How to give injections correctly
The drug must be injected into the subcutaneous fat layer. To do this, you will have to overcome the barrier of the skin, the thickness of which in adult patients and adolescents often varies between 2-2.5 mm. In children, the dermis is slightly thinner. A special insulin syringe with a 4 mm needle is sufficient for a safe puncture.
It is convenient to use automatic syringe pens that allow you to set the puncture depth. They also automatically administer a predetermined dose of insulin.
Attention: you should try to avoid intramuscular administration of the medicine! This leads to too rapid absorption of the substance and sharp jumps in glucose levels in the circulatory system.
There is no need to wipe the insulin injection site with alcohol. For better suction, it is permissible to lightly press this area with your fingertips (do not rub too hard).
Complications after insulin injections
The subcutaneous layer has a rich blood supply, so when insulin is administered every day, a bruise or hematoma at the injection site . The cause may be either using a needle that is too long or reusing the same needle. Change the needles in your insulin pen often - this will reduce discomfort if insulin is injected every day!
If insulin leaks from the cartridge before an injection , this may be due to storing the insulin pen with the needle (if the needle is not removed after the injection) or to an incorrectly inserted needle.
If insulin leaks from the injection site after an injection, this may be due to the injection of too much insulin. A dose exceeding 40–50 units is recommended to be divided into two parts. A second reason for insulin leaking from the injection site may be removing the needle too quickly after the injection. As mentioned above, after administering insulin, you need to release the skin fold, wait 10 seconds and only then remove the needle, pressing the injection site with a cotton swab or napkin.
One of the most unpleasant complications after insulin injections is lipohypertrophy - a local increase in adipose tissue at the sites of repeated insulin injection. In order to avoid the development of lipohypertrophy, it is necessary to change the site of insulin administration. The risk of lipohypertrophy is also increased by repeated use of the needle, as this injures the tissue.
Which part of the body to inject into?
There are several places on the human body for insulin injections. This:
- upper anterior abdomen: approximately 1 cm below the last rib, 1 cm to the side of the navel;
- middle third of the outer part of the shoulder;
- the anterior upper surface of the thigh (third closest to the groin);
- upper buttocks;
- base of the scapula, to the right or left of the spinal column.
It is not recommended to inject the hormone into the arm on your own, since there is no possibility of creating a skin pocket, which increases the risk of intramuscular injection of the drug. For the same reason, unsuitable places for insulin injections in children and thin people are the shoulders and legs due to insufficient thickness of the fat layer.
Possible complications from insulin injections
First of all, study the article “Low blood sugar (hypoglycemia)”. Do what it says before you start treating diabetes with insulin. The insulin therapy protocols described on this site greatly reduce the risk of severe hypoglycemia and other less dangerous complications.
Repeatedly injecting insulin into the same areas can cause thickening of the skin called lipohypertrophy. If you continue to inject in the same places, the drugs will be absorbed much worse, and blood sugar will begin to jump. Lipohypertrophy is determined visually and by touch. This is a serious complication of insulin therapy. The skin may be red, hard, swollen, or swollen. Stop injecting medications there for the next 6 months.
Lipohypertrophy: a complication of improper treatment of diabetes with insulin
To prevent lipohypertrophy, change injection sites each time. Divide the areas you are injecting into into areas as shown in the picture. Use different areas alternately. In any case, inject insulin at a distance of at least 2-3 cm from the previous injection site. Some diabetics continue to inject their medications into areas of lipohypertrophy because such injections are less painful. Stop this practice. Learn to give injections with an insulin syringe or pen painlessly, as described on this page.
Why does blood sometimes flow after an injection?
Sometimes during insulin injections, the needle gets into small blood vessels (capillaries), causing bleeding. This happens periodically to all diabetics. This should not be a cause for concern. Bleeding usually stops on its own. They leave small bruises for several days.
Blood getting on your clothes can be a nuisance. Some advanced diabetics carry hydrogen peroxide with them to quickly and easily remove blood stains from clothing. However, do not use this product to stop bleeding or disinfect the skin because it may cause burns and impede healing. For the same reason, you should not smear with iodine or brilliant green.
Some of the injected insulin flows out along with the blood. Do not try to immediately compensate for this with a second injection. Because the dose received may be too high and cause hypoglycemia (low glucose levels). In the self-monitoring diary you need to indicate that bleeding occurred and, perhaps, some of the injected insulin leaked out. This will help explain later why the sugar was higher than usual.
