Types of injections
Injections are divided into several types, but the three most common types are subcutaneous (SC), intramuscular (IM) and intravenous (IV). The variety of methods of drug administration is due to the difference in the speed of its effect on the human body. For example, when the drug is administered subcutaneously, the effect occurs noticeably later than when administered intramuscularly. And with intravenous injection, the drug spreads throughout the body almost instantly.
- Subcutaneous injection is used when it is necessary to administer a drug between the skin and muscle, in cases where the immediate effect of the drug is not required. For example, when administering insulin or vaccination. It is most convenient to make subcutaneous injections in those areas of the human body where the skin is easily pulled back and folded - the thigh, the lateral surface of the abdomen, the shoulder, under the shoulder blade.
- The most common type of injection is an intramuscular injection. Most people, when they say that they can easily give an injection on their own, mean intramuscular injection of drugs. The main area for administering drugs in this way is the buttocks, and sometimes the shoulder and thigh. Most antibiotics, vitamins, antispasmodics, and antipyretics are administered intramuscularly. This method is the simplest; it is what doctors and paramedics use to quickly relieve pain, “bring down” the temperature, and lower blood pressure.
- An intravenous injection is a technically more complex method than the previous two, usually performed by specialists. It is used in cases where a quick therapeutic effect is required, while active drugs are administered.
- In addition to the three listed types, which are the main ones, there are other methods, for example, intradermal (i.c.) - the familiar Mantoux reaction. In addition, injections can be made into the joint cavity for some arthritis, into the spinal canal for meningitis, directly into the nerve trunks for pain relief, for example, in dentistry.
Negative sides
In modern society, there is a stereotype that treatment with injections is much more productive and will give the desired result faster, however, in most cases this is not the case. Nowadays there are enough drugs used orally, which are in no way inferior to treatment with injections. I would like to draw attention to the disadvantages of using the injection method.
- Everything related to injections causes hostility, pain, and fear.
- If sterility is violated, an infection transmitted only through blood, for example, viral hepatitis B and AIDS, can be introduced into the body.
- Complications can be caused by incorrect insertion; the needle may accidentally hit a nerve, which can lead to complex consequences.
- There are cases when, after the injection, the tissue at the injection site turns red, becomes painful, and in the worst case, an abscess may occur that will need to be opened.
- When given an injection, allergic reactions are more acute than when using the same drug orally in capsules or tablets. When administering injections, the possibility of anaphylactic shock is several times higher than in other cases.
Experts around the world strive to limit the number of injections . The best pharmacologists from leading companies see their task as creating drugs that act quickly and effectively when taken orally. It is unlikely that it will be possible to completely abandon injections, especially when treating emergency conditions, but minimizing the number and limiting the indications is a completely feasible task.
Positive sides
- Injections are effective in cases where rapid penetration of the drug into the blood and an immediate therapeutic effect are necessary.
- Injections are used when the drug cannot be administered through the oral cavity, as it will be destroyed in the gastrointestinal tract.
- It is impossible to drink the medication, for example, if you are unconscious or vomiting.
- The drug used, when administered by syringe, has a more pronounced and longer-lasting effect.
Technical side
Everyone in their life has been faced with the need to give themselves or loved ones a simple intramuscular injection. It's quite simple if you know how to do it and don't be afraid. The recommendations written below apply specifically to intramuscular injections, but it is better to entrust intravenous injections to people with medical education and not risk doing it yourself.
- Be sure to wash your hands with soap.
- Next, check the expiration date of the drug that needs to be administered.
- Taking the ampoule, shake it, lightly tap the tip with your fingernail so that no liquid remains in it, wipe the tip with a cotton swab moistened with alcohol.
- Then you need to open the ampoule with the medicine; to do this, remove the ampoule file from the cardboard box with the medicine. Taking the file, run it forcefully along the base of the tip several times, and then carefully break it off.
- Unpack the syringe without removing the cap from the needle and put it on the syringe.
- Carefully, without touching the needle, remove the plastic cap from it and draw up the medicine.
- Turn the syringe vertically up, and, holding it in this light position, tap it with your fingernail so that the air bubbles rise to the top.
- Press lightly to release air from the syringe; when a drop of medicine appears at the tip of the needle, stop.
- Place a cap on the needle.
- Place the patient on their stomach or side to relax the butt muscles.
- Mentally divide the buttock into four squares, the injection is made in the upper outer square.
