Article for the “bio/mol/text” competition: Despite the rapid development of medicine, tuberculosis is in no hurry to lose its position, remaining not only relevant and deadly, but also a difficult to diagnose disease. But timely diagnosis is an opportunity to reduce the number of patients with active forms and influence the spread of infection! Traditionally, the Mantoux 2 TE test is used to diagnose tuberculosis. However, in recent years, alternative methods have appeared - Diaskintest and the IGRA (Interferon Gamma Release Assay) blood test. What kind of tests are these and are they able to completely replace the “old lady” Mantoux test, which recently turned 110 years old?
Competition "bio/mol/text"-2018
This work was published in the “Biopharmaceutics” category of the “bio/mol/text” competition 2018.
The nomination partner is medical.
The general sponsor of the competition is: the largest supplier of equipment, reagents and consumables for biological research and production.
The audience award was sponsored by the medical genetics center Genotek.
"Book" sponsor of the competition - "Alpina Non-Fiction"
The problem of treatment and diagnosis of tuberculosis still remains extremely relevant. And it’s not just that Koch’s bacillus (Mycobacterium tuberculosis) develops amazing resistance to antibiotics: the situation is also complicated by the long incubation period of the disease. In fact, we are dealing with a pathogen whose carriers can be completely healthy for a long time! In addition, there are not only active forms of tuberculosis, but also latent carriage. And it is extremely difficult to predict whether it will go into an active form and when it will happen. However, not everything is so bad, because even latent carriage can be diagnosed and, if necessary, treated. The only question is that an accurate and effective method for diagnosing tuberculosis processes has not yet been developed. Therefore, for many years, scientists have been trying to develop an “ideal” test that would distinguish tuberculosis from post-vaccination immunity and latent carriage, would have a low cost and would not depend on the human factor.
However, a diagnosis is not yet a diagnosis, and the result of any test is not the ultimate truth. The diagnosis is still made based on several components:
- clinical picture;
- having contact with a tuberculosis patient;
- X-ray of the lungs, fluorography or computed tomography;
- results of diagnostic tests.
However, most of these methods diagnose tuberculosis after the fact - only screening tests help identify individuals at high risk of developing the disease or with an incipient process. And for more than 100 years, the main method of mass diagnosis of tuberculosis has been the Mantoux 2 TE tuberculin test (containing 2 tuberculin units). The test is controversial, with many false positive results, but it is the one that is used all over the world and there are no plans to abandon it yet.
Mantoux test
The Mantoux 2 TE test is a specific skin test based on tuberculin. Tuberculin is a mixture of various antigens obtained from inactivated Mycobacterium tuberculosis and its metabolic products (proteins, polysaccharides, nucleic acids - about 200 items in total [1], [2]). The preparation for the Mantoux test also contains phenol as a preservative, Tween-80 stabilizer, salts of phosphate buffer solution and sodium chloride.
The meaning of this test is that the human body infected with Mycobacterium tuberculosis will respond to the introduction of its particles by producing T-lymphocytes [3]. If a person is healthy, such a reaction will not occur. However, there is one thing: the antigens that make up tuberculin are characteristic not only of Koch’s bacillus, but also of other strains of mycobacteria, including M. bovis - the basis for the BCG vaccination. Therefore, the Mantoux test does not “distinguish” well between those vaccinated with this vaccine and those actually sick with tuberculosis.
Three types of tuberculin are used in the world (Fig. 1): the Danish drug PPD (purified protein derivative) RT 23 , the American PPD-S and the Russian one - PPD-L . They differ in the types of mycobacteria from which they were obtained: in the production of Danish and American drugs, only M. tuberculosis is used, and in the production of Russian drugs, a mixture of M. tuberculosis and M. bovis (mycobacterium that causes tuberculosis in cattle; based on this strain The BCG vaccine was developed. The difference in the composition of tuberculin determines different limits for a positive result: 15 mm for children vaccinated with BCG, and no more than 10 mm for unvaccinated children under 5 years of age for the Danish drug, no more than 10 mm for the American and 5 mm for the Russian [4].
Figure 1. Tuberculin preparations
Nationwide shortage of tuberculin skin test antigens
Diagnosis using the Mantoux test is carried out as follows: a small amount of tuberculin is injected under the skin just above the wrist and after 72 hours the reaction is assessed, which is considered positive if a swelling (papule) more than 5 mm in diameter appears at the injection site.
