What is this?
Tularemia is a bacterial infection that can be contracted through contact with wild animals or ticks.
It is not as well known as rabies or tick-borne encephalitis, although it causes a lot of problems for humans. The disease causes inflammation and suppuration of the lymph nodes, which sometimes have to be removed. The clinical form of tularemia depends on the method of penetration of the pathogen into the human body. Most often, after infection with tularemia, damage to the lymphatic system develops (the lymph nodes become inflamed); the disease affects the skin and mucous membranes of the eyes, pharynx and lungs. An acute disease is accompanied by high fever and signs of intoxication.
The source of tularemia infection is the bacterium Francisella tularensis. This is a very tenacious microbe that can survive for a long time in water, soil, grain and straw. It is stable in the environment, able to survive at very low temperatures. Surprisingly, F. tularensis remains viable even after being deep frozen for a long time. It can be stored in ice for more than 10 months, and in frozen meat for up to 3 months. At the same time, the bacterium is sensitive to ultraviolet radiation, heat and the effects of disinfectants. For example, upon contact with a Lysol solution, the causative agent of tularemia dies within 3–5 minutes.
How does infection occur? Vectors of infection and routes of transmission
Various types of rodents, birds, dogs, sheep and goats make a major contribution to the spread of infection. Despite the fact that the natural reservoir of tularemia is mainly mammals, the main carrier of the disease is insects that feed on the blood of infected animals, including ticks of the genus Ixodes. In addition to a tick bite, the cause of illness in humans can be:
- direct contact with an infected animal;
- eating raw foods and unboiled water;
- inhalation of dust in industries where plant materials are processed or livestock is slaughtered (Fig. 1).
The disease is not transmitted from person to person.
Important! Tularemia is extremely contagious and, when it enters the human body, causes disease in almost 100% of cases.
Figure 1. How a person becomes infected with tularemia. Source: CC0 Public Domain
Foci of tularemia appear every now and then in: Russia, Kazakhstan, Turkmenistan, countries of Eastern Europe. To a lesser extent, tularemia is common in Western Europe, the USA, Canada, China and Japan.
In Russia, the European part of the country and Siberia are considered dangerous from the point of view of tularemia infection. The spread of the infection is being carefully monitored, despite the relatively low incidence - in 2021, only 71 cases of the disease were registered in our country.
The seasonality of the infection (increased incidence usually occurs in summer and autumn) is associated with the period of activity of ticks and other blood-sucking insects. Previously, most human cases were recorded in rural areas, where people are more likely to come into contact with animals and be in nature. However, in recent years, about ⅔ of all cases are city residents. The reason for this is the frequent trips of city residents to the forest or to their dachas, as well as the consumption of raw meat.
Who is at risk?
The risk group for tularemia includes people who frequently come into contact with animals or agricultural raw materials:
- hunters,
- fishermen,
- veterinarians,
- shepherds,
- animal shelter staff,
- livestock workers,
- cooks,
- agricultural workers, etc.
Why is the tularemia vaccine necessary?
This infection belongs to the category of acute zoonotic, which is transmitted to humans from animals and carried by insects. The disease occurs only in certain regions and countries. Russia is on the list of states where you can encounter the vector. Ticks, mosquitoes, mosquitoes and horseflies can infect not only humans, but also pets. Therefore, tularemia has begun to gain momentum in recent years.
enlarged cervical lymph node
Why is vaccination against tularemia carried out?
- In Russia, over the past decades, the number of cases of disease has increased from 60 to 500 per year.
- In almost 100% of cases, this infection can be treated with conventional antibacterial drugs, but the healing process lasts up to several months.
- One of the symptoms is enlarged lymph nodes, which are called buboes; they can take up to 4 months to heal.
- The number of deaths does not exceed 0.5%, but when the pathogen enters the bloodstream, pneumonia, inflammation of the brain, psychosis, and even inflammation of many joints can develop.