- The place where the injection will be given must be wiped with a cotton swab dipped in an alcohol solution.
- To reduce pain, the skin at the injection site can be stretched or squeezed with the fingers of the other hand. In children, the skin should not be stretched under any circumstances; it should be compressed.
- With a sharp movement at a right angle, insert the needle 3/4 of the way through, that is, almost to the very end.
- Gradually, slowly, introduce the medicine.
- With a sharp movement, remove the needle and press the injection site with cotton wool moistened with alcohol.
- Massage the affected muscle.
If possible, limit the number of injections in one place; it is advisable not to inject in one area more than 2 times a week. To do this, alternate sides: on the first day, inject into the right side, on the second, into the left.
In addition, you may encounter the fact that the injection medicine is in powder form. In this case, you need to dilute it with special distilled water or novocaine in ampoules. To dilute the medicine you will need one syringe and two needles.
How to properly dilute powdered medicine
- Take an ampoule with liquid, it can be distilled water or novocaine, and use a needle to draw it into a syringe;
- Wipe the lid of the bottle with the powder with a cotton swab and alcohol and inject liquid from the syringe into it;
- Remove the syringe and shake the bottle well until the powder is completely dissolved;
- Then, draw the solution into the syringe again;
- Place a new needle on the syringe without removing the cap.
- The solution for administration is ready.
Injection technique and means of administering insulin
Home » Useful articles » Injection techniques and means of administering insulin
Lifelong insulin replacement treatment has become the main condition for the survival of patients with type 1 diabetes, and it also plays an important role in the treatment of a certain part of patients with type 2 diabetes. In the early years, there were quite a lot of problems associated with obtaining the drug, the technique of its administration, and changing doses, but gradually all these issues were resolved. Now, every diabetic patient with a need for insulin, instead of the phrase “We are forced to inject insulin,” should say: “We have the opportunity to inject insulin.” In recent years, interest in the possibilities of improving insulin therapy, i.e., bringing it closer to physiological conditions, has been constantly growing. A certain role here is played not only by the focus on reducing lifestyle restrictions and improving the quality of life, but also by recognizing the need for fundamental changes aimed at improving metabolic control. It is very important to correctly use insulin and modern means of its administration, which include syringes, syringe pens and insulin pumps.
Insulin storage
Like any drug, insulin has a limited shelf life. Each bottle must indicate the expiration date of the drug. The insulin supply must be stored in the refrigerator at a temperature of + 2 ... + 8 ° C (under no circumstances should it be frozen). Insulin vials or pens used for daily injections can be stored at room temperature for 1 month. You should also not allow the insulin to overheat (for example, do not leave it in the sun or in a closed car in the summer). After the injection, be sure to put the insulin bottle in a paper package, since insulin activity decreases under the influence of light (the syringe pen is closed with a cap). When transporting a supply of insulin (during vacation, business trip, etc.), it is not recommended to check it in your luggage, as it can get lost, break, freeze or overheat.
Insulin syringes
Glass syringes are inconvenient (require sterilization) and cannot provide a sufficiently accurate dosage of insulin, so today they are practically not used. When using plastic syringes, syringes with a built-in needle are recommended to eliminate the so-called “dead space” in which a certain amount of solution remains in a regular syringe with a removable needle after injection. Thus, with each administration, a certain amount of the drug is lost, which, given the scale of the incidence of diabetes, results in huge economic losses. Plastic syringes can be used repeatedly, provided they are handled correctly and hygienically. It is desirable that the dividing price of an insulin syringe should not be more than 1 unit, and for children - 0.5 units.
Insulin concentration
Plastic syringes are available for insulin with a concentration of 40 U/ml and 100 U/ml, so when receiving or purchasing a new batch of syringes, you should pay attention to their scale. Patients traveling abroad should also be warned that in most countries only insulin with a concentration of 100 U/ml and appropriate syringes are used. In Russia, insulin is currently found in both concentrations, although the world's leading insulin manufacturers supply it in a concentration of 100 units per ml.
Set of insulin in a syringe
The sequence of actions when collecting insulin using a syringe is as follows: • prepare a bottle of insulin and a syringe; • if necessary, inject long-acting insulin, mix it well (roll the bottle between your palms until the solution becomes evenly cloudy); • draw as much air into the syringe as the number of units of insulin you will need to draw later; • introduce air into the bottle; • first, draw a little more insulin into the syringe than needed. This is done to make it easier to remove air bubbles trapped in the syringe. To do this, lightly tap the body of the syringe and release the excess amount of insulin along with the air back into the bottle.