You may need to increase the dose of the drug with your next injection. However, there is no need to rush into it. At least 4 hours must pass between two injections of short-acting or ultra-short-acting insulin. Two doses of rapid insulin should not be allowed to act in the body at the same time.
Why there may be red spots and itching at the injection site
Most likely, subcutaneous hemorrhage occurred due to the fact that the needle accidentally touched a blood vessel (capillary). This often happens in diabetics who inject insulin into the arm, leg, or other inappropriate places. Because they give themselves intramuscular injections instead of subcutaneous ones.
Many patients think that red spots and itching are manifestations of an allergy to insulin. However, in practice, allergies are rare after animal insulin preparations are abandoned.
An allergy should be suspected only in cases where red spots and itching occur repeatedly after injections in different places. Nowadays, insulin intolerance in children and adults, as a rule, is of a psychosomatic nature.
Diabetics who follow a low-carbohydrate diet require insulin dosages 2-8 times lower than standard. This significantly reduces the risk of complications of insulin therapy.
Dependence of hormone absorption on injection site
The speed and efficiency of drug absorption depend on where insulin is injected for diabetes. We present the main indicators in table form.
| injection site | suction efficiency (%) | suction speed |
| stomach | 90 | fastest |
| shoulder | 70 | fast enough |
| buttock | 70 | slower |
| hip | 70 | slow |
| spatula | 30 | slowest |
From the data given in the table, it follows that it is better not to give injections in the scapular area, since they are the least effective.
If a person injects the hormone on his own, then the short-acting must be injected into the stomach , and the long-acting drug into the leg, because in the legs the absorption rate is much lower.
When injections are given by relatives, the “short” hormone can be injected into the arm, the “long” one into the buttock, where the absorption rate is also lower. A similar scheme is relevant for young children, since such injections are the least painful.
Injection technique and means of administering insulin
The beginning of the practical use of insulin almost 85 years ago remains one of the few events whose significance is not disputed by modern medicine. Since then, many millions of insulin-dependent patients around the world have been saved from death as a result of diabetic coma. Lifelong insulin replacement treatment has become the main condition for the survival of patients with type 1 diabetes, and it also plays an important role in the treatment of a certain part of patients with type 2 diabetes. In the early years, there were quite a lot of problems associated with obtaining the drug, the technique of its administration, and changing doses, but gradually all these issues were resolved. Now, every diabetic patient with a need for insulin, instead of the phrase “We are forced to inject insulin,” should say: “We have the opportunity to inject insulin.” In recent years, interest in the possibilities of improving insulin therapy, i.e., bringing it closer to physiological conditions, has been constantly growing. A certain role here is played not only by the focus on reducing lifestyle restrictions and improving the quality of life, but also by recognizing the need for fundamental changes aimed at improving metabolic control. J. J. R. MacLeod (whose assistants, Frederick Banting and Charles Best, discovered insulin in 1921) wrote in his book “Insulin and its Use in the Treatment of Diabetes”: “So that the patient can trust himself with his own life, he you need to be excellent at determining the dose and administering insulin...” This phrase is still relevant today, since there is no replacement for subcutaneous insulin administration in the foreseeable future.
In this regard, it is very important to correctly use insulin and modern means of its administration, which include syringes, syringe pens, and wearable insulin pumps.
Insulin storage
Like any drug, insulin has a limited shelf life. Each bottle must indicate the expiration date of the drug. The insulin supply must be stored in the refrigerator at a temperature of + 2 ... + 8 ° C (under no circumstances should it be frozen). Insulin vials or pens used for daily injections can be stored at room temperature for 1 month. You should also not allow the insulin to overheat (for example, do not leave it in the sun or in a closed car in the summer). After the injection, be sure to put the insulin bottle in a paper package, since insulin activity decreases under the influence of light (the syringe pen is closed with a cap). When transporting a supply of insulin (during vacation, business trip, etc.), it is not recommended to check it in your luggage, as it can get lost, break, freeze or overheat.