Depending on its size, the degree of reaction is distinguished from negative (0–1 mm) to pronounced, or hyperergic (17 mm or more in children and adolescents, 21 mm or more in adults) [5]. And here the difficulties begin, because those vaccinated with BCG have a positive Mantoux reaction [6]! Moreover, the larger the post-vaccination scar, the higher the sensitivity to tuberculin [7]. Therefore, in BCG vaccinated people, not only the diameter of the papule is assessed, but also the size of the post-vaccination scar (Table 1). Table 1. Ratio of papule and scar size after BCG vaccination. [8]
| Time elapsed since BCG vaccination | Scar size after BCG | Vaccinated immunity (mm) | Unclear reason | Suspicion of infection |
| 1 year | 6–10 mm | 5–15 mm | 16 mm | More than 17 mm |
| 2–5 mm | 5–11 mm | 12–15 mm | More than 16 mm | |
| 0 mm | 2–4 mm | 5–11 mm | More than 12 mm | |
| 2 years | Regardless of size | Reduction in the size of the papule or its previous size | Increase in size by 2–5 mm from the previous positive result | The reaction changes to positive or the papule increases by more than 5 mm |
| 3–5 years | Regardless of size | 5–8 mm or reduction in papule size | Increase in size by 2–5 mm over the past year or no tendency to decrease | Change to a positive (5 mm) reaction or increase in papule by 6 mm; 12 mm for the first test; change from the previous size by 2–4 mm or a size of 12 mm |
| 6–7 years | Regardless of size | 0–4 mm | 5 mm | 6 mm or more |
| 7–9 years | If the child was revaccinated with BCG at the age of 7, the Mantoux test becomes positive again and the norms are repeated. | 0–4 mm | 5 mm | 6 mm or more |
| Adults | Negative reaction, redness of any diameter; papule up to 4 mm | More than 5 mm |
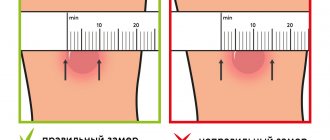
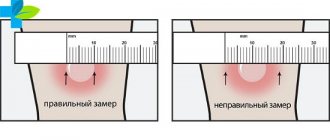
Of course, the method of assessing the result is quite subjective. But most importantly, the papule must be measured correctly, recording only the size of the convex part and ignoring the redness around it (Fig. 2).
Figure 2. Correct and incorrect estimates of papule diameter
“Should I worry if the size of the mantu is 10 mm”
However, this is not the main disadvantage of the Mantoux test: the problem is that with its help it is difficult to distinguish post-vaccination immunity from the disease, and the cost of an error is an “unnecessary” course of antibiotics. Therefore, most often the result is only the first step, only a suspicion of tuberculosis. Interestingly, in severe cases of the disease, due to an inadequate T-cell response, there is usually no reaction to tuberculin [6], however, this phase of the disease is already clearly visible both in the clinical picture and on the radiograph.
Another difficulty with the diagnostic capabilities of the Mantoux test is that they depend on the lower limit of a positive result: the lower the limit, the more false positive reactions will be observed. For example, in Russia the threshold value is a papule of 5 mm. This leads to overdiagnosis—a large number of recorded reactions, but ultimately to a low percentage of actually detected cases of infection [4].
In general, it is not surprising that recently the informativeness of the tuberculin test has been constantly questioned. Moreover, it can cause allergic reactions not related to tuberculosis, so more and more healthy, but allergy-prone children are forced to go to a tuberculosis clinic in the hope of finding out the reason for the positive reaction. Finally, many factors can influence the test result: recent infections, chronic diseases, medications, changes in hormonal levels, or immunity to non-tuberculous mycobacteria [7].
If we talk about the advantages of the Mantoux test, then in addition to low cost, they will be the ability to detect tuberculosis in the early stages of development (except for persons with immunosuppression and young children under two years of age [7]) and a higher diagnostic value in those unvaccinated with BCG compared to vaccinated ( from 50% and below versus 65.4% [6], [9]).
