Pros of vaccination
Vaccinations do not prevent a virus or pathogenic bacteria from entering the body of a vaccinated person.
Vaccines protect us from disease in a different way. They train the immune system before it encounters a particular infection. Vaccines contain a kind of miniature disease. You cannot get sick after vaccination, but you can acquire immunity. In response to the introduction of a vaccine, our body produces specific antibodies and immune memory cells, allowing the immune system to effectively fight dangerous microbes when encountering them in the future. This tactic is extremely effective. According to the World Health Organization (WHO), vaccination saves the lives of more than 2 million people every year. When it comes to the flu shot, a 2021 study from the U.S. Centers for Disease Control and Prevention found that the flu vaccine reduces deaths from the flu virus by 52% to 79%. Vaccination also significantly reduces the number of hospitalizations of patients diagnosed with influenza, which means that the disease in vaccinated people is not as severe as in unvaccinated people.
Important! Flu vaccines come in different compositions and vary in effectiveness. The composition of the drugs you are interested in can be found on the official websites of the manufacturing companies. For more information about what types of influenza vaccines are available, read the articles “Flu shots in 2020-2021” and “Flu shots.”
It is a mistake to think of the flu as a mild infection. Sometimes influenza causes very serious complications, including secondary bacterial pneumonia, which requires separate antibiotic therapy, is very severe and is responsible for the deaths of 25% of influenza patients.
H1N1 influenza virus. Photo: PHIL CDC
Flu is especially dangerous for pregnant women, children under 5 years of age, and the elderly. In these categories of citizens, the disease is more often severe. In pregnant women, infection can contribute to stillbirth or premature birth. Therefore, the flu vaccine is recommended for all women planning pregnancy, as well as all unvaccinated pregnant women, starting from the second trimester of pregnancy.
Those at risk for influenza also include:
- cancer patients,
- patients with AIDS and HIV,
- asthmatics,
- diabetics,
- people with chronic lung and heart diseases.
Medical workers, military personnel, schoolchildren and students are more susceptible to influenza infection than others. The first - because they often come into contact with patients, the rest - because they exist in close groups. In addition to the fact that vaccination reduces the risk of getting sick and allows you to avoid the dangerous consequences of the flu, provided that it is widely used (when more than 60-70% of people are vaccinated in society), it protects those who are contraindicated for vaccinations for one reason or another. Because the vaccine reduces the risk of infection, people who should not get a flu shot are at less risk when they are around those who have been vaccinated (Figure 1).
Figure 1. Benefits of influenza vaccination. Statistics in the USA. Source: CDC
Causes of allergies after vaccination
The reason that edema occurs and the injection site swells is the body’s reaction to the introduction of foreign substances. This may be evidence that the immune system has thus reacted to the penetration of viral particles and began to fight them. Therefore, redness of the injection site is not always a pathology, sometimes it is evidence that the vaccine is working correctly.
We recommend reading: Nurofen and ibuprofen - what are the similarities and differences?
Reasons that can provoke the development of local reactions:
- injection of a vaccine that damaged the integrity of the skin (irritation of this place is a peculiar reaction of the body to the invasion);
- development of immunity in response to the introduction of a viral antigen;
- vaccination carried out intramuscularly: when the drug is injected into the gluteal region, there is always a danger of affecting the subcutaneous fatty tissue. For children, it is preferable to carry out this procedure on the front of the thigh, for adults - on the upper third of the shoulder.
The basis for the onset of a skin reaction is:
- reproduction of viral agents that have penetrated the skin;
- allergic manifestations after the injection (the hand may swell, the injection site will have an increased body temperature);
- increased manifestations of bleeding after the procedure.
Allergic reactions may be the fault of the medical workers who performed this procedure:
- the vaccine was stored incorrectly, at a temperature that did not meet the standards specified by the manufacturer;
- the injection was not administered in the manner recommended;
- the employee neglected the rules of asepsis and antiseptics.