Insulin injection technique
Figure 1. Injecting insulin with needles of different lengths
The rate at which insulin is absorbed depends on where the needle is inserted. Insulin injections should always be administered into the subcutaneous fat, but not intradermally or intramuscularly (Fig. 1). It turned out that the thickness of the subcutaneous tissue in people with normal weight, especially in children, is often less than the length of a standard insulin needle (12–13 mm). Experience shows that very often patients do not form a fold and inject at a right angle, which leads to insulin entering the muscle. This was confirmed by special studies using ultrasound equipment and computed tomography. Periodic release of insulin into the muscle layer can lead to unpredictable fluctuations in glycemic levels. In order to avoid the possibility of an intramuscular injection, you should use short insulin needles - 8 mm long (Becton Dickinson Microfine, Novofine, Dizetronic). In addition, these needles are the thinnest. If the diameter of standard needles is 0.4; 0.36 or 0.33 mm, then the diameter of the shortened needle is only 0.3 or 0.25 mm. This is especially true for children, since such a needle causes virtually no pain. Recently, shorter (5–6 mm) needles have been proposed, which are more often used in children, but further reduction in length increases the likelihood of intradermal penetration. To give an insulin injection, you need the following:
Figure 2. Formation of a fold of skin for insulin injection
• free up a place on the skin where insulin will be injected. There is no need to wipe the injection site with alcohol; • with your thumb and forefinger, take the skin into a fold (Fig. 2). This is also done to reduce the likelihood of getting into the muscle. This is not necessary when using the shortest needles; • insert the needle at the base of the skin fold perpendicular to the surface or at an angle of 45°; • without releasing the fold (!), press the syringe plunger all the way; • wait a few seconds after injecting insulin, then remove the needle.
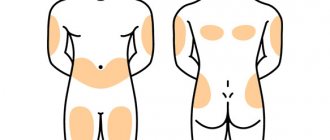
Insulin injection areas
Several areas are used for insulin injections: the front surface of the abdomen, the front surface of the thighs, the outer surface of the shoulders, buttocks (Fig. 3). It is not recommended to inject yourself into the shoulder, since it is impossible to form a fold, which means the risk of intramuscular injection of insulin increases. You should be aware that insulin is absorbed from different areas of the body at different rates (for example, the abdominal area is the fastest). Therefore, it is recommended to inject short-acting insulin into this area before meals. Long-acting insulin injections can be given in the thighs or buttocks. The injection site must be new every day, otherwise there may be fluctuations in blood sugar levels.
Figure 3. Insulin injection areas
You should also ensure that changes do not appear at the injection sites - lipodystrophy, which impairs the absorption of insulin (see below). To do this, it is necessary to alternate injection sites, and also retreat from the previous injection site by at least 2 cm.
Syringe pens
In recent years, along with plastic insulin syringes, semi-automatic insulin dispensers, the so-called syringe pens, have become increasingly common. Their device resembles an ink fountain pen, in which instead of an ink reservoir there is an insulin cartridge, and instead of a pen there is a disposable insulin needle. Similar “pens” are now produced by almost all foreign insulin manufacturers (Novo Nordisk, Eli Lilly, Aventis), as well as medical equipment manufacturers (Becton Dickinson). They were originally developed for patients with visual impairment who could not draw insulin into a syringe on their own. Subsequently, they began to be used by all patients with diabetes, as they can improve the patient’s quality of life: there is no need to carry a bottle of insulin with you and draw it with a syringe. This is especially significant with modern regimens of intensified insulin therapy, when the patient has to give injections multiple times during the day (Fig. 4).
Figure 4. Intensified insulin therapy regimen using multiple injections
However, mastering the injection technique using a pen syringe is somewhat more difficult, so patients should carefully study the instructions for use and strictly adhere to all instructions. One of the disadvantages of syringe pens is that when a small amount of insulin remains in the cartridge (less than the dose the patient needs), many patients simply throw away such a cartridge and the insulin along with it. In addition, if a patient injects short- and long-acting insulins in an individually selected ratio (for example, with intensified insulin therapy), then he is deprived of the opportunity to mix and inject them together (as in a syringe): he has to inject them separately with two “handles”, thus increasing number of injections. As in the case of insulin syringes, an important requirement for injectors is the ability to dose in multiples of 1 unit, and for small children - in multiples of 0.5 units. Before injecting long-acting insulin, you need to make 10-12 turns of the pen 180° so that the ball in the cartridge mixes the insulin evenly. The dial ring places the required dose in the housing window. Having inserted the needle under the skin as described above, press the button all the way. After 7–10 seconds (!), remove the needle.