Myths about the Mantoux test
- Tuberculin is harmful to health because inactivated mycobacteria cause allergies and “load the immune system . There is a small grain of truth here: as a drug, tuberculin can cause allergic reactions not associated with infection, but there can be no talk of any “load”, if only because antibodies are not produced against it.
- The Mantoux 2 TE test is toxic because the drug contains phenol . In the tuberculin test, phenol is a preservative that inhibits the growth of bacteria and fungi [5]. Moreover, its amount is so small (0.00025 g) that it cannot have any effect on health. Phenol is a metabolic product of bacteria that inhabit our intestines, so it is formed in the tissues of the body, enters the blood and is excreted in the urine. Approximately 0.1–0.15 g of phenol is excreted daily, which is many times greater than the amount contained in the preparation for the Mantoux test.
- The Mantoux test is done only in third world countries. This is not true: the tuberculin test is done all over the world, including the USA, Canada, Germany, Denmark and the Netherlands. However, due to the low incidence in these countries, tuberculin testing is usually carried out only in risk groups.
How long does it take to check the reaction?
The reaction to the administered tuberculin is checked no earlier than 72 hours from the test. Neither sooner nor later does it make sense to take measurements of papules or redness - the data will be distorted, which will entail the need for revaccination or an extensive examination by a phthisiatrician.
We recommend reading about why Mantoux is placed before BCG. From the article you will learn how many days after BCG is given after Mantoux, when the vaccination cannot be done, and whether Mantoux can be done without BCG. And here is more information about whether it is necessary to make Mantoux.
Mantoux is given to children of preschool and school age with a certain frequency. A clear schedule minimizes the risks of obtaining distorted results and developing side effects. Typically, the test is performed once a year, but at the discretion of the doctor, the frequency can be increased.
"Diaskintest"
Science, however, does not stand still, and alternatives to the Mantoux test exist. The only question is how alternative they are. After decoding the genome of M. tuberculosis in 1998, it became possible to develop completely new tests: the domestic skin test “Diaskintest” and IGRA blood tests. However, Diaskintest is the one that most claims to be a substitute test for the Mantoux test.
Compared to the tuberculin test, Diaskintest is a big step forward. And all because it does not contain hundreds of antigens, but only the recombinant protein CFP10-ESAT6 in a standard dilution, which does not react either to the vaccine strain of M. bovis or to most non-pathogenic mycobacteria - it is mainly sensitive only to Koch’s bacillus . In other words, only this protein can be used to diagnose an infection, which indicates the presence or absence of cellular immunity to M. tuberculosis. Diaskintest is administered intradermally and the result is checked after 72 hours.
Figure 3. ESAT-6 and CFP-10 antigens
"Tuberculosis: the causative agent"
In the M. tuberculosis genome, the ESAT-6 and CFP-10 proteins are encoded in the RD1 region. They are expressed during the reproduction of mycobacteria and are associated with its virulence; therefore, the immune response to these proteins reflects the activity of the infectious process [10]. As part of Diaskintest, they are presented in the form of a recombinant protein from two related antigens ESAT6 and CFP10 (Fig. 3), synthesized by a genetically modified bacterial culture Escherichia coli BL21(DE3)/pCFP-ESAT [6]. Using a similar technology, another drug was obtained - Danish C-Tb , but it has a different ratio of ESAT-6 and CFP-10, and it is less sensitive compared to the Russian development [4].
Due to the fact that Diaskintest does not contain a cocktail of polysaccharides, lipids and proteins, but only a synthetic antigen plus excipients (phenol, sodium chloride, Tween-80), it is more highly specific than the preparation for the Mantoux test. That is, with its use, fewer false-positive results are recorded, as well as allergic reactions of a non-infectious nature [2].
As for assessing the activity of the tuberculosis process, in this “Diaskintest” is head and shoulders above its competitors, because a gradation of positive results has been developed for it (Table 2).
