Description
The central catheter is a long, thin tube that is inserted into a large vein. A central catheter is used to deliver medications, nutrition, intravenous drugs, and chemotherapy into the bloodstream.
There are different types of central catheters, including:
- Peripheral central catheter - the catheter is inserted through a vein in the arm until it reaches a vein close to the heart;
- A non-tunneled central venous catheter is inserted into a large vein in the neck or leg; the end of the tube is outside the skin.
- A tunneled catheter is a catheter that is secured in place when scar tissue forms. It can be used for several weeks or months. The catheter is inserted into a large vein in the neck, which returns blood to the heart. It is then advanced along the chest wall and removed through the skin at a distance of about 12 cm from the injection site into the vein.
- Port catheter - a device inserted into a vein in the shoulder or neck. A port (titanium chamber) is placed under the skin and a catheter is inserted into a central vein. To administer medications, the port membrane is pierced with a special needle, and for the next 3-5-7 days, any solutions in any quantities can be injected through this needle.
Rules of care
It is important to remember that each type of catheter has its own, strictly defined period during which it can remain in the vein without risk to the patient’s health. For steel catheters, the installation time should not exceed 24 hours, for polymer catheters - no more than 3 days. At this time, systematic special treatment of the device is necessary, which allows not only to prevent bacteria from entering the bloodstream, but also to prevent occlusion (blocking) of the device ports, which inevitably occurs due to the “growth” of plasma clots and drug residues.
Consequences of improper catheter maintenance
What happens if you do not maintain the catheter promptly and correctly? At first glance, this device is completely harmless and is designed to reduce the number of invasive interventions in the patient’s body, but improper and untimely care of the catheter or the surface of the arm at the catheterization site can lead to serious consequences.
The main dangerous complications typical of catheterization are phlebitis and abscess.
Phlebitis with PVK is inflammation of the walls of the venous bed as a result of prolonged mechanical or chemical exposure.
Mechanical irritation is explained by the fact that a foreign object - a metal or plastic needle - has been in the vein for a long time. During any procedural manipulations or simply careless movements of the patient, mechanical impact on the vein walls cannot be avoided. The longer the catheter is in the bloodstream, the higher the risk of phlebitis.
Chemical irritation occurs as a result of the administration of certain drugs. This may depend on the concentration or feed rate of solutions.
An abscess with PVK is a purulent inflammation localized at the site of direct catheterization and resulting from non-compliance with asepsis rules.
An airtight dressing can also have a negative impact due to the accelerated growth of bacteria and fungi in such an environment. In this regard, it is not recommended to apply airtight dressings, except in cases where the catheterization site is close to open or burn wounds or tracheostomies.
In hospital settings, specialists constantly conduct bacteriological cultures of drug residues and patient blood from the surfaces of the catheter and skin at the site of venipuncture. This is done to conduct analysis and prevent the risk of infectious infection of the venous bed, as well as tissues near the catheterization site.
When using the device, it is necessary to regularly inspect the catheterization site and the vein above the catheter. At the slightest sign of redness or swelling, the device must be removed immediately. This can be done simply by lightly pressing the skin at a distance of 7–10 cm above the catheter, smoothly pulling it towards you, and after the needle comes out, bend your arm at the elbow, pressing a swab soaked with an antiseptic to the venipuncture site.
Flushing the catheter ports
Typically, the catheter has two ports covered with caps of different colors - white and colored (according to the target labeling). The colored valve closes the port for direct administration of medications using conventional injection syringes, and the white valve closes the port for infusions, i.e. this is where the dropper is connected.
To avoid infection of the bloodstream, which inevitably arises when using a catheter for a long time, it is necessary to flush the device. Typically, a heparinized solution or saline solution is used for this, which is drawn into a sterile disposable syringe, after which the needle is removed.
Immediately before this manipulation, the valve is removed and pressing on the syringe plunger ensures flushing of the port.
Depending on the total time, frequency of direct use and composition of the drugs, catheters can be washed regularly, from one to three times a day, or after each infusion session. The latter is most preferable.
The fact is that the cavity of the device port is a comfortable environment for the development of decomposition bacteria, and blood clots and drug residues, growing, can cause clogging of the tube, which reduces the capacity of the catheter initially declared by the manufacturer.
For rinsing, either pure saline solution (0.9% sodium chloride solution) is used, or the same solution, but in combination with heparin. The combined solution is prepared at the rate of 100 IU (0.02 ml) of heparin per 1 ml of 0.9% NaCl.