Insulin syringes
Glass syringes are inconvenient (require sterilization) and cannot provide a sufficiently accurate dosage of insulin, so today they are practically not used. When using plastic syringes, syringes with a built-in needle are recommended to eliminate the so-called “dead space” in which a certain amount of solution remains in a regular syringe with a removable needle after injection. Thus, with each administration, a certain amount of the drug is lost, which, given the scale of the incidence of diabetes, results in huge economic losses. Plastic syringes can be used repeatedly, provided they are handled correctly and hygienically. It is desirable that the dividing price of an insulin syringe should not be more than 1 unit, and for children - 0.5 units.
Insulin concentration
Plastic syringes are available for insulin with a concentration of 40 U/ml and 100 U/ml, so when receiving or purchasing a new batch of syringes, you should pay attention to their scale. Patients traveling abroad should also be warned that in most countries only insulin with a concentration of 100 U/ml and appropriate syringes are used. In Russia, insulin is currently found in both concentrations, although the world's leading insulin manufacturers supply it in a concentration of 100 units per ml.
Set of insulin in a syringe
The sequence of actions when collecting insulin using a syringe is as follows:
- prepare a bottle of insulin and a syringe;
- if necessary, inject long-acting insulin, mix it well (roll the bottle between your palms until the solution becomes evenly cloudy);
- draw as much air into the syringe as the number of units of insulin you will need to draw later;
- introduce air into the bottle;
- First, draw a little more insulin into the syringe than you need. This is done to make it easier to remove air bubbles trapped in the syringe. To do this, lightly tap the body of the syringe and release the excess amount of insulin along with the air back into the bottle.
Mixing insulins in one syringe
The ability to mix short- and long-acting insulins in one syringe depends on the type of long-acting insulin. Only insulins that contain protein (NPH insulins) can be mixed. Analogs of human insulin that have appeared in recent years should not be mixed. The advisability of mixing insulin is explained by the possibility of reducing the number of injections. The sequence of actions when putting two insulins into one syringe is as follows:
- introduce air into the vial of extended-release insulin;
- introduce air into the vial of short-acting insulin;
- first dial up short-acting insulin (transparent), as described above;
- then dial in extended-release insulin (cloudy). This should be done carefully so that part of the already collected “short-acting” insulin does not end up in the bottle with the extended-release drug.
Insulin injection technique
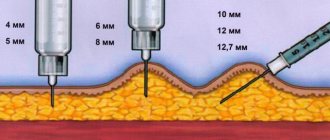
| Figure 1. Injecting insulin with needles of different lengths |
The rate at which insulin is absorbed depends on where the needle is inserted. Insulin injections should always be given into subcutaneous fat and not intradermally or intramuscularly (Figure 1). It turned out that the thickness of the subcutaneous tissue in people with normal weight, especially in children, is often less than the length of a standard insulin needle (12–13 mm). Experience shows that very often patients do not form a fold and inject at a right angle, which leads to insulin entering the muscle. This was confirmed by special studies using ultrasound equipment and computed tomography. Periodic release of insulin into the muscle layer can lead to unpredictable fluctuations in glycemic levels. In order to avoid the possibility of an intramuscular injection, you should use short insulin needles - 8 mm long (Becton Dickinson Microfine, Novofine, Dizetronic). In addition, these needles are the thinnest. If the diameter of standard needles is 0.4; 0.36 or 0.33 mm, then the diameter of the shortened needle is only 0.3 or 0.25 mm. This is especially true for children, since such a needle causes virtually no pain. Recently, shorter (5–6 mm) needles have been proposed, which are more often used in children, but further reduction in length increases the likelihood of intradermal penetration.
To give an insulin injection, you need the following:
| Figure 2. Formation of a fold of skin for insulin injection |
- make room on the skin where insulin will be injected. There is no need to wipe the injection site with alcohol;
- With your thumb and forefinger, take the skin into a fold (Fig. 2). This is also done to reduce the likelihood of getting into the muscle. This is not necessary when using the shortest needles;
- insert the needle at the base of the skin fold perpendicular to the surface or at an angle of 45°;
- Without releasing the fold (!), press the syringe plunger all the way;
- wait a few seconds after injecting insulin, then remove the needle.
