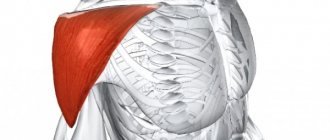
Features of intramuscular injections
Patient preparation
Possible complications after intramuscular injections
How much does an intramuscular injection cost in Moscow?
Intramuscular injection is a parenteral method of administering drugs, in which they are absorbed by muscle tissue and then enter the bloodstream through the capillary network. This is a simple, convenient and affordable way to administer medications. In terms of frequency of use, intramuscular injections are second only to the tablet method of drug administration.
Interested in where to get an intramuscular injection in Moscow? Do you need a good clinic with experienced doctors and trained medical staff in the Western District of the city? We invite you to “Stimul” on Yartsevskaya, 28.
- To make an appointment for an intramuscular injection or an appointment with a therapist to receive a referral, call 8
(ZAO Moscow, Kuntsevo district, Krylatskoye).
We work seven days a week. We accept cash and bank cards for payment. The dentistry is located a three-minute walk from the Molodezhnaya metro station (exit No. 2).
Loading a map
Needle breakage
Not often, but it does happen. The reason is strong muscle contraction due to fear of the procedure, unexpected start of injection, or improper psychological preparation of the patient.
Help: keeping calm, reassure the patient, assure him that everything will be fine. With the !-th and 2nd fingers of the left hand, press down the tissue on both sides of the broken needle, squeezing it out in this way. Take tweezers with your right hand, carefully grab the tip of the fragment and remove it. The action is repeated several times. If attempts are unsuccessful, urgently call a doctor through an intermediary, remaining with the patient and reassuring him. In the future, follow all the doctor’s instructions.
Consequences of air ingress
Situations in which air ends up in a vein are called embolism in the medical literature. They happen extremely rarely, but if they do occur, the following can happen in the body:
- Blockage of a vessel. The likelihood of this result is highest in people who have atherosclerotic plaques and suffer from hypertension. In both cases, vessel patency is reduced, which increases the likelihood of blockage
- Atrial stretch. Air that has entered the circulatory system and freely reaches the myocardium is collected in the right part of the myocardium, from where it is not able to freely exit. If its amount is quite high, muscle tissue is stretched, which has an extremely negative effect on the functioning of the heart, causing arrhythmia, paroxysms and more serious dysfunctions.
- Death. Occurs when an exorbitant volume of air (from twenty cubic meters) is introduced into a vein. The likelihood of its occurrence is greatly increased in people with cardiovascular diseases
Despite the fact that the possibility of air entering the circulatory system during an intravenous injection or placement of a drip cannot be completely excluded, doctors assure that its volume cannot cause significant harm to a healthy person. Dangerous consequences are fraught only with the deliberate introduction of an impressive amount of air or its accidental penetration during surgery, injury, childbirth, or in other emergency situations.
Emboli
Oil and suspension embolisms occur when a needle enters the lumen of a blood vessel with subsequent administration of a drug. If there is insufficient air displacement from the syringe, there is a risk of an air embolism if the entire contents of the syringe are injected into the blood vessel where the needle entered.
Help: place the patient in a lateral position with the head raised, immediately call a doctor through an intermediary.
Prevention: complete displacement of air from the lumen of the syringe, “pulling back” the piston when the needle is inserted with the intention of introducing oil or suspension solutions.
Possible complications after intramuscular injections
- Hematomas are small subcutaneous hemorrhages (incorrect technique for intramuscular injections, use of old, blunt or deformed needles).
- Infiltrates - subcutaneous compactions at the injection sites (frequent injections into the same muscle, injection of unheated oily drugs into the muscle, injection of medication more than the permissible volume).
- Needle breakage - the needle partially or completely remains in the patient’s body (use of low-quality or old games, deep insertion of the needle, injection into a tense muscle).
- Oil embolism is the entry of oily drugs into the bloodstream and further blockage of the vessel (during the injection, the needle entered the vessel and not the muscle).
Most complications occur when you are given the injection incorrectly. Therefore, do not trust your health to random people. Without medical training, they can make the situation worse: if something goes wrong, they will not be able to help you promptly, and this can lead to unpleasant consequences.
If you need intramuscular injections, they can be done in our clinic. We will do it quickly, safely and painlessly. You can make an appointment using the contact numbers that you will find on our website.
Allergic reactions
When any drug is administered, the patient may experience an allergic reaction from urticaria to anaphylactic shock . The treatment room should be equipped with an anti-shock first aid kit and instruments to assist in respiratory arrest.