There is no need to prepare a solution for flushing in advance; we focus only on the internal volume of the venous catheter, i.e. 5–10 ml will be enough.
Reasons for performing the procedure
A central catheter is inserted when the patient needs:
- Administer medications or fluids long-term;
- During chemotherapy;
- For nutrition, if food intake through the digestive system is impossible;
- Periodic blood sampling;
- Blood transfusion;
- For intravenous administration of drugs when the veins in the arm are difficult to access;
- For dialysis.
The central catheter is usually inserted by an interventional radiologist or vascular surgeon. Once inserted, the catheter can be used for several weeks to months.
Intraurethral administration of drugs (istilation)
(From the book by A.P. Azizov Prostatitis, fiction and reality, Makhachkala, 2004)
VIII. Treatment methods for chronic prostatitis
Old venereologists say that you can put into the urethra what you can confidently put into the eye. We adhere to the rule of being very careful during instillations and other manipulations with the urethra (urethroscopy, endourethral physiotherapy, bougienage, catheterization, instillation of various chemically aggressive drugs).
Where possible, efforts should be made to avoid these procedures. With all the above procedures, irritation, cauterization, and trauma to the mucous membrane of the urethra occur, and the quality of the mucus produced by the paraurethral glands and its bactericidal properties deteriorate. At this stage, the likelihood of infection of the urethra from the outside by pathogenic or conditionally pathogenic flora, which was previously harmlessly present here, increases sharply.
It is necessary to point out the ineffectiveness of instillations with a syringe, without the use of a catheter, when the drug is administered only into the anterior part of the urethra. The external sphincter does not allow it to enter the posterior prostatic section, where the inflammatory process during prostatourethritis is mainly localized. No matter what kind of sanitation we carry out in the anterior urethra, infected material - urine, mucus, sperm coming from above from the posterior section will not allow it to remain clean.
Whenever indications for instillation are specifically identified, it should be performed through a catheter. Chlorhexedine, miramistin for instillation should be diluted 5-10 times. Dimexide should be used in a concentration of 5-10%. Quite widely for instillations in our practice, we use a standard solution of Metrogyl for intravenous infusion or various formulations with an antibiotic on dimexide.
We often use urethral instillation with solutions of dioxidin , chlorophyllipt , lysozyme , interferon , as well as a mixture of the following composition: 10% solution of dimexide 5.0 ml, rifampicin 0.15, oil solution of retinol acetate 2.0 ml.
- Dioxidin , 1% aqueous solution, 10 ml is injected into the posterior urethra; simultaneously inject 30 ml of the same solution into the rectum. The patient does not urinate for 2-3 hours, the procedure is carried out daily or every other day, No. 15-20. If necessary, repeat 2-3 courses with an interval of 30 days.
- 0.5% iodine-fir solution, the basis for the preparation of which is a 10% solution of fir oil in fish oil. For instillation after urination, 8.0-10.0 0.5% iodine-fir oil solution , which is held for 10 minutes and released outside (this is how the tolerance of the drug is checked). When administered again with a slight massaging movement, the drug moves into the posterior urethra, after which the patient refrains from urinating. The procedure is carried out every other day, No. 15-20. If necessary, 2-3 courses are repeated with an interval of 10 days. At the same time, it is recommended to inject 30-40 ml of 0.25% iodine-fir oil solution in the form of microenemas.
The following composition is also successfully used for instillations:
dimexide 0.5% - 400.0 + dexamethasone 0.1% - 30.0 + doxycycline - 8.0 + metrogyl 0.5% - 60.0.
