How does Diaskintest differ from the Mantoux reaction?
Due to the fact that the drug DIASKINTEST contains proteins that cause an immune response only to the presence of pathogenic (capable of causing disease) mycobacterium tuberculosis, the test has a higher sensitivity compared to the Mantoux river (the ability to detect infection in those who actually have it ) and, most importantly, higher specificity (the ability to give a negative reaction in those who do not have an infection).
Mantoux, Diaskintest test, Quantiferon test or T.SPOT? How do the methods for diagnosing tuberculosis differ and which one to choose?
Decoding the results
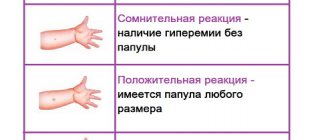
Pediatricians and therapists evaluate the results of DST. There are three possible interpretations:
- Negative. This result indicates that there are no active tuberculosis bacteria in the patient’s body.
At the injection site, you can see a direct injection mark and a slight bruise.
- Positive. This result is characterized by the appearance of redness and infiltration at the injection site of the diagnostic drug.
A compaction of more than 15 mm may indicate an active infectious process in the body. In this situation, you should also pay attention to the lymph nodes, which may be inflamed and enlarged.
- Doubtful. Most often observed during the formation of a large bruise, when assessing the size of true hyperemia and infiltration is problematic. In such a situation, a repeat study is indicated.
Attention! When performing Diaskintest, false results are possible. Their causes are non-compliance with doctor’s recommendations, the development of an allergic reaction to the drug and the presence of autoimmune diseases in the patient.
Parent Questions
Is it possible to do Diaskintest if allergies worsen?
Yes, but against the background of desensitizing therapy (5 days before and 2 days after the test).
Is it possible to eat sweets while on Diaskintest?
Can. But if you know that sweets can provoke an exacerbation of skin allergies, then it is better not to give them to your child.
Is it possible to do Diaskintest with a runny nose?
Yes, if it is not accompanied by an increase in temperature.
Is it possible to do Diaskintest immediately after an illness?
You should wait 2-3 days after the temperature has returned to normal. Residual runny nose and cough are not a contraindication and will not affect the results of Diaskintest.
Can Diaskintest provoke tuberculosis?
Preparations for Diaskintest are obtained from genetically modified strains of Escherichia coli, which in no case can cause the development of tuberculosis. Diaskintest is usually very well tolerated, only in rare cases there is a short-term and slight increase in temperature, mild headache and malaise.
Is it possible to wet Diaskintest and is it possible to go to the pool after Diaskintest?
Yes, you can wet Diaskintest and wash yourself. But it is still better to avoid exposure to chemical irritants (shampoos, reagents in the pool). Also try to prevent the child from scratching the sample.
What should a child not do after Diaskintest?
You should not rub or scratch the injection site, or apply any chemicals (iodine, brilliant green, hydrogen peroxide, creams) to it; for the same reason, you should not visit the pool. Everything else (walking, swimming, eating everything that does not cause an allergic reaction in your child) is possible.
What to do if a purple bruise remains after Diaskintest?
Don't worry ahead of time. Firstly, the bruise may completely disappear by the time of the test. Secondly, the size of the bruise also matters. During the test, the doctor will measure your reaction to the test and give you precise instructions on what to do next.
Can there be a fever after Diaskintest?
Yes, elevated temperature after Diaskintest in children is quite possible. Usually the discomfort does not last long and goes away on its own without treatment. What to do if you have a high temperature after Diaskintest? Most likely, it is associated not with the tests being carried out, but with ARVI or another disease that coincided with the time of Diaskintest.
Is it possible to get vaccinated after Diaskintest?
The interval between vaccinations (including BCG) and Diaskintest should be at least 1 month. If the Diaskintest result is negative, you can start vaccination immediately after the test.
Is it possible to do Diaskintest after Mantoux?
Yes, you can do Diaskintest after the Mantoux test.
Is it possible to refuse Diaskintest?
Yes, you can refuse Diaskintest and replace it with other tests for tuberculosis, such as the Mantoux test, quantiferon test or T-spot, as well as fluorography for children 15-17 years old. We do not advise you to refuse tuberculosis tests as such: the epidemic situation in Russia remains tense.
You can always ask all your questions and consult about Diaskintest in your particular case with our pediatricians by phone: +7 812 331 00 00.
Timing and indications for Diaskintest
The main indication for conducting a diagnostic test is the detection of tuberculosis among the population under the age of 18 years. Diaskintest is a screening test. As a rule, the test is given annually to children from 8 to 17 years old, but other options are also possible:
- DST is indicated once every 6 months if the child has not been vaccinated with the BCG vaccine within the period established by the national calendar.
- Children aged 1 to 8 years can be tested only if tuberculosis is suspected as a result of a positive Mantoux test.