Insulin injection areas
Several areas are used for insulin injections: the front surface of the abdomen, the front surface of the thighs, the outer surface of the shoulders, buttocks (Fig. 3). It is not recommended to inject yourself into the shoulder, since it is impossible to form a fold, which means the risk of intramuscular injection of insulin increases. You should be aware that insulin is absorbed from different areas of the body at different rates (for example, the abdominal area is the fastest). Therefore, it is recommended to inject short-acting insulin into this area before meals. Long-acting insulin injections can be given in the thighs or buttocks. The injection site must be new every day, otherwise there may be fluctuations in blood sugar levels.
| Figure 3. Insulin injection areas |
You should also ensure that changes do not appear at the injection sites - lipodystrophy, which impairs the absorption of insulin (see below). To do this, it is necessary to alternate injection sites, and also retreat from the previous injection site by at least 2 cm.
Syringe pens
In recent years, along with plastic insulin syringes, semi-automatic insulin dispensers, the so-called syringe pens, have become increasingly common. Their device resembles an ink fountain pen, in which instead of an ink reservoir there is an insulin cartridge, and instead of a pen there is a disposable insulin needle. Similar “pens” are now produced by almost all foreign insulin manufacturers (Novo Nordisk, Eli Lilly, Aventis), as well as medical equipment manufacturers (Becton Dickinson). They were originally developed for patients with visual impairment who could not draw insulin into a syringe on their own. Subsequently, they began to be used by all patients with diabetes, as they can improve the patient’s quality of life: there is no need to carry a bottle of insulin with you and draw it with a syringe. This is especially significant with modern regimens of intensified insulin therapy, when the patient has to give injections multiple times during the day (Fig. 4).
| Figure 4. Intensified insulin therapy regimen using multiple injections |
However, mastering the injection technique using a pen syringe is somewhat more difficult, so patients should carefully study the instructions for use and strictly adhere to all instructions. One of the disadvantages of syringe pens is that when a small amount of insulin remains in the cartridge (less than the dose the patient needs), many patients simply throw away such a cartridge and the insulin along with it. In addition, if a patient injects short- and long-acting insulins in an individually selected ratio (for example, with intensified insulin therapy), then he is deprived of the opportunity to mix and inject them together (as in a syringe): he has to inject them separately with two “handles”, thus increasing number of injections. As in the case of insulin syringes, an important requirement for injectors is the ability to dose in multiples of 1 unit, and for small children - in multiples of 0.5 units. Before injecting long-acting insulin, you need to make 10-12 turns of the pen 180° so that the ball in the cartridge mixes the insulin evenly. The dial ring places the required dose in the housing window. Having inserted the needle under the skin as described above, press the button all the way. After 7–10 seconds (!), remove the needle.
The very first syringe pen was Novopen, created in 1985. The required dose was administered discretely with its help, since only 1 or 2 units could be administered with each button press.
The next generations of syringe pens made it possible to administer the entire dose at once, having previously determined it. Currently in Russia, syringe pens are used, into which a 3 ml cartridge (300 units of insulin) is inserted. These include Novopen 3, Humapen, Optipen, Innovo.
Novopen 3 is intended for the administration of insulins from Novo Nordisk. The syringe pen has a body made of plastic and metal. It allows you to simultaneously administer up to 70 units of insulin, with an injection step of 1 unit. In addition to the classic silver version, multi-colored syringe pens are available (so as not to confuse different insulins). For children, there is a modification of Novopen 3 Demi, which allows insulin to be administered at a dose rate of 0.5 units.
The Humapen syringe pen is designed for administering Eli Lilly insulins. The pen is very easy to use; you can easily recharge the cartridge (due to a special mechanism), as well as correct an incorrect dose. The body of the device is entirely plastic, which reduces its weight, and the specially developed ergonomic design of the body makes it comfortable for the hand during injection. The color inserts on the body are designed for the use of different insulins. Humapen allows you to simultaneously administer up to 60 units of insulin, the dose increment is 1 unit.
The Optipen syringe pen is designed for administering Aventis insulins. Its main difference from other models is the presence of a liquid crystal display, which displays the dose to be administered. The most common option on the Russian market is Optipen Pro 1. It allows you to simultaneously administer up to 60 units of insulin, the number “1” means that the dose increment is 1 unit. Another advantage of this model is the fact that it is impossible to set a dose greater than the amount of insulin remaining in the cartridge.