For chronic torpid urethritis and urethrogenic prostatitis, V. A. Molochkov, I. I. Ilyin (1998) widely use daily rinsing of the anterior and posterior parts of the urethra with a weak solution of potassium permanganate (1:10000-1:6000) , furatsilin (1:5000) , silver nitrate solution (1:4000) , mercury oxacyanide (1:800) , 5-10% dimexide solution, irrigation with a complex enzyme preparation cataferm (50PE dissolved in 4 ml of distilled water). In the presence of a mild infiltrate or granulation, urethral instillation is prescribed with solutions of silver nitrate (0.25-1%), protargol (1-2%) , Ligenten gel (contains gentamicin sulfate, etonium, lidocaine; has bactericidal and bacteriostatic properties against staphylococci , streptococci, fungi of the genus Candida, etc.), 1% solution of dioxidine, ectericide , microcide , 0.001-0.005% myrimistin , 5% hydrocortisone suspension 1 time in 2-3 days. If there is no effect, limited areas of mucosal lesions are lubricated with a 10-20% silver nitrate solution through the urethroscope tube at intervals of 5-6 days, for a course of 3-5 procedures. For trichomonas urethritis, instillation with a solution containing 20 g of protargol, 15 g of osarsol and 300 ml of distilled water gives a good effect. For desquamative urethritis, instillations are used 2 times a day with a 1% solution of zinc sulfate or a mixture of the following solution: Zinci sulfatis, Plumbi acetatic aa 1.0; Aq. dest 200.0 . For transitional infiltrate and urethral adenitis, bougienage of the urethra is used with straight or curved bougie of increasing diameter (for a course of 8-12 bougie for 1-1.5 minutes) with urethral massage on a bougie or urethral tamponade according to Vashkevich . To do this, a urethroscopic tube (No. 25-27) is inserted into the anterior urethra up to the external sphincter, the obturator is removed, and a cotton swab soaked in a 2-3% glycerin solution of protargol or 1-2% solution of collargol, loosely screwed onto a smooth round probe, is inserted through the tube. Holding the probe, remove the urethroscope tube, then remove the probe from the tampon. The tampon is left in the urethra for 1-3 hours, after which it is removed from the urethra by a stream of urine when urinating. Tamponade is performed 2-3 times a week, a total of 6-8 procedures per course of treatment (V. A. Molochkov, 1998).
Share link:
- Telegram
Liked this:
Like
Possible complications after insertion of a central catheter
Complications are rare, but no procedure is guaranteed to be risk-free. Before you install a central catheter, you need to be aware of possible complications, which may include:
- Bloodstream infections, when bacteria enter the bloodstream through or around the central line;
- Bleeding;
- Lung collapse;
- Arrhythmia (unstable heartbeat);
- Nerve damage;
- An air bubble or part of the catheter may block blood vessels, causing chest pain, shortness of breath, dizziness, and rapid heartbeat;
- Blood clots in a vein or catheter can block blood flow.
Factors that may increase the risk of complications include:
- Smoking;
- Difficult access to veins;
- Blood clots;
- Obesity;
- Broken bones;
- Infection;
- Poor blood circulation;
- Bleeding tendencies.
How much does it cost to put in an IV with your medicine?
The higher cost applies to liquids with various vitamins or electrolytes and other medications. Keep in mind that fluids and other suggested treatments can easily be obtained through other means (taking generic vitamins and other over-the-counter medications) for only a few hundred rubles. Remember that the dropper allows you to quickly saturate the blood with essential microelements and is indispensable in the emergency treatment of patients.
How much does it cost to get an IV at the Latum clinic? Infusion therapy without the cost of the drug is only 700 rubles, so almost all patients can undergo the procedure with a high level of medical services in our clinic.
How is a central catheter inserted?
Preparation for the procedure
- A blood test may be done to check blood clotting;
- The doctor may ask about allergies;
- You need to arrange a trip home after the procedure;
- The patient may be asked to stop taking certain medications a week before the procedure: Aspirin or other anti-inflammatory drugs;
- blood thinners such as clopidogrel or warfarin;
Anesthesia
The area where the catheter will be inserted is numbed with local anesthesia. Depending on where the central catheter will be inserted, a sedative may be given intravenously.
Description of the procedure for inserting a central catheter
This procedure can be done either in a hospital as part of treatment or on an outpatient basis.
Having a catheter increases the risk of bloodstream infection. Hospital staff should perform the procedure while taking the following steps to reduce this risk:
- Care must be taken to select a safe place to insert the catheter;
- Wash your hands thoroughly or use hand sanitizer;
- You must wear surgical gowns, masks, gloves, and cover your hair;
- Cleanse the skin with an antiseptic;
- Use a sterile drape.
The next steps may vary depending on the type of catheter and where it is inserted. In general, staff will do the following:
- Anesthesia is administered;
- A small incision is made;
- X-rays or ultrasound are used to guide the catheter into the vein;
- Before installing the catheter, you need to cut it to the desired length. The catheter is flushed with saline (salt water);
- The catheter is guided using a catheter guide. The conductor is then removed;
- The catheter is secured to the skin (usually with adhesive tape). A cap is placed on the end of the catheter;
- A bandage is applied to the catheter insertion site. The date of insertion is marked on or near the bandage.