In 1999, Novo Nordisk released a new syringe pen, Innovo. Due to a special mechanism, the length of the device was reduced. Like Optipen, the dose is displayed on the liquid crystal display. But the main difference from all previous modifications is that Innovo shows the time that has passed since the last injection and remembers the last dose of insulin. Also, the electronic control system guarantees accurate administration of the dialed dose. The range of administered doses is from 1 to 70 units, the dosing step is 1 unit. The set dose can be increased or decreased by simply turning the doser forward or backward without losing insulin. It is impossible to set a dose greater than the amount of insulin remaining in the cartridge.
Changing needles
Since a patient on insulin therapy has to make a huge number of injections during his life, the quality of insulin needles becomes of great importance. In order to ensure that insulin administration is as comfortable as possible, manufacturers are constantly making needles thinner, shorter, and sharper. To make insulin injection virtually painless, the needle tip is specially sharpened and lubricated using the latest technology. However, repeated and repeated use of the insulin needle leads to damage to the tip and abrasion of the lubricating coating, which increases pain and discomfort. A dull needle not only makes insulin injection painful, but can cause local hemorrhage. In addition, erasing the lubricant on the needle increases the force of pushing the needle through the skin, which increases the risk of bending the needle and even breaking it. However, the main argument against repeated use of a needle is microtrauma to the tissue. The fact is that when the needle is reused, its tip bends, taking on the shape of a hook, which is clearly visible under a microscope (Fig. 5). When the needle is removed after insulin is administered, the hook ruptures the tissue, causing microtrauma. This contributes to the formation in a number of patients of protruding compactions (plus tissue) at the sites of insulin injections, i.e. lipodystrophies. In addition to causing cosmetic damage, lipodystrophic lumps can have serious medical consequences. Often, patients continue to inject insulin into these seals due to the fact that injections in these places are less painful. However, insulin absorption at these sites occurs unevenly, which may result in poor glycemic control. Quite often in such situations, an erroneous diagnosis of “labile diabetes” is made.
Figure 5. Deformation of insulin needles after repeated use.
Repeated use of the needle can cause insulin crystals to clog the channel, which in turn makes insulin delivery difficult and inadequate.
Repeated use of insulin pen needles can lead to another serious mistake. The instructions for syringe pens state that the needle must be removed after each injection. But most patients do not comply with this rule (due to the fact that an insufficient number of needles are provided free of charge). Thus, the channel between the insulin cartridge and the environment remains open. As a result of temperature fluctuations, insulin leaks and air enters the vial. The presence of air bubbles in the insulin cartridge causes insulin to be delivered more slowly as the plunger is pushed. As a result, the insulin dose administered may not be accurate. In the presence of large air bubbles, the amount of insulin administered in some cases may be only 50–70% of the administered dose. In order to reduce the influence of this factor, it is necessary to remove the needle not immediately, but 7–10 s after the piston has reached its lower position, which is what patients should be instructed to do.
What conclusions can be drawn based on all the above observations? Ideally, single use of insulin needles should be recommended; in addition, after each injection of insulin, the needle must be removed immediately.
Given the importance of the above points, doctors should periodically check the means of insulin administration, injection technique and the condition of injection sites in each patient.
Insulin pumps
Wearable insulin dispensers (insulin pumps) appeared in the late 1970s. The next decade was characterized by intense interest in these new technical means of administering insulin, and certain hopes were placed on them. After gaining experience and conducting a sufficient number of scientific and clinical studies, the pump “boom” subsided, and these devices took their definite place in modern insulin therapy. In Russia, Medtronic Minimed pumps are currently used.
When using dispensers, the following occurs (Fig. 6): to simulate physiological secretion through a cannula installed in the body (the injection site changes every 2–3 days), short-acting insulin is pumped continuously as a subcutaneous infusion (basal rate), and before meals the patient injects Various additional amounts of insulin (bolus).