So should you be vaccinated against tularemia? It is included in the vaccination calendar for epidemic indications, that is, it is not mandatory for everyone, but is necessary for a certain category of people who are at risk for tularemia. Treating a disease for several months, trying to get rid of complications that will bother a person for a long time, and healing aesthetically unpleasant buboes is a troublesome task and not always effective. The disease sometimes becomes chronic and periodically recurs during a sharp decrease in immunity.
Vaccination against tularemia is necessary, but not for everyone, since the likelihood of encountering the infection varies among people in different areas.
Forms of the disease
After entering the body, the tularemia bacillus attacks the lymph nodes, as well as internal organs - the liver, spleen, and less often - the lungs. Depending on how a person became infected, the disease manifests itself differently (Table 1).
| Table 1. Clinical forms (classification) of the disease | |||
| Form of the disease | Type of infection | Which organs are affected? | Symptoms |
| Bubonic | Through the skin | The lymph nodes | Lymph nodes enlarge significantly, sometimes reaching the size of a chicken egg. The contours of the lymph nodes (buboes) are clear. They hurt when pressed. As the disease progresses, the buboes may dissolve or fester. Possible formation of abscesses and fistulas |
| Ulcerative bubonic | After being bitten by a tick or other insect | Bite site | A small ulcer with a dark bottom appears at the site of the bite, which heals very slowly |
| Oculo-bubonic | In case of contact with eyes with dust or dirty hands | Eyes, lymph nodes | Conjunctivitis: inflammation of the eyes with redness, swelling, tenderness and stinging. Papular formations, which then turn into wounds and purulent ulcers |
| Anginal-bubonic | After drinking contaminated food or water | Pharyngeal mucosa, lymph nodes | High temperature, enlarged lymph nodes. Sore throat, problems swallowing, redness and swelling of the tonsils. The tonsils are enlarged and covered with a gray coating that is difficult to remove. Later, long-healing ulcers form on the tonsils, and then scars |
| Abdominal | After drinking contaminated food or water | Lymphatic vessels in the intestines | Abdominal pain, nausea, vomiting, weight loss |
| Pulmonary | After inhalation of contaminated dust | Bronchial lymph nodes, lungs | Fever, cough, chest pain |
| Generalized | Does not depend on the type of infection, but most often develops when the pathogen is inhaled | Spread of infection through blood, sepsis | Fever, weakness, confusion, headache, muscle pain |
The incubation period of tularemia, when there are no symptoms yet, usually does not exceed 3-7 days. The first manifestation of the disease is a high temperature, which rises to 38-40 °C. After this, the patient begins to suffer from muscle pain and headaches, feels constant weakness and dizziness. The fever lasts a long time and subsides only after 2-3 weeks.
During the examination of the patient, the doctor observes redness and swelling of the face, a noticeable increase in the vascular network of the eyes or “red eye” syndrome, and dark red spots – hemorrhages – are visible on the mucous membrane of the mouth. The tongue is covered with a white or gray coating. The main characteristic sign of infection is greatly enlarged lymph nodes (Fig. 2).
Figure 2. Lymphadenitis due to tularemia. The disease often affects the cervical lymph nodes. Source: Coronation Dental Specialty Group
In the later stages of the disease, blood pressure decreases and the pulse becomes rarer. On the fifth day from the moment the first symptoms appear, a severe dry cough develops. Most patients have an enlarged liver and spleen.
Diagnostics
Considering the strong seasonality, locality, occupation characteristic of a high risk of infection, and pronounced symptoms, the clinical diagnosis of tularemia is not very difficult.
Laboratory diagnosis is confirmed by identifying antibody titers or x-ray (for the pulmonary form). Bacteriological and PCR methods make it possible to detect the presence of a pathogen in biological samples taken from a patient.
Which doctor should I contact?
Having felt the symptoms and arrived at the clinic, the patient goes to the local therapist. He, in turn, gives a referral to an infectious disease specialist, who makes a decision on hospitalization.
An infectious disease specialist diagnoses and treats tularemia.
Tests for tularemia
There are several methods for laboratory diagnosis of tularemia.