Statement of DST is possible no earlier than a month after acute infectious diseases or vaccination and 2 months after receiving a negative result. If the test is positive, a repeat test is allowed as soon as possible.
The principle of action of the drug "Diaskintest"
The action of the drug "Diaskintest" is based on the detection of a cellular immune response to antigens specific to Mycobacterium tuberculosis. When the drug is administered intradermally in persons with tuberculosis infection, a specific skin reaction occurs, which is a manifestation of delayed-type hypersensitivity.
To identify (diagnosis) tuberculosis infection, a test with Diaskintest is carried out:
- children sent to an anti-tuberculosis institution for additional examination for the presence of a tuberculosis process;
- children belonging to high-risk groups for tuberculosis, taking into account epidemiological, medical and social risk factors;
- children referred to a phthisiatrician based on the results of mass tuberculin diagnostics (Mantoux).
Important! A test with the drug "Diaskintest" cannot be used instead of a tuberculin test (Mantoux) to select individuals for primary vaccination and revaccination with BCG
Test specifics
Tuberculosis is a socially significant disease that is caused by an infectious agent - Koch's bacillus. Most often, tuberculosis affects the lungs, less often other organs (kidneys, skin, bones, eyes).
Tuberculosis is widespread among the population of different countries. Previously, it was believed that only socially disadvantaged sections of the population were susceptible to tuberculosis. However, observations in recent years indicate the opposite. Anyone can become infected with tuberculosis, regardless of social status and material wealth.
So, the diagnosis of tuberculosis involves:
- bacteriological examination of a smear obtained from sputum;
- X-ray examination of the lungs and other organs;
- fluorographic examination;
- immunological tests (Mantoux test, Diaskintest).
Bacteriological examination of a sputum smear is not always informative, especially in the early stages, and requires compliance with certain rules for the collection and storage of sputum. The result of x-ray and fluorographic examination must be differentiated from other diseases that give a similar x-ray picture.
The Mantoux reaction also has a fairly large error. Among all the above methods for diagnosing tuberculosis, the Diaskintest test is by far the most informative and reliable.
The drug is administered exclusively intradermally with a special tuberculin syringe with a thin short needle with an oblique cut. The test is carried out in a medical institution by a specially trained specialist (in the vaccination room of the clinic) in compliance with all the rules of asepsis and antiseptics. The drug is administered against the background of complete health.
Administration of the drug is not allowed in the following cases:
- epilepsy;
- acute or exacerbation of chronic infectious diseases;
- somatic diseases in the acute period;
- extensive skin lesions due to dermatological diseases;
- complicated allergic history.
The test is performed with caution and only in case of urgent need for women during pregnancy and breastfeeding. The test result is assessed by a phthisiatrician or a nurse at a phthisiological or vaccination office.
Contraindications
"Diaskintest" is not used if the child is sick with some kind of acute infection (he is coughing, has a runny nose, high temperature and other symptoms), as well as within 1 month after recovery. The solution is not used for any diseases with a chronic course, if they have worsened (you must first treat such an exacerbation, and then do a test). A contraindication for such a drug is an allergic condition, in which allergy symptoms are first eliminated and only then Diaskintest is administered.
An obstacle to performing the test will also be any skin disease, in which there are pustules, rashes and other skin lesions in the forearm area. If a child visits an institution where quarantine has been declared for chickenpox or another infection, Diaskintest is used only after the quarantine period has ended.
Vaccination or test?
The essence of the drug is in its name. Diaskintest (DST) is a test, not a vaccination. It reflects the body’s reflex to the activity of tuberculosis bacilli and helps prevent the development of a serious disease. This is the immune system's response to protein allergens entering the body, which states how "familiar" it is with these antigens. A positive reaction indicates: “sign” – infected or sick.
Since 2015, the drug has been used to detect tuberculosis in children 8-17 years old. In children under seven years of age inclusive, the mass diagnosis of the disease remains the same. Mantoux and Diaskintest are similar in their action, but a positive DST reaction is an indisputable indication for starting anti-tuberculosis chemotherapy.
How often to test for tuberculosis
Children and adults at risk should be tested for TB at least once a year. In many children's institutions there is a rule: do a test for the Mantoux reaction 2 times a year.
Diaskintest is carried out simultaneously with Mantoux, most often the injections are given on different hands.
The most dangerous disease is also epilepsy and other pathologies of the nervous system.
After preventive vaccinations, the Diaskintest test is carried out a month later.
Now you know what it is - Diaskintest, what in most cases is a contraindication to using this drug, and in what cases it is used. People who have received a test with this drug leave only positive reviews. The main thing is to be aware of contraindications to the use of the drug and not to vaccinate during dangerous periods.
Interpretation of a positive result in children and adults
In a child and an adult, a positive result means the presence of an immune response to the introduction of Mycobacterium tuberculosis antigens. However, this should be interpreted differently.