Figure 6. Intensified insulin therapy regimen using a pump
Thus, the device is an “open” type system. This means that the patient regulates the insulin dosage himself, changing it depending on the results of self-monitoring of glycemia. The latter is the link that, as it were, “closes the chain”, forming feedback. One of the main advantages of current wearable pumps is the ability to vary the basal insulin infusion rate. Modern pumps allow you to set different speeds for each hour of the day, which helps to cope with such a phenomenon as the “dawn phenomenon” (an increase in glycemic levels in the early morning hours, forcing patients in this case to make the first insulin injection at 5–6 a.m.). Also, the use of pumps allows you to reduce the number of injections, show greater flexibility regarding the timing of meals and the amount of carbohydrates consumed. There are also implantable pumps in which insulin enters intraperitoneally, which means it enters the portal vein, as happens during normal insulin secretion.
However, numerous studies have shown that there is no significant difference in the level of metabolic control between patients using insulin pumps and those on a multiple-injection regimen. The biggest disadvantage is the high cost of pumps. The use of pumps is clearly justified in certain situations, for example, during pregnancy, in children with labile diabetes, etc. A miniature, portable device that not only injects insulin, but also has a sensor for determining glycemia, as well as an automated insulin supply function based on the results obtained, i.e., it would be an artificial b-cell, has not yet been developed for long-term clinical use. However, experimental models already exist, and mass production of such devices may begin in the near future. In this regard, interest in the use of conventional pumps has increased, since both medical workers and patients need to get used to handling complex technical devices.
Thus, today we have in our arsenal means of self-monitoring and insulin administration, which in many ways allow us to optimize the treatment of patients with diabetes. All that remains is to teach patients to use them correctly, which is no less difficult a task than the creation of these funds itself.
Literature
1. Berger M., Starostina E. G., Jorgens V., Dedov I. I. Practice of insulin therapy (with the participation of Antsiferov M. B., Galstyan G. R., Grüsser M., Kemmer F., Mühlhauser I., Sawicki P., Chantelau E., Spraulya M., Starke A.). 1st ed. Springer-Verlag, Berlin-Heidelberg, 1995. 2. Dedov I. I., Mayorov A. Yu., Surkova E. V. Diabetes mellitus type I: A book for patients. M., 2003. 3. Dedov I.I., Surkova E.V., Mayorov A.Yu., Galstyan G.R., Tokmakova A.Yu. Therapeutic training of patients with diabetes mellitus. M.: Reapharm, 2004. 4. Mayorov A. Yu., Antsiferov M. B. Modern means of self-control and insulin administration in optimizing the treatment of patients with diabetes // Collection of materials of the Moscow City Conference of Endocrinologists, February 27-28, 1998 / System development training patients in endocrinology: schools for patients with diabetes, obesity, osteoporosis, menopause. M., 1998. pp. 43-49. 5. Bantle JP, Neal L., Frankamp LM Effects of the anatomical region used for insulin injections on glycemia in Type I diabetes subjects. Diabetes Care, 1996. 6. Engstrom L. Technique of insulin injection: is it important? Practical Diabetes International, 1994, 11: 39.
It is not recommended to do the following
- Under no circumstances should you touch the needle with your fingers while preparing and administering the medicine. If you acted carelessly, touching or dropping the needle, it needs to be replaced. Otherwise, an abscess may appear at the injection site.
- Using a small needle or not inserting it deeply enough, when injecting you can get it not into the muscle tissue, but under the skin, where a compaction will quickly appear, which will subsequently fester. To avoid this, before the injection site turns red, apply a heating pad to help it dissolve.
- You should never give injections while standing; in this position, the muscle tissue does not relax enough and the needle may break.
- Be very careful when choosing the injection site, as you can accidentally hit a nerve, and then your patient will have to be treated by a neurologist for a very long time.
How to use Polyoxidonium suppositories
Medicinal suppositories are intended for rectal or intravaginal use. The total number of suppositories per course of treatment is 10 pieces. Repeated local therapy is allowed after 3–4 months.
The medicine is administered into the intestines once a day, in the evening, placing a 6 or 12 mg suppository 5–6 cm deep. Before the procedure, it is advisable to visit the toilet or do an enema. To relieve acute symptoms, the drug must be used daily. For maintenance therapy, it is enough to use it once every 2-3 days.
In the treatment of gynecological pathologies, 12 mg suppositories are used. They are administered before bedtime, placing them as deeply as possible into the vagina. For acute diseases, repeat the procedure for 3–4 days in a row, then proceed to maintenance treatment: 1 suppository every 2–3 days. For indolent chronic diseases, it is recommended to use suppositories 1-2 times a week.