cure not only bacterial, but also some viral infections, such as viral hepatitis. We will not belittle the importance of condoms in controlling the spread of sexually transmitted diseases.
However, assessing the epidemiological retrospective, we come to the conclusion that vaccines played the greatest role in the fight against dangerous infections. Of course, it is still possible to find an American today with legs paralyzed due to polio, but since the mid-1990s, this disease has no longer been recorded in the Western Hemisphere. There is no longer any smallpox in the world (the last case was registered in Somalia in 1977), but until recently this infection was a planetary disaster.
In the 18th century in Russia, every 7th child died from smallpox, and in the 20th century the virus claimed the lives of almost half a billion people! It was smallpox, as well as other infections brought to South and Central America, that destroyed indigenous civilizations.
Preventive vaccination against cholera in 1966.
The word “vaccine” itself comes from the Latin name for cow (vacca). In 1796, Edward Jenner first used an effective method of preventing smallpox - he inoculated his own son with cowpox, which is non-lethal to humans. Many years before, in the East they began to use rubbing smallpox scabs from people who had had a mild form of smallpox, then the practice of such vaccinations spread to Europe. This is how Jenner himself was vaccinated in childhood. Unfortunately, human smallpox vaccinations were very dangerous and about 2% of children did not survive them. However, smallpox epidemics at that time were so devastating that people preferred such vaccinations as there was less risk. Jenner's ingenious discovery was a successful attempt to inoculate not human, but closely related cowpox. The discovery did not immediately gain fame. Jenner was ridiculed at the Royal Society of London, where he sent his work for evaluation, and was hostile to the idea of inoculating people with cow disease and the clergy. And yet, having gone through a thorny path, vaccination spread throughout Europe during Jenner’s lifetime, and the scientist died in 1823 at the zenith of his fame.
Even during Jenner’s lifetime, vaccination began to acquire the most bizarre myths. Over time, myths changed and new ones replaced outdated ones. However, despite all the resistance to vaccines, smallpox was eradicated by vaccinating almost the entire population of the planet, from civilized Western countries to the illiterate and superstitious natives of Africa. As frightening as the myths about vaccinations sounded, smallpox, which claimed so many lives, was much worse.
British artist James Gillray in 1802 caricatured the vaccination scene at St. Pancras Hospital. Here Edward Jenner vaccinates frightened girls, while cows jump out of those already vaccinated. At that time, there was a myth that cowpox vaccination could cause the growth of appendages on the body that resembled the body parts of a cow. The boy next to Jenner holds a tub on which is written “Fresh Cow Pocks,” and in his pocket he has a newspaper with the article “Benefits of Vaccine.” The picture at the top of the cartoon depicts the popular biblical scene of the worship of the golden calf.
We began to forget about terrible epidemics largely thanks to vaccination, and as vaccinology developed, vaccinations became increasingly safer. For vaccination, weakened pathogens are used, and in recent decades, killed bacteria and viruses or even their purified antigens, which are not capable of causing even the mildest form of infection in the vaccinated person, are increasingly used. However, today new myths about vaccines are increasingly emerging and “anti-vaccination” theories are gaining popularity.
WHO GENERATES MYTHS ABOUT VACCINATIONS?
First of all, individuals involved in health care itself or in related fields are involved in this process. As in any profession, in the medical environment there are competent and not so competent specialists. At the same time, an illiterate physician can give rise to a very harmful myth. Of course, among the most ardent anti-vaxxers, psychopathic individuals predominate, but they are the ones who prefer to be invited to popular talk shows, and it is their illiterate opuses that are willingly published in the press. In their pseudoscientific reasoning, they are able to outshout any intelligent scientist. The horror stories they come up with find an invariable response in the hearts of parents, whose concern for newborns normally reaches an almost paranoid level.