Allergological methods
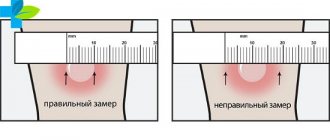
At an early stage of the disease, starting from the third day after the onset of symptoms, an allergy test is used for diagnosis. The test involves injecting the patient subcutaneously with tularemia antigen. In case of infection, the diameter of the swelling at the injection site is larger than usual in healthy people - at least 0.5 cm. The test results are assessed 24, 48 and 72 hours after the injection.
Serological methods
Serological diagnostic methods (agglutination reactions and passive hemagglutination) involve examining patient blood samples for the presence of specific antibodies. Depending on the chosen method, the disease can be diagnosed already on the 7-15th day of its course.
Bacteriological diagnostic methods
The bacteriological method consists of isolating the infectious agent from blood samples or the contents of the patient’s ulcers and buboes on days 7-10 after infection. The bacteria are then grown in a special nutrient medium. This approach to diagnosing tularemia is used very rarely because of its labor intensity, and also because not all laboratories have permission to work with F. tularensis.
Polymerase chain reaction
Polymerase chain reaction (PCR) is a diagnostic method that allows you to detect pathogen DNA in a biological sample. The sensitivity and specificity of PCR are not inferior to agglutination and passive hemagglutination reactions, and the method can be used already on the 10th day of illness.
“Tularemia in Russia in the recent past,” reports A.A. Nafeev, a sanitary doctor at the Center for Hygiene and Epidemiology in the Ulyanovsk Region, was one of the most common natural focal infections. Despite the successes achieved in the fight against this infection, cases of the disease are still registered annually. This dictates the need to improve sanitary and epidemiological surveillance, as well as the constant vigilance of outpatient doctors in relation to the first symptoms of tularemia.”
Conclusion about tularemia vaccination
As a result, it can be argued that the vaccine against tularemia is necessary for people who live in endemic areas or those whose work involves animals. The pros and cons of tularemia vaccination is an extremely controversial issue.
Vaccination is carried out by applying the reagent to slightly cut skin where, under normal circumstances, the body's response should occur. Cellular and humoral immunity once formed lasts up to five years.
If, under any circumstances, you have been infected with tularemia, immediately consult a doctor for an accurate diagnosis! An infectious disease doctor, having carried out diagnostic measures, will determine the presence or absence of contraindications to vaccination, explain to you how the drug works and what it is, prescribe treatment and give recommendations on prevention. After which, he will send a notification about the infectious disease to the district SES to take measures to deratize and detoxify the affected area.
Treatment
The treatment of tularemia is based on antibiotic therapy. To defeat a disease, it is necessary to destroy its source - the bacterium.
Drug therapy aimed at combating the infectious agent
The generally accepted standard of treatment for tularemia is antibiotics from the aminoglycoside and tetracycline groups. Third-generation cephalosporins and fluoroquinolones are used as second-line drugs.
The course duration is usually two weeks. In the event of a relapse of the disease, a drug that was not used during the first wave of the disease is chosen to continue treatment, since the bacteria could have acquired resistance to the previously used antibiotics.
Symptomatic treatment
Patients with symptoms are recommended bed rest and a balanced diet rich in vitamins. The ward is disinfected daily.
As symptomatic treatment, drugs are used to reduce the harmful effects of intoxication, allergic reactions and inflammation. Vitamins and medications may be prescribed to support the cardiovascular system. In case of eye damage, they are washed and instilled with a 20-30% solution of sodium sulfacyl 2-3 times a day. For tularemic sore throat, gargling is prescribed.
Treatment of ulcers
To treat ulcers and speed up the resorption of buboes, compresses and bandages with ointment are used. Physiotherapy procedures may be indicated: exposure to heat, blue light, laser irradiation, etc.
If the bubo has festered, it is opened and cleaned.
Possible complications
The vast majority of patients with tularemia can be cured without consequences. But in approximately 1-2% of cases of the disease, complications are observed, mainly related to the generalized form of tularemia.
Common complications include:
- meningitis and meningoencephalitis,
- secondary pneumonia,
- infectious psychosis after tularemia,
- chronic joint damage - polyarthritis,
- progressive heart disease - myocardial dystrophy,
- chronic course with frequent relapses.