If a port catheter is inserted, a small cavity is made under the skin to accommodate it. The incision will be closed, usually with absorbable suture.
Immediately after the procedure
The insertion site will be checked for bleeding, fluid leakage, and swelling.
Preparing to insert a catheter
Before you begin installing a catheter yourself, you need to prepare the following set of tools and materials:
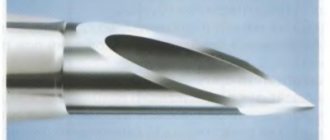
- Peripheral catheter of the required size.
- Syringe.
- An ampoule with saline solution or a pre-prepared heparin solution.
- Venous tourniquet.
- Bandage.
- Patch.
- Preferably sterile gloves.
- Sterile wipes.
- Any medical antiseptic or 70% alcohol.
- Tray for used materials.
Once you have prepared everything you need, you can begin to install the catheter into the vein.
If you intend to attach a drip, then at the time of catheterization the system should be completely assembled and filled with a medicinal solution.
Caring for the patient after the central catheter insertion procedure
Hospital care
After the procedure, staff may provide the following assistance to aid recovery:
- An x-ray is taken to ensure that the catheter is in the correct position;
- The catheter insertion site is periodically checked for bleeding;
- Medicines, fluids, or nutritional solution are given through the catheter;
- The port catheter is flushed to prevent blood clots;
- Steps are taken to reduce the risk of infection: Wash your hands and gloves thoroughly before touching the catheter or changing the dressing;
- An antiseptic is used to clean the exposed parts of the catheter;
- Precautions are taken when handling medications, fluids, or foods that will be administered through the catheter;
- The patient is monitored for signs of infection, which include fever, chills, and problems at the insertion site (eg, redness, swelling, drainage);
- Visitors should not be in the hospital room when the dressing is changed;
- The catheter remains at the insertion site as long as necessary.
There are also steps you can take to reduce your risk of infection:
- Employees should be asked to take all precautions to prevent infection;
- Personnel should immediately alert the physician if there is redness or pain at the catheter insertion site;
- You must wash your hands before entering the room. Visitors should not be allowed to touch the catheter.
Home care
When you return home, you should do the following to ensure a normal recovery:
- The insertion site should be kept clean, dry and bandaged. When changing the dressing, follow the doctor's instructions;
- You should wash your hands or use hand sanitizer before touching the catheter;
- You should ask your doctor about when it is safe to shower, swim, or expose the surgical site to water;
- Do not swim or bathe with a central catheter inserted;
- Any activity that could weaken the central catheter should be avoided;
- No one should touch the catheter;
- The injection site should be checked every day for signs of infection (eg, redness, pain);
- The catheter should be flushed with saline or heparin as directed by your doctor.
How to properly place an IV: procedure algorithm
In order to administer an intravenous infusion, appropriate knowledge, experience and strict adherence to technique are required. Correct placement of a drip is not only about inserting a needle without consequences for the patient, but also about choosing a system, infusion rate, etc.
Tools and accessories
To carry out the infusion, it is necessary to prepare the medications prescribed by the doctor (check the expiration date, volume and other important indicators), as well as instruments and consumables:
- Dropper stand. It is a portable stand with hooks onto which containers with solutions are placed. Its height is 1.5-2 m, which provides sufficient pressure for insertion.
- Infusion system. Droppers differ in the diameter of needles, tubes and the speed of infusion of drugs. It is very important to decide on the size of the needle, which is inversely proportional to the number: twenty-second is the thinnest, fourteen is the thickest. It depends on the anatomical features of the patient and the characteristics of the drug.
- Related accessories. In addition to a tripod and a system for placing an IV, you will need a tourniquet (it helps to find the vein), a patch to fix the needle and cotton wool.
In addition to the prescribed medications, you need to prepare an antiseptic liquid. Most often, alcohol is used; if a person has allergies, they take alcohol-free solutions (for example, Chlorhexidine).
Preparation for the procedure
Before manipulations, be sure to wash your hands and wipe them with an antiseptic. Failure to comply with hygiene rules can lead to infection and sepsis, even if the health worker has perfect infusion technique.
- Connect the system to the container or package with the drug. To do this, you need to wipe the needle with alcohol and pierce the cork - this is not difficult, since they are made of soft rubber or other materials.