Oddly enough, many myths are supported by the vaccine manufacturers themselves. Vaccines are a very lucrative business and the competition is aggressive. As soon as another myth appears about the mortal danger of one of the components of the vaccine, for example, a preservative, one of the manufacturers immediately replaces this component with an analogue, or finds a way to produce the vaccine without preservatives at all. Moreover, the absence of this component, which is actually completely safe, is used by the manufacturer as a powerful advertising ploy. The average person, hearing that this vaccine is better than all others because it does not contain such and such a preservative, naturally concludes that this component is dangerous to health. Immediately, retrospective analyzes of the health of those vaccinated with old vaccines with the ill-fated preservative begin, and, of course, there are many “victims”...
After scientists started talking about the neurotoxic effect of aluminum, all utensils made from this metal were removed from public catering. “Anti-vaxxers” immediately jumped on vaccine adjuvants. Such adjuvants are presented in a number of vaccines in tiny and completely safe dosages in the form of aluminum alum, which many drink by the spoonful to combat heartburn. You can still find popular aluminum-containing antacids on the shelves of pharmacies. However, many vaccine manufacturers have tried to avoid using aluminum-containing adjuvants, again following myths.
Anti-Vaccination rally in Santa Monica, July 3, 2015 © Kent Nishimura / Los Angeles Times
Several years ago, I encountered a large-scale anti-vaccine protest in Moscow. Leaflets were posted everywhere, convincing passersby of the dangers of the hepatitis B vaccine. The authors of these opuses presented incoherent horror stories based on the fact that this recombinant vaccine is produced from baker's yeast through genetic engineering. “How can this be!” they were indignant: “Scientists want to change our genes!” Nonsense, of course, but many fellow citizens were very scared and refused vaccinations...
About 6 years ago I had the opportunity to give a lecture on tick-borne encephalitis at one of the large enterprises in Siberia. When the topic of vaccination came up, one of the listeners was indignant and told the audience an amazing story. According to her, one of her closest friends gave birth to a child with severe brain underdevelopment due to the fact that shortly before conception her husband was vaccinated against tick-borne encephalitis. It would seem that the whole story is nonsense. But the audience reacted sympathetically to the story. As a result, almost everyone in this group refused vaccination. The more fanciful and categorical a medical horror story, the more followers it has. However, real facts indicate that the vaccines used in medicine today are among the safest drugs, and serious complications after vaccinations are so rare that in most cases it is not possible to prove a cause-and-effect relationship between the vaccine and the disease that occurred at the same time.
Let me give you some numbers:
The childhood measles, rubella, and mumps combination vaccine causes serious complications in 1 in 1,000,000 frail children. At the same time, the measles disease itself can cause the most serious consequences: pneumonia in 6 out of 100 patients, encephalitis in 1 out of 1000, death in 2 out of 1000 children. Rubella causes severe malformations in newborns in every fourth pregnancy complicated by this infection in the first trimester. Mumps (mumps) causes up to 1/4 of all cases of male infertility.
Diphtheria causes death in 1 in 20 cases, tetanus in 2 in 10. Whooping cough kills one in 1,500 children and causes pneumonia in 1 in 8, and encephalitis in 1 in 20. What about the combined vaccine against diphtheria, tetanus and whooping cough ( DPT), not a single case of a fatal complication has been proven, acute encephalopathy is observed in the USA in 0-10.5 cases out of 1,000,000, convulsive and anaphylactic reactions followed by complete recovery are recorded in 1 out of 14,000 cases. To keep the number of severe adverse reactions to an absolute minimum, vaccines are now increasingly using an acellular pertussis component.
The live polio vaccine (oral drops) raises many questions. It is indeed capable of causing vaccine-associated polio in immunodeficient and genetically predisposed children. And although the incidence of such complications is very low (in general, 1 case per 2,500,000 vaccinations), in developed countries pediatricians have switched to an inactivated (killed) vaccine in the form of injections, which does not cause such complications.
How does healing proceed in newborns: stages of scar healing
In newborn babies, approximately 4-6 weeks after the vaccine is administered, a small spot is noticeable. Soon it becomes indurated, like a mosquito bite.