That is, the more pathogen in the body, the larger the size of the papule. This means that in the majority of tuberculosis patients the reaction to this test is more pronounced than in latent carriers (the only thing is that here again there is a subjective assessment of the result). Let's add to this the fact that Diaskintest allows us to identify carriers with a high risk of developing tuberculosis and reduce the amount of unnecessary therapy [11], as well as reducing the severity of the reaction to it in patients receiving a course of antibiotics [4], and we will get a very valuable competitive advantage over tuberculin test. Table 2. Assessment of response to Diaskintest. Compiled based on information from the instructions.
| Reaction | Size of hyperemia and papules |
| Negative | No papule and/or hyperemia, “prickly reaction” up to 2 mm |
| Doubtful | The presence of hyperemia in the absence of a papule |
| Positive: | Papule of any size: |
| - mild positive reaction | Up to 5 mm |
| - moderate reaction | 5–9 mm |
| - pronounced reaction | 10–14 mm |
| - hyperergic reaction | 15 mm or more, as well as with vesicular-necrotic changes and (or) lymphangitis, lymphadenitis, regardless of the size of the infiltrate |
However, Diaskintest also has disadvantages:
- It is not sensitive to M. bovis and, therefore, cannot diagnose the tuberculous process caused by this type of mycobacterium. Of course, the number of such cases is small, but it still reduces the effectiveness of the test.
- According to studies, Diaskintest has a fairly high sensitivity in detecting tuberculosis infection both in children - 90-96.7%, and in adults - 78-81.5% [2]. However, there remain approximately 10–20% of cases that it misses.
- Diaskintest can be negative in tuberculosis patients with severe impairments of the immune system due to severe disease, as well as in HIV-infected patients (in this case, the sensitivity of the test depends on the level of CD4+ T-lymphocytes [2]).
What you need to know about skin testing?
- The preparation for the Mantoux 2 TE test and Diaskintest are markers of tuberculosis allergy, that is, they are “allergens”. Tuberculosis allergy is associated with an immune response to M. tuberculosis, which makes the body sensitive (sensitized) to even small amounts of mycobacterium. Using skin tests containing an irritating factor (inactivated particles of Koch's bacillus), this process can be recorded. Infectious allergy is a delayed reaction, so the test result is not assessed immediately, but after 72 hours.
- The skin reaction to these tests is a marker of a T-dependent immune response, which involves CD4+ and CD8+ T cells and associated proinflammatory cytokines, IFNγ, TNF, etc. Therefore, skin tests are also sensitive to latent carriage, when the amount of mycobacteria is extremely small [4], [6].
- As can be seen from tables 1 and 2, the results of skin tests are observed over time, if necessary, comparing the values of previous years. Therefore, there is no point in doing a tuberculosis diagnosis, as they say “for show”: only for a medical card for kindergarten or school - it must be done annually (or at least once every two years).
- In the interpretation of the results of skin tests, there is the concept of a turn - a sharp increase in the diameter of the papule by six or more millimeters compared to the previous test. In addition, the transition of a negative reaction to a positive one, not related to BCG vaccination, is considered a turn. A Mantoux test does not always mean infection (it can also be of an allergic nature), however, to clarify the situation, an additional examination and consultation with a phthisiatrician is usually prescribed.
How often do preschoolers make Mantoux, how many times a year?
Mantu is given to preschool children once a year. The first vaccination against tuberculosis is given in the maternity hospital on the 3-5th day of the baby’s life (depending on the general condition of the newborn, complications during childbirth and other indicators).
The Mantoux test is performed no earlier than 12-13 months after BCG, and it is rarely perceived by doctors as informative - the antibodies produced as an immune response to the vaccine are still active in the child’s body.
Subsequent tests are carried out every year - in the 2nd, 3rd and so on.
What to choose: Mantoux test or Diaskintest?
If we compare the diagnostic effectiveness of tests, then “Diaskintest” gives a significant head start to the tuberculin test. Nevertheless, among phthisiatricians there are adherents of both the Mantoux test and Diaskintest. However, comparative studies do not speak in favor of tests with tuberculin - after all, a reaction to them does not mean illness or infection with mycobacteria. Plus, mass BCG vaccination sharply reduces their diagnostic abilities [6].
An example is a domestic study that compared the results of skin tests [6].