- Hang the containers on the racks and secure them well. Be sure to check that there is no air in the system - fill the tubes and drip chamber about a third with liquid. Small bubbles are usually not dangerous - they will stick to the walls of the container and will not enter the bloodstream.
If sterility is violated at one of the stages, infusion is strictly prohibited. This can lead to blood poisoning and other dangerous consequences.
Placement of the IV
Before the procedure, it is necessary to familiarize the patient with the features of its implementation. Each drug has a special effect on the body, and some sensations may frighten a person. It is important to distinguish the side effects of drugs from the alarming symptoms that develop when infusions are performed incorrectly. Pain, dizziness, nausea, weakness and other discomfort should be reported to a healthcare professional immediately. The procedure algorithm is as follows:
- the patient takes a comfortable position - it is best to do the IV while lying down, but it is also possible in a semi-sitting or sitting position;
- the arm in the biceps area is tied with a tourniquet, the needle insertion site is thoroughly disinfected;
- the needle is inserted into the darkest, well-filled vein parallel to the surface of the arm at an angle of 35-45 degrees;
- after blood appears in the catheter, it is positioned as parallel to the limb as possible and fixed with an adhesive tape;
- connect the system tube to the catheter, make sure the connection is tight, and additionally secure it with a bandage;
- The rate of supply of the solution is adjusted using a dial with a wheel - sometimes the number of drops is marked on it to make counting easier.
During the procedure, it is necessary to monitor the patient and the needle insertion site. If the fluid flows too quickly, the person may become dizzy. In such a situation, it is better to simply reduce the infusion rate by turning the wheel in the desired direction.
After completing the procedure, it is necessary to close the system, carefully remove it, apply cotton wool soaked in alcohol to the injection site and press well. You need to keep it for at least 10-15 minutes, and preferably 20-25 minutes. During this time, a blood clot will form, which will clog the wound. If you remove the cotton too quickly, drops of blood will get under the skin, resulting in a bruise or bruise. Do not rub or touch the injection site, as this can also lead to the accumulation of blood clots.
Contraindications
Digging is prohibited for drunk people. The effect will be when a person oversleeps and a hangover comes.
Breaking out of binge drinking at home is a comfortable and productive method. However, for some, this procedure may be harmful. Home digging is contraindicated:
- for diseases of the heart and blood vessels;
- if a person drinks for more than a week;
- in old age;
- with diagnosed diabetes, asthma, alcoholic psychosis, especially during exacerbations.
It is better for everyone who is in the “risk group” to go to the hospital and undergo treatment under the supervision of a doctor.
Take a dip at home
Digging allows you to pump out a person, return him to normal life, to a state of sobriety. The dropper will restore the functioning of internal organs and systems:
- replenishing fluid loss;
- normalizing salt balance;
- absorbing toxins.
All drugs are administered intravenously. Once in the blood, they act instantly.
This procedure must be carried out by doctors. It is difficult for a non-specialist to cope with intravenous administration and to adequately assess the situation.
By calling a doctor to your home, you will be sure that a narcologist will assess the patient’s condition, measure blood pressure, conduct an examination, and only then select a set of medications for intravenous infusion.
Why do we need a port system?
Every year, many people are implanted with Celsite® port systems. Some for a few months, some for several years; it all depends on the duration of treatment. The doctor prescribes the implantation of a port system to avoid repeated intravenous interventions, which happen every time new courses of chemotherapy are prescribed. With repeated catheterizations, significant injury to the veins occurs; Frequent infusions into peripheral veins and changing catheters can lead to the development of phlebitis.
The use of port systems in patients with cancer is an integral part of the “gold standard” of treatment.
Ports are widely used in Western European countries in patients with newly diagnosed cancer who are scheduled to undergo multiple chemotherapy sessions, especially with cytostatic drugs that cause damage to peripheral veins. In addition, infusion ports are placed in patients with thin peripheral veins in the arms and legs. In domestic oncology practice, ports are rarely used.
According to the recommendations of the European Oncology Association, the most rational option is to install a port system at the earliest stage of chemotherapy, before the appearance of peripheral phlebitis, in those cancer patients who are planning to undergo long-term chemotherapy.
In Western European countries, infusion ports are installed in 95% of all patients receiving long courses of chemotherapy.
The infusion port allows you to simplify the procedures for collecting venous blood for laboratory tests, significantly facilitate parenteral nutrition, increase the efficiency of transfusion of blood components, especially platelet concentrate, as well as a number of other manipulations that require the installation of a central intravenous catheter.