Contraindications
Flu vaccines are easily tolerated. Most drugs are based on either parts of destroyed influenza A and B viruses, or their individual antigen proteins that can cause an immune response. So who should not receive influenza vaccines? Contraindications to vaccination can be absolute (permanent), temporary (relative), or age-related.
Absolute contraindications
Among those who should not get the flu vaccine:
- people allergic to egg whites (chicken embryos are used in the production of many influenza vaccines);
- people with severe reactions and complications after receiving previous doses of the vaccine. This is a fairly rare occurrence, however, if there are negative reactions to the first dose of the vaccine, this drug is not recommended for further use.
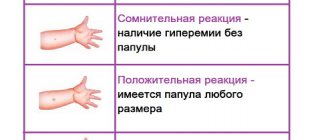
A severe reaction to the vaccine is considered to be a temperature above 40℃, as well as swelling or redness (hyperemia) at the injection site greater than 8 cm in diameter. And post-vaccination complications are, for example, a severe allergic reaction (anaphylactic shock).
However, these contraindications are absolute only in relation to specific drugs. So, if chicken eggs were not used in the production of the vaccine, even allergy sufferers can be vaccinated with it. Sometimes an absolute contraindication can become relative. In many countries around the world, people who are allergic to egg whites are vaccinated against influenza, despite the fact that eggs are used to produce vaccine viruses. The fact is that vaccines used year after year have proven their safety - viral antigens are thoroughly purified before entering the drug, and the likelihood of developing an allergic reaction after vaccination is negligible.
Relative contraindications
Relative contraindications are those whose importance must be assessed by the physician. The decision to vaccinate is made after carefully weighing all the risks that may threaten the patient's health if he receives or does not receive the vaccine. Neglect of some contraindications may be justified if:
- There is an outbreak of influenza in the region,
- the patient is at risk for influenza,
- There is a high risk of complications for the patient in case of influenza.
Among the relative contraindications, first of all, mild acute respiratory viral infections or other diseases in the acute phase, as well as chronic diseases and pregnancy can be noted.
Permanent contraindications
Permanent contraindications are those that accompany a person throughout his life. These include allergies to vaccine components, severe reactions after vaccination, and some chronic diseases and conditions.
Temporary reasons for recusal
Temporary contraindications are exacerbations of chronic diseases or the presence of any acute infections. Since viral antigens that affect the immune system are introduced into the human body during vaccination, doctors do not allow people whose immunity is already fighting another pathogen into the vaccination room.
As soon as a person recovers or has an exacerbation of a chronic disease, the vaccine can be administered (at least 2-4 weeks after recovery). If the patient had a mild form of ARVI or acute intestinal disease, they are sent to the vaccination room immediately after the temperature has stabilized.
Vaccinations are also temporarily contraindicated for children under six months of age and pregnant women in the first trimester. Children after six months and pregnant women in the second and third trimesters must be vaccinated. They are at risk because they are susceptible to the most severe infection. Children are even more vulnerable to the flu virus than adults. In an adult, unlike a child, antigenic imprinting can work: if a person has already had the influenza virus, his body can use the already existing immune memory in response to the attack of the virus and activate protection.
Important! In the case of the live influenza vaccine, pregnancy is an absolute contraindication to vaccination, regardless of the timing. WHO also does not recommend administering live influenza vaccines to pregnant women. The best solution would be an inactivated vaccine or a split vaccine. These medications do not contain merthiolate (a mercury-based compound used as a preservative in some vaccines) and have been shown to be safe.
General contraindications
General contraindications include factors that make vaccination impossible or undesirable for any patient. All of them are listed in the instructions for each specific drug. These are allergies, age up to 6 months, first trimester of pregnancy, strong negative reactions to previous doses of the vaccine.
Particular contraindications
Particular contraindications are established by the doctor after examining and interviewing the patient. These may be chronic diseases aggravated by each other, acute respiratory infection, acute immunodeficiency, underweight (for infants).