It turned out that in adolescents who lived in close contact with patients with an open form of tuberculosis (bacterial excretors), positive reactions to the administration of tuberculin were observed in 77.9% of cases, while the disease was detected only in 4.9%. At the same time, positive reactions to Diaskintest were noted in only 5.6%, of which tuberculosis was detected in 62.5% of cases [6]. According to Russian scientists, the effectiveness of Diaskintest in detecting active tuberculosis can exceed the effectiveness of the Mantoux 2 TE test by 40 times (Table 3) [11]! Table 3. Comparison of the results of Diaskintest and the Mantoux test in different situations. [9]
| Mantoux test result | Diaskintest result | |
| Fine: | ||
| in those unvaccinated with BCG | Negative | Negative |
| in those vaccinated with BCG | Weakly positive or positive without hyperergy | Negative |
| If infected: | ||
| in those unvaccinated with BCG | Positive | Weak or positive depending on the activity of the process* |
| in those vaccinated with BCG | Strongly positive | Weak or positive depending on the activity of the process* |
| * The situation (10–20% of cases) when the Diaskintest result is false negative is not taken into account. | ||
How often is Mantoux given to adults, and up to what age is it done?
Mantoux is not often given to adults, but only according to indications:
- the doctor has good reason to suspect the patient has extrapulmonary tuberculosis;
- the patient has recently undergone radiotherapy, radiography or any other radiation exposure;
- a person undergoes long-term treatment with certain medications (glucocorticosteroids, immunosuppressants).
After the age of 16-18 years, the Mantoux test is done extremely rarely, unless there are clear indications for it. After reaching the age of 35, such manipulation is performed only at the request of doctors.
Most often, Mantoux is given to those adults who are at risk - they are in constant contact with patients, live in a region that is unfavorable specifically for the incidence of tuberculosis, work in correctional colonies, and so on.
Due to age-related changes in the human body, the Mantoux test is considered to be of little information; it is advisable to rely on fluorography data in diagnosis.
Blood tests for tuberculosis: pros and cons
The discovery of M. tuberculosis-specific antigens allowed the development of laboratory tests for the diagnosis of tuberculosis. These are the well-known IGRAs (Interferon-Gamma Release Assays), which include T-SPOT®.TB and QuantiFERON-TB Gold In-Tub (“Quantiferon”).
The technology for carrying them out is quite simple: venous blood is taken from the patient, mixed with the proteins ESAT-6, CFP-10 and TB 7.7, and then the reaction is observed. That is, the number of T-lymphocytes (T-SPOT®.TB) or gamma interferon (“Quantiferon”) [12].
Many unreasonably consider these tests to be the “gold standard” for diagnosing tuberculosis and its latent forms, although their results can only indirectly indicate active infection with mycobacteria or carriage - processes that IGRA analyzes do not distinguish [12]. And if we rely on the guidelines of the WHO, as well as the European Center for Disease Control and Prevention (ECDC), there are no “gold standards” in diagnosing latent forms of tuberculosis. Just as there is no adequate model of latent tuberculosis infection. Therefore, to assess the limits of the results of IGRA tests, it is necessary to use so-called “surrogates” - testimonies of people with confirmed active tuberculosis [12]. And this only complicates the situation, because patients with tuberculosis have reduced cellular immunity, and their indicators cannot serve as a basis for assessing the diagnosis of latent infection [6].
In addition, a negative IGRA blood test result does not guarantee the absence of the disease; They are also not immune to false results. For example, when testing with Quantiferon, false negative results are possible:
- in the early stages of infection;
- in immunodeficiency conditions;
- due to improper blood collection or transportation;
- due to errors during decoding of results.
I will add that IGRA tests require high-quality equipment, special reagents and qualified personnel, so their cost is quite high.
In addition, compared to skin tests, a significant disadvantage of these tests is the in vitro determination of only interferon-gamma production or T-cell activity. Therefore, in countries with high incidence (and Russia is undoubtedly one of them, with an indicator of more than 50 patients per 100,000 population [13]), IGRA analyzes do not have any additional advantages [12]. Moreover, their ability to diagnose the tuberculosis process ranges from 42–90% for different age groups, and they do not mark latent carriage [12]. In other words, for residents of our country, blood tests for tuberculosis are generally a waste of money, although in countries with low incidence (USA, Canada, Western Europe) they are more informative and are recommended to replace tuberculin tests for those vaccinated with BCG [14].
There are more than half a billion latent carriers of M. tuberculosis living in the world. Moreover, not every one of them ends up getting sick, because the proliferation of mycobacteria is restrained by the immune system. For example, out of 100 children infected with Koch bacillus, only one develops an active form of tuberculosis, so diagnostic tests are aimed not only at identifying latent carriers, but also at assessing the risk of developing the disease [15].