Knowing the possible complications after IM injections, the nurse should make every possible effort to prevent them. And if any complication arises, be ready to take the necessary actions on your part.
Article “Post-injection complications in the work of a nurse”
Post-injection complications
Infiltrate
- the most common complication after subcutaneous and intramuscular injections - is considered as a nosocomial infection.
Most often, infiltration occurs if: a) the injection is performed with a blunt needle; b) for intramuscular injection, a short needle intended for intradermal or subcutaneous injections is used. Some drugs, when administered intramuscularly with a short needle, cause severe chemical irritation of tissues and are absorbed for a long time, which together leads to the formation of infiltrates. Inaccurate choice of injection site, frequent injections into the same place, violation of aseptic rules are also the cause of infiltrates. Infiltration is characterized by the formation of a compaction at the injection site, which is easily determined by palpation (feeling).
Abscess
- purulent inflammation of soft tissues with the formation of a cavity filled with pus and delimited from surrounding tissues by a pyogenic membrane.
The reasons for the formation of an abscess are the same as for infiltrates. With infiltration and abscess, soft tissue becomes infected as a result of violation of asepsis rules. These complications belong to the group of nosocomial infections.
Needle breakage
during injection is possible when using old, worn needles, as well as when there is a sharp contraction of the buttock muscles during an intramuscular injection, if a psychoprophylactic conversation is not held with the patient before the injection or the injection is given to the patient in a standing position.
Drug embolism
(Greek Embolia - throwing in) can occur when injecting oil solutions subcutaneously or intramuscularly (oil solutions are not injected intravenously!) and the needle gets into the vessel. Oil, once in the artery, will clog it and this will lead to disruption of the nutrition of surrounding tissues and their necrosis. Signs of necrosis: increasing pain in the injection area, swelling, redness or red-bluish discoloration of the skin, increased local and general temperature. If the oil ends up in a vein, it will enter the pulmonary vessels through the bloodstream. Symptoms of pulmonary embolism: a sudden attack of suffocation, cough, blue discoloration of the upper half of the body (cyanosis), a feeling of tightness in the chest.
1
Air embolism
with intravenous injections and infusions it is the same dangerous complication as oil. The signs of air embolism are the same as oil embolism, but they appear very quickly (within a minute), since the cubital vein is large and anatomically located close to the pulmonary vessels.
Incorrect administration of a drug
should also be considered as a complication of the injection. In such cases, a 0.9 percent sodium chloride solution, a total of 50-80 ml, should be immediately injected into the injection site and around it. This will reduce the concentration of the erroneously administered drug and reduce its irritating effect on the tissue. For this purpose, you can place an ice pack at the injection site.
The antagonist of an erroneously administered drug can be administered only as prescribed by a doctor.
If the drug is administered (erroneously) subcutaneously, then before administering an isotonic sodium chloride solution, a tourniquet should be applied above the injection site (this will slow down the absorption of the drug).
Damage to nerve trunks
can occur with intramuscular and intravenous injections, either mechanically (if the injection site is chosen incorrectly), or chemically, when the drug depot is near the nerve (with intravenous injection, part of the drug may end up under the skin), as well as when the vessel supplying the nerve is blocked . The severity of the complication can vary - from neuritis (inflammation of the nerve) to paralysis (loss of function) of the limb.
Thrombophlebitis
- inflammation of a vein with the formation of a blood clot in it - observed with frequent venipunctures of the same vein, or when using insufficiently sharp needles. Signs of thrombophlebitis are pain, skin hyperemia and the formation of infiltrate along the vein. Body temperature may be low-grade.
Necrosis
(death) of tissue can develop when venipuncture is unsuccessful and a significant amount of an irritating agent is mistakenly introduced under the skin. Penetration of the drug under the skin during venipuncture is possible due to:
- piercing the vein “through and through”;
- failure to enter the vein initially.
2
Most often this happens with inept intravenous administration of a 10% calcium chloride solution. If the solution does get under the skin, you should act in the same way as if you administered the drug by mistake, only in this case an ice pack is not applied, since a 10% calcium chloride solution is dangerous only due to its local irritant effect, and not its resorptive effect.
Hematoma
(hemorrhage under the skin) can also occur during inept venipuncture: a purple spot appears under the skin, as the needle pierced both walls of the vein and blood penetrated into the tissue. In this case, the puncture of this vein should be stopped and pressed for several minutes with cotton wool (napkin) and alcohol. In this case, the intravenous injection prescribed to the patient is given into another vein, and a local warming (semi-alcohol) compress is placed on the area of the hematoma.