Age restrictions
Infants are vaccinated against influenza starting at the age of 6 months, since the mother’s immunity lasts until about six months after the baby’s birth. While the child’s body is protected by maternal antibodies, the effect of the administered vaccine is much lower, and it is not recommended to administer it.
Fact! Children from 6 months to 2 years of age (up to 9 years of age if they are receiving the vaccine for the first time) are recommended to receive 2 doses of influenza vaccine with an interval of 4 weeks, since the second dose increases the effectiveness of immunization for them.
There is no upper age limit for influenza vaccination. Exceptions are cases when the vaccine manufacturer indicates the age limit in the instructions. In any case, you should consult your doctor before vaccination.
Important! There is also a list of false reasons for refusing vaccinations. These include: asthma, dysbiosis, anemia, post-vaccination complications in the family and others. The position of the Russian Ministry of Health in this regard is quite strict: following such contraindications indicates the incompetence of the doctor.
Possible side effects and complications
Like any medicine, flu vaccines have side effects. They are divided into serious and frivolous.
Non-serious reactions after vaccination are minor and considered normal. Thus, the body temperature after immunization may increase, but not by more than 0.5℃, and the throat may turn red. Swelling (no more than 8 cm in diameter) may occur at the injection site. A person may feel like they are starting to get sick. Muscles or headaches may ache, and appetite may decrease. Such adverse post-vaccination reactions occur either immediately in the office when the vaccine is administered, or within the first three days and usually do not require special attention.
The live influenza vaccine can also cause symptoms of ARVI: cough, sore throat, runny nose, nasal congestion, general malaise and loss of appetite. They can last up to 6 days after vaccination. But live vaccines are now rarely used. Doctors give preference to inactivated vaccines, which are easier and faster to tolerate.
The most serious consequence is, of course, anaphylactic shock. It requires immediate resuscitation.
This condition can begin immediately after the start of the vaccine, up to several minutes after its administration, and has clear signs (Fig. 2):
- paleness, cold sweat;
- difficulty breathing, swelling of the throat;
- lethargy, loss of consciousness, in rare cases – convulsions;
- swelling, redness, skin rash.
Figure 2. Signs of anaphylactic shock.
Source: Verywell An allergic reaction to influenza vaccines may be associated with an allergy to egg protein if the drug is based on viruses grown on chicken embryos, although in recent years a number of studies have shown the safety of these vaccines even for allergy sufferers (viral proteins pass through them thorough cleaning). Do not be afraid of vaccines because of the possibility of developing a severe allergic reaction. Almost any product can potentially cause anaphylactic shock in a predisposed person. Finding out the cause and predicting its onset is very difficult, unless the patient knows what exactly he is allergic to. Otherwise, the occurrence of allergies cannot be predicted in advance. Fortunately, allergies and anaphylactic shock in response to vaccines are very rare. Much more often, people are allergic to regular aspirin, antibiotics (especially penicillin) or an anesthetic used by the dentist.
In the medical community, flu vaccination is sometimes associated with Guillain-Barré syndrome. This is a condition where the immune system destroys its own nerves. It is accompanied by weakness, loss of sensitivity, mild paralysis of the arms, legs and facial muscles. But the connection of this syndrome has been proven only with the live influenza vaccine against the H1N1 virus (influenza A virus). But, again, such drugs containing live attenuated influenza viruses are rarely used today. There is no reliable evidence for other vaccines.
What Causes Guillain-Barré Syndrome According to WHO, the cause of Guillain-Barré syndrome can be any infection - bacterial or viral. It can also develop after vaccination or surgery.
It is very important to use vaccines correctly and to store and transport them at low temperatures. Violation of storage and transportation rules can lead to damage to the vaccine, and its administration can lead to undesirable reactions. The effectiveness of spoiled vaccines can be significantly reduced or eliminated. Other errors that can significantly affect the effectiveness of vaccination include:
- violation of antiseptic rules,
- incorrect dose and injection site,
- use of expired vaccine.