T-spot test for tuberculosis instead of Mantoux in a child
Instead of Mantoux, a T-spot blood test is performed on the child; it is indicated for detecting active and latent tuberculosis infection. It can be the main or auxiliary method, in combination with tuberculin tests it gives the most reliable result.
The analysis is carried out on venous blood and consists of counting T-lymphocytes that have been in contact with Mycobacterium tuberculosis. The main advantages and disadvantages are similar to the quantiferon test.
Scheme of T-spot analysis for tuberculosis
Blood tests vs skin tests: comparison of effectiveness
When assessing the effectiveness of tests for diagnosing tuberculosis, two parameters are most often taken into account: sensitivity and specificity. Sensitivity refers to the ability of a method to identify individuals with the disease or carriers at high risk of developing tuberculosis. Specificity is the ability of the test to correctly identify people who do not have tuberculosis (that is, this parameter characterizes the risk of erroneous false-positive results) [12].
According to studies, IGRA blood tests have a fairly high specificity, but problems with sensitivity (Table 4), so they cannot become the main tool in the diagnosis of tuberculosis, especially in countries with high incidence.
As for Diaskintest, if you believe domestic publications [4], [6], [10], [11], it has both high specificity and high sensitivity (Table 4). A miracle, not a test! However, high sensitivity does not equal absolute sensitivity, which is why “Diaskintest” also experiences “punctures” in the form of false results (most often they are observed in children under two years of age or in persons with concomitant severe diseases [11]). Table 4. Assessment of the sensitivity and specificity of IGRA blood tests in comparison with the Mantoux tuberculin test and Diaskintest in the diagnosis of active tuberculosis
| "Quantiferon" [12] | T-SPOT®.TB [12] | Mantoux test [12] | "Diaskintest" [2] | |
| General sensitivity | 80%* | 81%** | 65%*** | 93,3% |
| General specificity | 79% | 59% | 75% | 93,7% |
| * Overall sensitivity 81% (95% CI 78–84%) for patients with confirmed tuberculosis. ** Overall sensitivity 92% (95% CI 90–93%) for patients with confirmed tuberculosis. *** Overall sensitivity 68% (95% CI 63–72%) for patients with confirmed tuberculosis. CI - confidence interval, confidence interval. | ||||
In general, blood tests are unlikely to be able to completely replace the Mantoux 2 TE test (and especially the Diaskintest if we are talking about the Russian Federation).
But perhaps they can become one of the additional tools in the diagnosis of active tuberculosis infection? Yes, such a possibility exists, but there are caveats here too. For example, for patients with extrapulmonary tuberculosis, HIV-infected people or children over five years of age, they can be considered as an additional method. However, at present there is a limited number of studies on these tests [12], so it is too early to draw far-reaching conclusions (Table 5). Table 5. Assessment of the specificity and sensitivity of IGRA blood tests, the Mantoux test and Diaskintest in children and adolescents in the diagnosis of tuberculosis
| Mantoux test [12] | "Quantiferon" [12] | T-SPOT®.TB [12] | "Diaskintest" | |
| Specificity | 89,4% | 85,8% | 84% | 86,3% [2] |
| Sensitivity | 65,4% | 79,9% | 42,2% | 90,5–96,7% [2] |
| 94,8 [11] |
An alternative to Diaskintest and Mantoux - quantiferon test
As an alternative for skin tests (Diaskintest and Mantoux), quantiferon can be chosen. It is suitable for selecting patients (screening) who need further examination.
To whom is it assigned?
Indications:
- negative Mantoux or Diaskintest in children with HIV infection, diabetes mellitus, malnutrition, blood tumors;
- contraindications to the administration of tuberculin - intolerance, allergies, skin diseases, infections or recent vaccination, epilepsy;
- questionable skin test result;
- the need to distinguish between positive Mantoux after vaccination and due to infection;
- examination of patients of special social groups (they may not come at the right time to assess the Mantoux results) or those who were in contact with patients;
- confirmation of tuberculosis by symptoms (cough, bloody sputum, fever), positive skin tests, changes in the lungs on an x-ray.