Sepsis
(generalized form of infection) can occur due to gross violations of aseptic rules during intravenous injection or infusion, as well as when using non-sterile solutions. Sepsis also belongs to the group of nosocomial infections.
Long-term complications that occur 2-4 months after the injection include viral hepatitis B, D, non-A, non-B (serum hepatitis), C, D - an infectious disease whose incubation period lasts 2-6 months, as well as HIV infection, in which the incubation period ranges from 6-12 weeks to several months. These complications are nosocomial infections.
Allergic reactions
to the administration of a particular drug by injection can occur in the form of urticaria, acute runny nose, acute conjunctivitis, Quincke's edema. The most dangerous form of an allergic reaction is anaphylactic shock.
When some drugs are administered intravenously, a local allergic reaction is observed. If the patient develops an allergic reaction, the doctor must be immediately informed and emergency care must be started.
Anaphylactic shock develops within a few seconds or minutes from the moment the drug is administered. The faster the shock develops, the worse the prognosis. The lightning-fast course of shock ends in death. Most often, anaphylactic shock is characterized by the following sequence of symptoms: general redness of the skin, rash, coughing attacks, severe anxiety, irregular breathing, decreased blood pressure, and arrhythmia of the heartbeat.
3
Symptoms can appear in various combinations. Death usually occurs from acute respiratory failure due to bronchospasm and pulmonary edema, acute cardiovascular failure.
***************
Post-injection complications
attracted the attention of doctors more than a hundred years ago, immediately after the invention of the syringe in 1853 and the first injections in 1855.
The widespread introduction of disposable syringes into medical practice has greatly facilitated and simplified the procedure for intramuscular and subcutaneous injections. However, the frequency of post-injection complications and their treatment still remain one of the pressing problems.
Modern medicine is unthinkable without the use of a large number of injections. Thus, according to a number of researchers, in Russia over 1 million injections are performed daily for the purpose of treatment, immunization and diagnostic studies. In parallel with the increase in the number of injections, the number of post-injection complications also increases.
Considering the frequency of the disease, its gradual increase, the involvement of medical workers in the occurrence of post-injection complications and the unsatisfactory results of treatment of this pathology, attention should be paid to the causes of post-injection complications: where, by whom and when injections performed most often lead to complications, which medications are more often complicated by abscesses and phlegmons ; what is the mechanism of development of the pathological process; what methods can be used to clarify the diagnosis of post-injection complications; which treatment method will be optimal when choosing treatment in each specific case.
Post-injection complications
1) Pyrogenic reactions .
Accompanied by a sharp rise in temperature and stunning chills. This happens when using drugs that have expired, or introducing poorly prepared solutions;
4
2) Fat embolism of the pulmonary vessels.
Occurs when drugs intended for internal or subcutaneous administration, such as a solution of camphor in oil, are mistakenly administered into a vein. Fat embolism is manifested by sudden pain in the heart area, choking, coughing, blueness of the face, upper half of the chest;
3) Air embolism of pulmonary vessels.
It occurs when air bubbles that are not promptly removed from the syringe or blood transfusion systems enter;
4) Dizziness, collapse, heart rhythm disturbance.
May be a consequence of too rapid administration of the drug;
5) Infiltration.
Formed when the drug enters the subcutaneous tissue. This occurs in the case of through perforation of the vein. Getting drugs such as euphyllia and calcium chloride under the skin is very painful. If this happens, it is recommended to place a semi-alcohol or dry compress on the elbow area;
6) Hematoma.
It is more often formed in patients with impaired blood clotting or increased vascular permeability. Prevention of this complication is long-term (3-5 minutes) and firm pressure on the site and injection;
7) Sepsis.
It can develop when the rules of eseptic and antiseptic conditions are violated;
 Phlebitis.
Phlebitis.
Inflammation of a vein caused by chemical or physical irritation is often accompanied by thrombosis of the affected vessel;
9) Allergic reactions.
May occur with most medications. They manifest themselves in the form of skin itching, skin rashes, and Quincke's edema. The most dangerous form of an allergic reaction is anaphylactic shock (shortness of breath, nausea, itchy skin, decreased blood pressure, loss of consciousness, bluish skin). If the patient develops any of these symptoms, you should immediately stop administering the medication and immediately provide emergency assistance. Anaphylactic shock develops within a few seconds or minutes from the moment the drug is administered. The faster the shock develops, the worse the prognosis. The main symptoms of anaphylactic shock: a feeling of heat in the body, a feeling of tightness in the chest, suffocation, dizziness, headache, anxiety, severe weakness, decreased blood pressure, heart rhythm disturbances. In severe cases, these signs are accompanied by symptoms of collapse, and death can occur a few minutes after the first symptoms of anaphylactic shock appear. Treatment for anaphylactic shock should be carried out immediately upon detection of a feeling of heat in the body.
