Immunization protects pregnant women from vaccine-preventable diseases, followed by the transfer of acquired antibodies to the newborn. Antibodies passively acquired from the mother can protect the child from diseases in the first months of life. Maternal immunization is an important challenge facing public health practice.
Vaccination and vaccinations during pregnancy lead to the transplacental transfer of antibodies, which can provide protection to the newborn in the first months of life [17].
Widespread implementation of immunization of pregnant women, as an important public health goal for the prevention of neonatal diseases, in the United States and other industrialized countries faces obstacles stemming from theoretical doubts by expectant mothers about the safety of vaccines, relatively low awareness, and practical socioeconomic problems. The most important issue regarding immunization during pregnancy remains the safety of vaccines for the fetus and newborn [1]. The decision to vaccinate a pregnant woman is quite a responsible one. To make this decision, the doctor and the pregnant woman must jointly determine the potential risk of infection with a particular pathogen, as well as the possible consequences of infection for the mother and child. These risks must be weighed against the likely benefits of vaccination [2, 3].
Are live antiviral vaccines contraindicated during pregnancy?
It was believed that pregnancy is a contraindication to vaccination with live viral vaccines due to the theoretical risk of virus penetration through the placenta and intrauterine infection of the fetus. Live virus vaccines include attenuated influenza vaccine (LAIV), MMR (measles, mumps, rubella), and varicella, smallpox, and tuberculosis (BCG) vaccines. Current guidelines suggest that caution should be exercised when administering live viral vaccines during pregnancy. The US Advisory Council on Immunization Practices (ACIP) of the Center for Disease Control (CDC) does not consider vaccination to be an indication for termination of pregnancy [4, 5].
From 1979 to 1980 The CDC closely monitored the effects of RA 27/3 vaccine (live rubella virus vaccine) given to women within three months before or after conception; There are no data on the effect of the vaccine on the development of birth defects or congenital rubella syndrome [6]. Live attenuated polio vaccine was also well tolerated by pregnant women [7, 8].
When live viral vaccines (eg, rubella, chickenpox, OPV) were administered to pregnant women, there was no increase in the incidence of adverse events in the fetus or newborn. Some of these vaccines (eg, OPV, yellow fever) are indicated for pregnant women who are at high risk of exposure to infection.
The only live antiviral vaccine that is toxic to the fetus remains the smallpox vaccine. These vaccines should not be used in women of childbearing age without appropriate toasts confirming the absence of pregnancy, and should not be administered to family members of a pregnant woman.
Hepatitis B
Compared with adults, newborns and infants infected with hepatitis B virus have a greater risk of developing severe liver damage and even death or chronic liver damage.
The hepatitis B vaccine includes hepatitis B surface antigen (HbsAg) particles. which are unable to cause infection. CDC believes that its use cannot cause harm to the fetus [10]. In contrast, almost 90% of children born to mothers infected with hepatitis B virus in the last trimester developed chronic hepatitis if they were not vaccinated at the time of birth [11].
Prevention of hepatitis B
In reality, it is very easy to get infected with this virus. And if for HIV infection the minimum dangerous dose of blood is 0.1 ml, then for hepatitis it is 1 million times less. There are many situations in life in which infection is potentially possible.
There are specific and non-specific measures to prevent infection.
Nonspecific prophylaxis is aimed at preventing the virus from entering the body. It includes the following activities:
- using condoms during sexual intercourse;
- refusal to use other people's hygiene and care items (for example, razors, manicure accessories);
- use of disposable consumables when working with blood and biological fluids;
- protection of the skin of the hands and face when performing medical and cosmetic procedures (disposable gloves, mask, protective screen);
- refusal to use drugs, casual relationships;
- control over the processing of reusable surgical, dental, manicure instruments.
Specific prevention of viral hepatitis consists of timely vaccination. Since the likelihood of the process becoming chronic is highest when infected at an early age, it is important to vaccinate the child within the first months and even days of life.
The hepatitis B vaccine is included in the National Vaccination Schedule. Free administration is provided in the compulsory health insurance system for children and adults under 55 years of age. Persons over 55 years of age who do not have epidemiological indications are vaccinated at their own expense. There are no age restrictions for hepatitis vaccination for patients.
Tetanus
Tetanus toxoid administration is indicated for pregnant and lactating women who have not previously received immunization or require a booster injection. No negative effects of the tetanus vaccine on the fetus have been identified [12]. As a precaution, the CDC recommends vaccination after the end of the first trimester of pregnancy [5]. Although Tdap vaccination (acellular DTP vaccine with a reduced content of difluoride toxoid and pertussis component) during pregnancy is not specifically specified, there are also no contraindications to its administration.