In 1999, Novo Nordisk released a new syringe pen, Innovo. Due to a special mechanism, the length of the device was reduced. Like Optipen, the dose is displayed on the liquid crystal display. But the main difference from all previous modifications is that Innovo shows the time that has passed since the last injection and remembers the last dose of insulin. Also, the electronic control system guarantees accurate administration of the dialed dose. The range of administered doses is from 1 to 70 units, the dosing step is 1 unit. The set dose can be increased or decreased by simply turning the doser forward or backward without losing insulin. It is impossible to set a dose greater than the amount of insulin remaining in the cartridge.
Changing needles
Since a patient on insulin therapy has to make a huge number of injections during his life, the quality of insulin needles becomes of great importance. In order to ensure that insulin administration is as comfortable as possible, manufacturers are constantly making needles thinner, shorter, and sharper. To make insulin injection virtually painless, the needle tip is specially sharpened and lubricated using the latest technology. However, repeated and repeated use of the insulin needle leads to damage to the tip and abrasion of the lubricating coating, which increases pain and discomfort. A dull needle not only makes insulin injection painful, but can cause local hemorrhage. In addition, erasing the lubricant on the needle increases the force of pushing the needle through the skin, which increases the risk of bending the needle and even breaking it. However, the main argument against repeated use of a needle is microtrauma to the tissue. The fact is that when the needle is reused, its tip bends, taking on the shape of a hook, which is clearly visible under a microscope (Fig. 5). When the needle is removed after insulin is administered, the hook ruptures the tissue, causing microtrauma. This contributes to the formation in a number of patients of protruding compactions (plus tissue) at the sites of insulin injections, i.e. lipodystrophies. In addition to causing cosmetic damage, lipodystrophic lumps can have serious medical consequences. Often, patients continue to inject insulin into these seals due to the fact that injections in these places are less painful. However, insulin absorption at these sites occurs unevenly, which may result in poor glycemic control. Quite often in such situations, an erroneous diagnosis of “labile diabetes” is made.
| Figure 5. Deformation of insulin needles after repeated use. |
Repeated use of the needle can cause insulin crystals to clog the channel, which in turn makes insulin delivery difficult and inadequate.
Repeated use of insulin pen needles can lead to another serious mistake. The instructions for syringe pens state that the needle must be removed after each injection. But most patients do not comply with this rule (due to the fact that an insufficient number of needles are provided free of charge). Thus, the channel between the insulin cartridge and the environment remains open. As a result of temperature fluctuations, insulin leaks and air enters the vial. The presence of air bubbles in the insulin cartridge causes insulin to be delivered more slowly as the plunger is pushed. As a result, the insulin dose administered may not be accurate. In the presence of large air bubbles, the amount of insulin administered in some cases may be only 50–70% of the administered dose. In order to reduce the influence of this factor, it is necessary to remove the needle not immediately, but 7–10 s after the piston has reached its lower position, which is what patients should be instructed to do.
What conclusions can be drawn based on all the above observations? Ideally, single use of insulin needles should be recommended; in addition, after each injection of insulin, the needle must be removed immediately.
Given the importance of the above points, doctors should periodically check the means of insulin administration, injection technique and the condition of injection sites in each patient.
Insulin pumps
Wearable insulin dispensers (insulin pumps) appeared in the late 1970s. The next decade was characterized by intense interest in these new technical means of administering insulin, and certain hopes were placed on them. After gaining experience and conducting a sufficient number of scientific and clinical studies, the pump “boom” subsided, and these devices took their definite place in modern insulin therapy. In Russia, Medtronic Minimed pumps are currently used.
When using dispensers, the following occurs (Fig. 6): to simulate physiological secretion through a cannula installed in the body (the injection site changes every 2–3 days), short-acting insulin is pumped continuously as a subcutaneous infusion (basal rate), and before meals the patient injects Various additional amounts of insulin (bolus).
| Figure 6. Intensified insulin therapy regimen using a pump |
Thus, the device is an “open” type system. This means that the patient regulates the insulin dosage himself, changing it depending on the results of self-monitoring of glycemia. The latter is the link that, as it were, “closes the chain”, forming feedback. One of the main advantages of current wearable pumps is the ability to vary the basal insulin infusion rate. Modern pumps allow you to set different speeds for each hour of the day, which helps to cope with such a phenomenon as the “dawn phenomenon” (an increase in glycemic levels in the early morning hours, forcing patients in this case to make the first insulin injection at 5–6 a.m.). Also, the use of pumps allows you to reduce the number of injections, show greater flexibility regarding the timing of meals and the amount of carbohydrates consumed. There are also implantable pumps in which insulin enters intraperitoneally, which means it enters the portal vein, as happens during normal insulin secretion.