Mortality with tularemia is less than 3%, with a generalized form - 30-60%.
Prevention
To protect yourself from infection, you should remember to take precautions while being in nature, when contacting animals, and eating meat and animal products. Vaccination remains the most effective method of prevention.
Is there a vaccine? Is it effective?
The most reliable way to protect yourself from infection is to get vaccinated. The effectiveness of vaccination against tularemia exceeds 90%; in Russia it is recommended for adults and children over 7 years old living in dangerous regions.
To protect against infection, a live vaccine containing weakened bacteria that cannot cause disease is used. On days 5–7 and 12–15 after vaccination, the strength of immunity is assessed. If immunity is not formed, re-vaccination is carried out. The state of immunity of vaccinated people is checked 5 years after vaccination and subsequently every 2 years.
Emergency unscheduled preventive vaccination is carried out in the presence of epidemiological indications:
- in case of illness of people in this territory,
- with intensive reproduction of rodents,
- with widespread carriage of tularemia among one or more animal species over a large territory.
Precautions in nature
Measures to reduce morbidity include controlling the spread of infection, carrying out deratization measures and disinsection of hazardous areas.
In case of a water outbreak, it is forbidden to drink unboiled water, as well as to swim. To reduce the risk of infection from tick and mosquito bites, it is recommended to use repellents, wear closed clothing, and limit the entry of unvaccinated people into disadvantaged areas.
To prevent commercial infections, it is advisable to use gloves when removing skins from killed rodents and to disinfect your hands.
It is necessary to carry out sanitary education work among the population of areas disadvantaged by tularemia. Persons who have been in contact with the patient are not isolated, since the sick are not contagious. The patient's home is disinfected.
How the tularemia vaccine works
Prevention methods help prevent severe infections. We are talking about vaccination. The vaccine against tularemia contains a portion of microbial cells: they enable the immune system to form the correct response to the causative agent of the disease.
The drug for tularemia (and there is only one) is called “Live tularemia vaccine.” The ampoule contains a dry substance - lyophilisate, intended for dissolution in liquid. In addition to the directly active substance, the product contains additional components (sucrose, sodium glutamate monohydrate, etc.) that promote absorption.
There is only one drug for vaccination against tularemia - “Live tularemia vaccine”
Vaccination options
There are two ways to administer the vaccine into the human body:
- Subcutaneous. Moreover, 0.1 ml of the reconstituted drug contains (1.0±0.1) x 10 x 7 living pathogen cells.
- Cutaneous. Applying small incisions to the skin. In 0.1 ml of the drug there will already be (2.0±0.5) x 10 x 8 microbial cells.
In each specific case, the vaccination method is chosen by the attending physician.
Is the tularemia vaccine mandatory?
The vaccine against tularemia is not included in the routine vaccination calendar (as, for example, vaccination against tuberculosis, measles, tetanus, polio, etc.). That is, it is not mandatory, which is understandable: many citizens of the Russian Federation live in natural conditions that are not conducive to the spread of this infection. However, if adults and children live in a region with a dangerous infectious situation, vaccination against tularemia for children is already carried out as planned. Most often, it is done at school (the health worker distributes forms in advance to the students, where parents must express their consent or refusal of vaccination), you can also go to the clinic for this purpose.
Most often, children are vaccinated right at school.
Naturally, no one will force a child to be vaccinated. But if there are periodic outbreaks of infectious foci in the region, doctors will strongly recommend that parents get vaccinated.
Children are immunized only from 7 years of age. The vaccination provides protection against tularemia for 5 years, after which revaccination will be required.
You should be aware that certain categories of the population are particularly at risk of contracting tularemia. These are people working in agriculture, livestock farming, working in mills, in grain barns, processing the skins of small rodents, and hunters. If the father or mother of the child is employed in such areas, this is an additional reason to vaccinate the baby.
If the child’s father, for example, is a hunter, then the risk of contracting tularemia increases
Immunity after vaccination is developed after 20–30 days. However, at the time of vaccination the child must be healthy. Otherwise, the opposite effect may work: the body will be affected by the bacterium instead of creating protection against it.