These are inevitable in large immunization campaigns but are minimized by careful quality control of all vaccination steps.
Fact! For adults, flu shots are given in the upper arm, and live vaccines are administered as a spray into the nose. Doctors vaccinate children in the thigh. The fact is that if there is a reaction to the vaccine, it is easier for the doctor to apply a tourniquet specifically to the child’s thigh.
Finally, a person can provoke a post-vaccination reaction himself. He may forget about his chronic illness or allergies and not tell the doctor about them before vaccination. In this case, responsibility for the health consequences falls on the patient. Reactions to the vaccine may also have psychosomatic causes. Sometimes a person is so afraid of either the vaccination procedure itself or the negative consequences after it that his health begins to deteriorate. This emotional reaction may include fainting, dizziness, and vomiting.
What to do before and after vaccination
There are many myths about how to prepare for vaccination. In fact, you should always proceed from how you feel. If a person is sick or does not feel well, they should temporarily refuse vaccination. In Russia, vaccination is voluntary.
A healthy person does not need any preliminary preparation, including testing. Before vaccination, you also do not need to take antihistamines or avoid normal physical activity.
Photo: master1305 / freepik.com
Immediately after the procedure, you should definitely wait at the vaccination office for about half an hour. This is necessary so that doctors can quickly provide the necessary assistance if an allergic reaction occurs. After vaccination, significant stress on the body is undesirable. It is better to postpone training in the gym, going to the bathhouse or to the beach for a couple of days. It is advisable to have the evening off after vaccination due to possible illness. Then it will be easier to bear possible unwanted post-vaccination effects.
I want to get vaccinated: instructions Since the increase in the incidence of influenza in Russia begins in the fall, it is better to get vaccinated against this infection in early September. However, you can get the vaccine later, even in winter. If you do not have exacerbations of chronic diseases or acute infections, feel free to go to the clinic.
- You can get a flu vaccine for free at any clinic. Take your passport and compulsory medical insurance policy with you.
- Contact your primary care physician. He will examine you and send you to the vaccination office. Be sure to tell your doctor if you have any allergies, in particular an allergy to egg whites. Find out which vaccine you will be vaccinated with.
- In the vaccination office, the doctor must open the vaccine preparation in front of you and, upon request, show you the packaging.
- After vaccination, spend 30 minutes in a medical facility in case of severe reactions.
- Follow all doctor's recommendations. For 3 days after vaccination, avoid physical activity, going to the pool or sauna. If you have a fever, you can take an antipyretic drug.
If you want to get a foreign flu vaccine, you can go to any commercial clinic and find out what products are available this year.
What to do
What to do when your hand is swollen after getting a flu shot? This situation should not cause panic or severe anxiety; most often, it does not threaten a person’s health in any way, but is only a temporary inconvenience that will not be difficult to get rid of.
What you can do to alleviate your own condition:
- to prevent such reactions, you should take antihistamines (recommended by your doctor) three days before and the next 3 days after vaccination;
- monitor the expiration dates and storage rules of the drug that the medical worker will use for the injection;
- do not wet the vaccination site for 24 hours, avoid excessive rubbing with clothing fabrics, or scratching if itching occurs;
- to alleviate the condition, apply an iodine mesh, use Fenistil gel, Troxevasin, Vitaon balm, Heparin ointment;
- apply a diluted solution of Dimexide to the injection site;
- use a slightly torn cabbage leaf or a slice of pickled cucumber;
- apply a tissue compress soaked in Novocaine solution to the site of inflammation;
- It is allowed to briefly apply a piece of ice wrapped in a napkin to the injection site.
Redness at the injection site requires seeking medical help if the diameter of its spread exceeds 8 cm, or there are signs of the development of a purulent process.
As a rule, redness or swelling of the injection site is not a cause for concern, but only an individual reaction of the body to the procedure that is not harmful to health.