However, numerous studies have shown that there is no significant difference in the level of metabolic control between patients using insulin pumps and those on a multiple-injection regimen. The biggest disadvantage is the high cost of pumps. The use of pumps is clearly justified in certain situations, for example, during pregnancy, in children with labile diabetes, etc. A miniature, portable device that not only injects insulin, but also has a sensor for determining glycemia, as well as an automated insulin supply function based on the results obtained, i.e., it would be an artificial b-cell, has not yet been developed for long-term clinical use. However, experimental models already exist, and mass production of such devices may begin in the near future. In this regard, interest in the use of conventional pumps has increased, since both medical workers and patients need to get used to handling complex technical devices.
Thus, today we have in our arsenal means of self-monitoring and insulin administration, which in many ways allow us to optimize the treatment of patients with diabetes. All that remains is to teach patients to use them correctly, which is no less difficult a task than the creation of these funds itself.
Literature
- Berger M., Starostina E. G., Jorgens V., Dedov I. I. Practice of insulin therapy (with the participation of Antsiferov M. B., Galstyan G. R., Grüsser M., Kemmer F., Mulhauser I., Savitsky P ., Chantelau E., Spraulya M., Starke A.). 1st ed. Springer-Verlag, Berlin-Heidelberg, 1995.
- Dedov I. I., Mayorov A. Yu., Surkova E. V. Diabetes mellitus type I: A book for patients. M., 2003.
- Dedov I. I., Surkova E. V., Mayorov A. Yu., Galstyan G. R., Tokmakova A. Yu. Therapeutic training of patients with diabetes mellitus. M.: Reafarm, 2004.
- Mayorov A. Yu., Antsiferov M. B. Modern means of self-monitoring and insulin administration in optimizing the treatment of patients with diabetes mellitus // Collection of materials of the Moscow City Conference of Endocrinologists on February 27-28, 1998 / Development of a patient education system in endocrinology: schools for patients with diabetes mellitus diabetes, obesity, osteoporosis, menopause. M., 1998. pp. 43-49.
- Bantle JP, Neal L., Frankamp LM Effects of the anatomical region used for insulin injections on glycemia in Type I diabetes subjects. Diabetes Care, 1996.
- Engstrom L. Technique of insulin injection: is it important? Practical Diabetes International, 1994, 11: 39.
A. Yu. Mayorov , Candidate of Medical Sciences, ERC RAMS, Moscow
Is it necessary to change the location of injections?
The area of the body where insulin is administered for diabetes should be changed periodically. If you constantly inject at one point, the subcutaneous fatty tissue will be damaged. Seals (lipohypertrophy) will form in it, which significantly impairs the effectiveness of drug absorption.
With the next one, you need to retreat at a distance of at least 1.5-2 cm from the previous puncture. You also need to alternately inject into the stomach, arm, and leg. The alternation should be consistent - this will ensure a stable level of glucose in the bloodstream. You can “return” to the place of the previous injection no earlier than three days later.
The level of compensation for type 1 diabetes depends not only on compliance with the diet and medication schedule, but on how competently the necessary procedures are carried out. The patient and his relatives should master the technique of correct insulin administration as quickly as possible - this will significantly improve the patient’s quality of life.
Where to inject insulin for diabetes?
Before considering how to properly inject insulin, you need to find out which areas of the body are suitable for this.
- Shoulder (outer surface). One of the most painless areas. Injecting the drug into this area ensures rapid absorption.
- Stomach. The most common area. This is where the hormone is absorbed most quickly. In addition, it is convenient to give injections into the abdomen yourself without outside help. It is only important to avoid the navel area.
- Back. It is possible to inject the hormone under the shoulder blade, but the substance will enter the bloodstream slowly.
- Buttocks. The surface is mentally divided into 4 equal parts. The hormone is injected into the upper outer square (left on the left buttock, right on the right).
- Thigh (front surface). The area is suitable for administering long-acting insulin. This is where the slowest absorption comes from.
Your doctor will help you determine the optimal place to administer the hormone. Explaining how to properly inject insulin, the specialist will clarify that it is extremely undesirable to inject in one place all the time. If a specific area is regularly used, it is divided into fragments.