5
Long-term complications that occur two to four months after the injection are viral hepatitis B, D, C, as well as HIV infection;
10) Abscess
- purulent inflammation of soft tissues with the formation of a cavity filled with pus. The reasons for the formation of abscesses are the same as for infiltrates. In this case, infection of soft tissues occurs as a result of violation of asepsis rules.
11) Damage to nerve trunks
can occur with intramuscular and intravenous injections, either mechanically (if the injection site is chosen incorrectly), or chemically, when the drug depot is located next to the nerve, as well as when the vessel supplying the nerve is blocked. The severity of the complication can vary - from neuritis to paralysis of a limb.
12) Thrombophlebitis
- inflammation of a vein with the formation of a blood clot in it - observed with frequent venipunctures of the same vein, or when using blunt needles. Signs of thrombophlebitis are pain, skin hyperemia and the formation of infiltrate along the vein. The temperature may be low-grade.
13) Necrosis
tissue can develop due to unsuccessful vein puncture and erroneous injection of a significant amount of irritating agent under the skin. Ingress of drugs along the course of venipuncture is possible due to: piercing the vein “through and through”; failure to enter the vein initially. Most often this happens with inept intravenous administration of a 10% calcium chloride solution. If the solution does get under the skin, you should immediately apply a tourniquet above the injection site, then inject a 0.9% sodium chloride solution into the injection site and around it, a total of 50-80 ml (it will reduce the concentration of the drug).
Conclusion
If sanitary and epidemiological requirements for performing medical procedures are violated, an artificial mechanism of infection transmission may be triggered. Any of the invasive procedures can lead to infection. A special place among various hospital infections is occupied by post-injection complications due to the high frequency of injection interventions. Here's what you need to do to have fewer post-injection complications:
The nurse must be careful not to mix up the medications, make a good injection (for example, accurately hit the vein);
- Ensuring high-quality disinfection and sterilization of consumables, medical products used for injections, catheterization;
6
Strict adherence to antisepsis and asepsis when carrying out parenteral manipulations;
Compliance with the technique of hygienic washing and hygienic antisepsis of the hands of medical personnel in treatment rooms, vaccination rooms, and those performing parenteral injection procedures;
Antiseptic treatment of the patient's skin before injection;
Compliance with the sanitary and anti-epidemic regime in treatment rooms, vaccination rooms, and manipulation rooms. Carrying out production and laboratory control in treatment rooms, vaccination rooms, and manipulation rooms.
7
What to do if air does get into a vein
If the incident took place in a hospital, medical personnel must immediately take measures to prevent negative consequences from occurring. These include:
- Hemostasis. It is performed through surgery. Designed to surgically remove air from the system
- Oxygen inhalations. Helps dissolve an air bubble (or several bubbles) in the blood
- Exposure to saline solution. Presumably damaged vessels are exposed to it
- Sessions in a pressure chamber. Helps normalize blood pressure, dissolve air inside the myocardium and in the vein
- Air aspiration. If its location is localized, the air is pumped out of the vein along with the blood
- Drug therapy. The patient is shown drugs that stimulate the cardiovascular system, normalize blood pressure, pulse and vein size; a dropper can be used for administration
- Steroid drugs. Indicated in cases of swelling of the brain caused by the penetration of air into the blood.
If air has entered a vein at home, you should immediately contact qualified specialists by calling an ambulance. Before her arrival, you need to remove the IV and take a comfortable position. If a vein is swollen, it makes sense to tighten it to prevent air from entering the myocardium.
Signs of air entering the circulatory system
If a mistake has been made, it cannot always be seen visually. If after the injection the following signs appear, it can be assumed with a high degree of probability that he got there:
- Painful sensations in the chest area. Occurs when the myocardium experiences a lack of blood supply due to an obstruction in the circulatory system in the form of air
- Bumps, bruises at the puncture site from the IV. The signs are indirect, but they quite often accompany airing
- Weakness, faintness, clouding of consciousness. It happens when a vesicle blocks a vein that supplies the brain
- A swollen vein, numbness in the extremities (usually the arms). This condition occurs if the bubble does not move towards the heart muscle, but is stuck at the entrance to a narrower bloodstream (the size of which is congenital or acquired)
- Wheezing in the chest, shortness of breath, drop in blood pressure, increase in heart rate, arrhythmia. Symptoms may indicate that air, having passed through the circulatory system, has entered the myocardium