Rubella
When infected with the rubella virus in the first 4 weeks. During pregnancy, in approximately 50% of cases, the fetus develops congenital rubella syndrome (CRS). including blindness, heart defects, deafness and other developmental defects [13]. By the third trimester, the risk of developing CRS in the fetus decreases to 10%.
Rubella vaccine is a live antiviral vaccine. It should not be administered to pregnant women due to the theoretical possibility of exposure of the fetus to the live virus. However, there were no cases of CRS development in newborns whose mothers were unscheduledly vaccinated or became pregnant within 3 months. After vaccination All women of childbearing age should be screened for rubella antibodies. Most cases of CRS have been reported in newborns whose mothers were not screened or vaccinated despite medical supervision [14].
Vaccinations - good or evil?
“Vaccination is one of the hottest topics on any social network. Despite the fact that in 2021 we have all become hostages of the COVID-19 pandemic and salvation is seen only in a vaccine, there are still a lot of “anti-vaxxers”. They react aggressively to the topic of vaccination and actively “recruit” all doubters into their ranks. There are more and more “refuseniks”. This is not only a Russian trend, it is a global trend. Several years ago, the World Health Organization put the problem of vaccination refusal on a par with such health threats as HIV, Ebola and poverty,” notes Tatyana Butskaya.
She emphasizes that a pregnant woman or an already accomplished mother must understand that she is responsible for her child, who, due to his age, cannot make important decisions. And the main thing here is not to make a mistake. “The argument “since everyone around is vaccinated, then the unvaccinated have nothing to fear” no longer works. Herd immunity protects if more than 95% of the population is vaccinated, and in our country this figure is lower. This means that diseases that were controlled in the past will increasingly create epidemics. For example, several years ago a severe outbreak of measles occurred in Europe. This was facilitated by the anti-vaccination lobby, which strengthened against the backdrop of insufficient awareness and fake data,” the expert notes.
Now the topic of vaccinations is extremely relevant. This means that those who did not have time to get vaccinated at the planning stage need to carefully consider their health issues and weigh the pros and cons.
For expectant mothers. What pregnancy myths should you not believe? Read more
Chicken pox
Infection of a pregnant woman can lead to the development of congenital chickenpox syndrome in the fetus, characterized by limb atrophy, strictures, microcephaly, cortical atrophy, and chorioretinitis. cataracts and other defects [15]. Compared to the first trimester, the risk of developing congenital varicella syndrome is slightly higher in the period from 13 to 20 weeks. pregnancy [16]. The effect of the vaccine on the fetus has not been proven. The risk of developing congenital varicella syndrome after infection with wild type virus is 0.4-2.0%; When using an attenuated vaccine, the risk of developing congenital varicella syndrome should theoretically be lower or completely absent [16].
Hepatitis A
The safety of hepatitis A vaccination during pregnancy has not been studied; however, since the hepatitis A vaccine is based on inactivated hepatitis A virus, the possibility of infection is theoretically very small. The risk associated with vaccination must be weighed against the possible risk of developing hepatitis A in a pregnant woman, especially if the risk of exposure to infection is high [18 ].
Literature:
- Munoz FM, Englund JA, Infect. Dis. Clin. North Amor. 2001: 15(1): 253-271.
- Silvers MJ. Steploe MM. Prim. Care Clin. Off. Pracl. 2001:28: 1-9.
- AnmncanCollegeotObntotnciansandGynecoiogisls, Committee on Obstetric Practice. Immunization during pregnancy. ACOG Com Opin. 2003; 282.
- Centers for Disease Control arxl Prevention. General recommendations on immunization, recommendations of tl»e Advisory Committee on Immunization Practices (ACIP) and the American Academy of Family Physicians (AAFP) MMWR Morb. Mortal. Wkly Rep. 2002; 51 (RR02): 1-36.
- Centers for Disease Control and Prevention. Guidelines for vaccinating pregnant women. 2004. Available at: https://www.in.gov/iHdh/programs/immunization/lmmunzationSchedGuldelines%20for%20Vaccinating%20Pregnant%20Women.pdf. Accessed January 25.2008.
- American Academy of Pediatrics: Poliowus infections. In Pickering LK (ed): 2000 Red Book Report of the Committee on Infectious Diseases, ed 25. Elk Grove Village. IL. American Academy of Pediatrics. 2000. pp. 465 470.