It reaches approximately 5-10 millimeters in diameter.
This papule is characterized by a color change to white, red, purple or bluish.
At the next stage, instead of a spot slightly raised above the surface of the skin, a pustule appears, inside of which there is liquid. Initially it is transparent, but over time it becomes cloudy.
Approximately 4-6 months after the injection (this period is individual for each child), the bubble bursts, and in its place a crust forms, which can change several times. Under no circumstances should you peel it off until it has completely healed. Otherwise, this process will drag on for a long time. At this stage, the vaccination site must be protected from water.
After six months, the scab falls off naturally in most babies. Instead, a scar remains, reaching 4-6 millimeters in diameter. It initially has a reddish tint, but later turns pale pink. The baby's scar is finally formed by the age of one year.
EPIDEMICS ARE BACK
The history of vaccine prevention inexorably shows that any interruptions in vaccination of the population against epidemic diseases immediately lead to outbreaks and deaths. Therefore, I do not entirely understand the logic of people calling for a complete refusal of vaccinations.
Let us recall, for example, the recent polio epidemic in Tajikistan, which broke out last spring (wrote here). Flaccid paralysis was diagnosed in 430 Tajik children, and panic reached even Russia. Since paralysis occurs in less than 1% of those infected, it is easy to estimate that up to half a million children were infected. In total, 1 million children at a vulnerable age live in Tajikistan. What does all this mean? Just one thing: the supply of vaccinations to the population in the country is suffering. And this is on the border with Afghanistan, which is unaffected by polio!..
REACTIONS AND COMPLICATIONS DURING VACCINATION
In practice, most post-vaccination reactions are individual in nature and cannot be predicted. Most often, quite predictable mild reactions are observed at the injection site, expressed in swelling and redness of the shoulder and an increase in body temperature to subfebrile levels. Many of these reactions are caused by aseptic inflammation, often due to injection of the vaccine into the subcutaneous fat (especially when vaccinating obese individuals with a short needle). Such reactions go away on their own in a couple of days, and if you take paracetamol, then even faster. Sometimes there is an increase in regional lymph nodes - and this is also a normal reaction to the vaccine.
© ROBIN UTRECHT/AFP/Getty Images
The second most common reaction to vaccination is fainting. Often, from the very sight of the syringe or a few minutes after the injection, vaccine recipients lose consciousness, which is often accompanied by convulsions and vomiting. This reaction is of the same nature as fainting at the sight of blood. It is not related to the vaccine as such, but for an outsider, as well as for the person being vaccinated, such a reaction is very unpleasant. True allergic reactions to vaccine components are relatively rare, but after vaccination the patient should be monitored for an hour in order to react in time to possible anaphylaxis. Before receiving the vaccine, the patient must be asked about his allergies to the components of the vaccine (chicken protein in the influenza vaccine, baker's yeast in the hepatitis B vaccine, etc.).
It should be noted that the presence of contraindications does not mean that the vaccine recipient will inevitably experience a complication. However, contraindications protect the medical worker from possible legal consequences... A clever lawyer can prove to a judge, far from practical medicine, the connection between vaccination and a complication of pregnancy or the birth of a defective child. Therefore, pregnant women are not vaccinated against rubella, mumps, measles, chickenpox and BCG. But non-live anti-influenza vaccines began to be strongly recommended for pregnant women after the swine flu pandemic...
What should a BCG vaccination look like?
In the absence of contraindications, the first BCG vaccination is given to the baby on days 3-5 from the moment of birth, and again when he reaches the age of seven.
The injection site is the outer side of the left shoulder, namely, the border between the upper and middle third. If vaccination is successful, immediately after the injection a papule with a diameter of 5 mm to 1 cm forms on the surface of the skin. After approximately 15-20 minutes, it completely resolves.
A month after this manipulation, the child’s body begins to respond to the injection. A pustule with purulent contents appears at the injection site. Parents of the baby should not worry, since such a reaction is absolutely normal.
There is no need to treat the pimple that appears with ointments and medications.