Advantages
The Quantiferon test has the following advantages:
- high percentage of reliable results, no false results after BCG vaccination;
- sufficient specificity and sensitivity;
- safe;
- no adverse reactions or contraindications;
- Just one visit to the doctor is enough;
- subjective assessment is excluded (for example, incorrect measurement of the papule).
Methodology for conducting the quantiferon test
Flaws
Even this modern diagnostic method has disadvantages:
- false results in a child under 5 years of age;
- does not show infection with reduced immunity;
- not suitable for detecting early stage tuberculosis;
- it is impossible to distinguish an active disease from a harmless carriage;
- a negative result is not a 100% guarantee of the absence of tuberculosis;
- Errors in blood collection and transportation may affect reliability.
Watch this video about the advantages and disadvantages of the quantiferon test:
Which test should you choose?
As they say, with all the wealth of choice, there are few alternatives. Unfortunately, when choosing a test, many are guided not by its diagnostic characteristics, but by its harmlessness to health, because phenol in skin tests scares many. And there is even a movement against the Mantoux test, whose support group periodically suggests replacing it with IGRA blood tests. But, as noted above, such fears have no basis. In addition, being a waste product of the body, phenol does not accumulate, but is excreted along with urine. Therefore, the main criteria are still the sensitivity and specificity of the tests.
At the moment, only Diaskintest demonstrates the best characteristics. However, despite this, the Mantoux 2 TE test continues to be used in mass diagnostics, and it completely satisfies phthisiatricians. After all, Diaskintest (as well as IGRA tests) does not respond to infection caused by M. bovis. In addition, it was introduced into mass diagnostics only 10 years ago, and this is too short a time to fully verify its diagnostic effectiveness and “write off” the tuberculin test as unnecessary.
As for IGRA blood tests, they are too expensive, do not surpass Diaskintest in sensitivity and do not distinguish between latent carriage. And in a world where there are more than 10 million tuberculosis patients and 1.7 billion carriers of mycobacteria [3], this is a significant drawback.
Literature
- Nesterova Y. (2017). “The 6 most popular tests for tuberculosis: the problem of choice.” MedAboutMe;
- Koretskaya N.M. (2013). Diaskintest: new opportunities in the diagnosis of tuberculosis. "Medicine in Kuzbass." 4, 3–8;
- A disease that refused to give up;
- Slogotskaya L.V., Bogorodskaya E.M., Levi D.T., Seltsovsky P.P. (2017). 10 years of skin test with recombinant tuberculosis allergen (Diaskintest) and 110 years of Mantoux tuberculin test - comparison of effectiveness. “BIOpreparations. Prevention, diagnosis, treatment." 17, 67–77;
- “On improving anti-tuberculosis measures in the Russian Federation.” (2003). Order No. 109 of the Ministry of Health of the Russian Federation;
- Slogotskaya L.V. (2013). Tuberculin diagnostics and new tests to detect infection. "Medical Bulletin". 16, 14–15;
- Filinyuk O.V., Kolokolova O.V., Kabanets N.N. Diagnosis of tuberculosis in children and adolescents. Tomsk: Siberian State Medical University, 2013. - 174 p.;
- Methods for detecting tuberculosis in children (methodological manual). Moscow, 1990;
- Yakovleva G.P. (2017). DIASKINTEST vs MANTU. "Tuberculosis allergy";
- Slogotskaya L.V. (2014). Immunological tests with Mycobacterium tuberculosis-specific proteins ESAT-6 AND CFP-10. "Tuberculosis and lung diseases." 1;
- Slogotskaya L.V., Senchikhina O.Yu., Nikitina G.V., Bogorodskaya E.M. (2015). The effectiveness of a skin test with recombinant tuberculosis allergen in detecting tuberculosis in children and adolescents of Moscow in 2013. “Pediatric Pharmacology.” 12, 99-103;
- ECDC guidance: Use of interferon-gamma release assays in support of TB diagnosis. Stockholm: ECDC, 2011. - 32 p.;
- Nechaeva O.B. (2016). Epidemic situation of tuberculosis in Russia. Central Research Institute of OIZ;
- Testing in BCG-vaccinated persons. (2016). CDC;
- Aksenova V.A. and Levy D.T. (2012). Tuberculosis in children and adolescents. “BIOpreparations. Prevention, diagnosis, treatment." 1, 22–27.