- DaSilva MM, Prom KA. Johnson FA. et at. JAMA 1958:1681 -1685-
- Linder N. Hands!ler R. Fruman O. et al Pedi.itr Infect. Ois J. 1994; 13:959-962
- Naleway AL. Smith WJ, Mullooly JP. Epidemiol Rev. 2006; 28: 47-53.
- Centers for Disease Control and Prevention Connecticut. 1994-1995 and United States. 1979-1994. MMWR Morb Mortal. Wkly Rep. 1996: 45: 584 -587.
- Estaban R. Vaccine 1995; 13(suppl 1): S35 - S36.
- Silveira CM. Caceres VM, Dutra MG. Lopes-Camelo J. CastMla EE Bulletin WHO. 1995:73.605-608
- AmencanColk*geofKtetriciansandGynecologists. ACOG N(ws Release November 29, 2002.
- HacktoyBKJ Nurse Midwifery 1999.44:106-117. 15- Centers for Disease Control and Prevention. MMWR Morb. Modal. Wkly Rep. 1996: 45 (RR* 11): 1-25.
- Pastuszak AL. Levy M. Schick In el al N. Engl. J Med 1994; 330: 901 905
- Englund. J. et al. Path 2007: 137: S16 - S19 18 COC. MMWR 2006: 55 (No. RR-7): 15
- CDC. MMWR 2006; 55 (No. RR-7): 15.
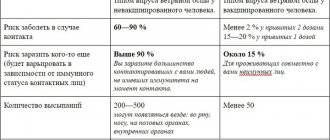
Table 1. ACIP recommendations regarding immunization during pregnancy or lactation
| Vaccine/toxoid | Use during pregnancy | Use during breastfeeding | Comments |
| Live attenuated viral vaccines | |||
| measles | No | Yes | usually included in MMR |
| parotitis | No | Yes | usually included in MMR |
| rubella | No | Yes | usually as part of MMR, 4 weeks in advance. before planned conception |
| polio | not routinely used | not routinely used | can be used when traveling to endemic areas |
| yellow fever | No | No | if contact with infection is unavoidable, it is possible to use |
| chicken pox | No | Yes | planning pregnancy after 4 weeks. after vaccination |
| Killed or inactivated vaccines | |||
| flu | Yes | Yes | Vaccination should be offered to all pregnant women in the second and third trimester. Can be used in women at risk in the first trimester |
| rabies | Yes | Yes | the disease is fatal in almost 100% of cases |
| Hepatitis B | Yes | Yes | |
| Pneumococcal infection | Yes | Yes | recommended for women at risk |
| typhoid fever | No | No | only when traveling to endemic areas |
| anthrax | No | No | recommended only for women at risk |
| tetanus | Yes | Yes | |
| diphtheria | Yes | Yes | |
Hepatitis E and pregnancy
Only recently was viral hepatitis E (HEV) recognized as “ours”, since in most of its few cases the disease among Russians was imported from hot countries. In foreign countries, HEV is almost an occupational disease of livestock farmers; more than three million people get sick there every year, and almost 60 thousand die. Hepatitis belongs to the virus company, A, and is also transmitted through dirt, which is called the “enteral route of transmission.” But unlike hepatitis, transmission of the virus is possible not only from person to person, but also from animals, and people become infected much less often. Two genotypes of the virus also live in our smaller brothers, two - only in humans. The E virus is less infectious than its other counterparts; it does not survive well without a host.
Incubation lasts about 40 days, but can last up to eight weeks. The onset period lasts from 3 days to a week with almost the same symptoms as hepatitis A. But the icteric period is different because the symptoms of intoxication remain, which is not the case with hepatitis A. In general, hepatitis E is much more severe, involving not only the liver, but also the nervous system, causing severe neuritis. Fatal kidney damage and coagulation system disorders are no exception. It is precisely the variant of fulminant and severe HEV that threatens a pregnant woman; hepatitis E and pregnancy are almost incompatible.
No hepatitis during pregnancy brings as many misfortunes as HEV: miscarriages, premature births, low survival rate of a full-term baby, death of a woman from renal failure and bleeding due to hemorrhagic syndrome. Childbirth and miscarriage further worsen a woman’s condition. And in all other categories of humanity, hepatitis E proceeds, although it is difficult, but mostly without misfortunes and with complete recovery. Although there is also a chronic form, we learned about it recently, but it only affects severe immune deficiencies and malignant tumors.
Hepatitis E is treated like hepatitis A, but with pregnant women everything is so complicated that information about how to treat it is scarce in the literature.