For reference. In children, the first detected positive reaction is called a turn. The turn means that the body first encountered Koch bacilli and infection occurred.
The child has either already suffered primary tuberculosis, after which a persistent immune response remained, or is currently experiencing it. In order to identify the activity of the process, it is necessary to consult a specialist and conduct additional research methods.
For reference. In adults, the result should normally be positive.
The likelihood that a person came of age in an epidemically unfavorable place and did not encounter mycobacteria is very low. It is impossible to distinguish active tuberculosis from inactive tuberculosis using Diaskintest alone.
The strength of the reaction, as a rule, correlates with the activity of the process. The more pronounced the response to the antigen, the greater the chance that a person is currently suffering from tuberculosis, but a consultation with a TB specialist is still needed to make a diagnosis.
From the point of view of prognosis, it is better for a patient with tuberculosis if the immune response is pronounced.
Similar articles:
- What is excretory urography of the kidneys, how is it performed? Excretory urography is a research method. Let's look at the name of the method so that...
- What is FGDS of the stomach? How is FGDS of the stomach performed? In official medical terms, this is gastroscopy...
- Quantiferon test - new in the diagnosis of tuberculosis The Quantiferon test for tuberculosis is a tube test using ...
- How to carry out a breath test for Helicobacter The breath test allows you to literally within an hour without much discomfort...
Why do you need to get the DST vaccine?
The causative agent of the disease is Mycobacterium tuberculosis. Develops against a background of decreased immunity, malnutrition, frequent hypothermia, malnutrition, HIV infection, drug addiction, and nervous hypothermia. Transmitted in several ways:
- Airborne: through communication, sneezing, contact with a patient;
- Household: when using dishes, things, kissing, etc.;
- Through contact with the carrier;
- Food: eating affected food;
- Intrauterine: from mother to child.
In the acute form of tuberculosis, a prolonged and wet cough with sputum production is observed; hyperthermia. The patient sharply loses weight, complains of fatigue, and a general deterioration in health. Performance is lost.
The cough is wet and pronounced. Occurs in the form of frequent attacks, especially in the morning. Often the disease at the initial stage is mistakenly confused with “smoker’s cough”, symptoms of chronic bronchitis.
According to statistics in the CIS countries, approximately 90% of people are carriers of Koch's bacillus. In this case, 5% get sick. The development of tuberculosis depends on the level of immunity. Therefore, the main method of preventing the disease is maintaining a healthy lifestyle. Children are required to be vaccinated; regular samples and tests are carried out, with the help of which it is possible to establish in the early stages. Diaskintest is a solution that helps identify the disease in the early stages.
Expert opinion
Author:
Alexander Vyacheslavovich Averyanov
Pulmonologist, Doctor of Medical Sciences, Professor, doctor of the highest qualification category
According to statistics, 90% of the population are carriers of the Koch bacillus, the causative agent of tuberculosis. However, the incidence is recorded in only 5%. The disease develops against the background of immunodeficiency, so it is important to lead a healthy lifestyle and engage in prevention.
Diaskintest allows you to diagnose tuberculosis. The method differs from the classical Mantoux in its accuracy. The effectiveness of Diaskintest is 90%. For comparison, Mantoux's accuracy ranges from 50 to 70%. The Yusupov Hospital uses Diaskintest to diagnose tuberculosis. The method is also effective for preventive purposes. Results are assessed after 72 hours. Diaskintest is well tolerated and rarely causes allergic reactions. Even if individual intolerance to a component of the test occurs, undesirable reactions disappear after 2–3 days.
Diaskintest has proven itself on the positive side with most domestic doctors. Diagnostics is being actively introduced into medical institutions. High efficiency allows you to prescribe correct treatment. This is important, since tuberculosis is characterized by a progressive course and high mortality without adequate therapy.
What not to do after Diaskintest
Diaskintest results are assessed 3 days after the injection. To exclude a false positive test result, you must follow the following rules:
- do not rub the skin in the injection area after washing;
- do not apply cosmetics (soap, shower gel, body lotion, cream, perfume, etc.) to the injection area;
- do not cover the injection area with a compress, bandage or adhesive plaster;
- when regularly applying medications to the injection area, temporarily abandon this measure or warn the doctor;
- exclude possible allergens from the diet (especially for children) - citrus fruits, seafood, eggs, strawberries, etc.;
- do not wear constrictive, itchy woolen or allergenic synthetic clothing;
- avoid hypothermia, overheating and visiting crowded places;
- do not rub or scratch the injection site; if itching, use antihistamines (Loratadine, Suprastin, etc.);
- temporarily give up active sports;
- exclude visiting the pool, bathhouse, sauna, solarium and beach;
- do not drink alcohol.
Contact with water and touching the skin at the injection site does not affect the result of the study.