Whooping cough: prevention and treatment
According to WHO, 500-600 thousand children die from whooping cough every year worldwide.
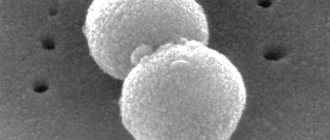
Whooping cough is a bacterial disease, it is transmitted from person to person, but in the external environment the germs of whooping cough, Bordet-Jongou bacteria, are not persistent, so the disease is transmitted only through close contact by airborne droplets: to become infected, you need to play or communicate with the patient. You cannot “catch” whooping cough by simply walking down the street past the source of infection. The source of infection is only the patient. When coughing, sneezing, screaming, talking, splashes of saliva containing an infectious principle enter the mucous membrane of healthy people and infect them. The most dangerous thing is that bacteria are released about a week before the onset of clinical manifestations. A person remains infectious for about two to three weeks while sick. Whooping cough is especially dangerous for children under two years of age.
Conclusion 1:
You need to carefully monitor who a small child is playing with or is in the same room with, and not allow them to interact with coughing children.
How the disease develops
Bordet-Jongou bacteria enter the body through the upper respiratory tract. There they settle in the walls of the bronchi. Small bronchi and bronchioles are more severely affected: foci of necrosis (death) appear there. Irritation from receptors in the respiratory tract is transmitted to the cough center in the brain. Toxins released into the blood by whooping cough microbes also irritate the cough center in the medulla oblongata. A focus of dominant excitation gradually forms (as in epilepsy). The immune system fights bacteria and after a short time they no longer remain in the body, but the cough center (focus) remains agitated and the whooping cough clinic continues.
Conclusion 2:
Whooping cough can be treated with antibiotics, but only at an early stage. By the time the diagnosis is usually made, that is, in the second week of the convulsive period, it is no longer the treatment of choice.
Clinical manifestations of whooping cough
As people in Asia say, whooping cough is a 100-day cough because whooping cough has a long course, that is, it is a very long-lasting cough.
The disease is divided into several periods:
- incubation;
- catarrhal period;
- spasmodic period;
- permission.
The duration of each period is different, depending on the age of the patient and the severity of whooping cough.
Incubation period for whooping cough:
can last from 4 days to two weeks, more often – about a week. This is a time when there are no clinical manifestations yet, but the child is already sick and even contagious.
Catarrhal period:
the disease begins with mild catarrhal symptoms, this is precisely the moment when bacteria multiply in the wall of the respiratory tract. But the symptoms are minor: a slight runny nose, a slight cough without sputum, and parents usually do not worry: they treat the runny nose and give expectorants. But the cough, which is dry from the very beginning, does not soften, and sputum does not appear.
Conclusion 3:
if there is reason to suspect that a child is infected with whooping cough (close contact with a patient, an epidemic in a kindergarten group), you can take a culture during the incubation period, diagnose whooping cough and take antibiotics when the Bordet-Jongou bacteria are still in the body. This will be effective and the severity of the disease will be significantly reduced.
Spasmodic period of whooping cough:
There are more and more coughing impulses in one attack, the child no longer has time to breathe. Most of all, the picture of each attack resembles a cough when a person chokes on something. Each cough impulse is a short exhalation. It seems that there is no more air left in the lungs, and the vocal cords are closed, and the cough continues. Finally, you manage to inhale, but with a whistle or wheezing, this is called a reprise. A dry, prolonged cough combined with repeated episodes is a classic clinical picture of the convulsive period of whooping cough. After inhalation, the cough continues, sometimes in one attack there are up to 3-4 repetitions. In severe cases of the disease, an attack can last up to 4 minutes. The pressure in the veins of the head and face increases, the face of a sick child turns red, and sometimes even pinpoint hemorrhages occur in the capillaries of the skin and eyes. When coughing, a sick child may stick out his tongue strongly and tears flow from his eyes. The attack either stops gradually or is resolved by vomiting. When coughing, the frenulum of the tongue is sometimes injured. There can be only a few such attacks per day with a mild course, or up to several dozen with severe whooping cough. With mild and moderate whooping cough, the general condition of children between attacks does not change: they feel well and play. In severe cases, patients are depressed, they are very tired when they cough, they sleep poorly at night, they show anxiety and are afraid of attacks. Since coughing during whooping cough occurs due to activation of the cough center, irritation of other centers of the brain can provoke an attack, and getting carried away with something relieves the dominant irritation and reduces the likelihood of a coughing attack.
Conclusion 4:
keep your child occupied with something. Any strong and positive emotional stress can contribute to rapid recovery
Resolution period
. Gradually, the frequency of attacks decreases, and the attacks themselves become shorter. The “whooping cough” cough is gradually replaced by an ordinary cough, which continues for about two more weeks. Since the cough center is irritated, resumption of the characteristic cough is possible with any cold. This is not a return of whooping cough, but a reaction of a recovered, but not restored, body to a new irritant.
Whooping cough in infants
Whooping cough in children under one year of age poses a serious threat to the baby’s life. There is a fulminant form of infection, in which the incubation period may be absent, and the catarrhal period is reduced to several hours. Increasing spasms of the respiratory tract quickly occur. Cardiovascular pathology is added. Clinical death may occur against the background of convulsive syndrome. Emergency placement of the baby in a specialized hospital is required. Very often, whooping cough in infants occurs in the so-called masked form. There are no pronounced reprises during coughing attacks. Instead, there is a sudden stop in breathing after a long bout of screaming and hysteria after several coughing shocks. There is a disturbance in the blood supply to the brain structures and heart muscle. A convulsive syndrome occurs, the baby's face turns blue.
Conclusion 5:
For children under one year of age, whooping cough is especially dangerous. Infants often do not develop a full clinical picture. Coughing attacks in children are shorter and there are no relapses, but during an attack breathing may stop.
What to do:
If a baby stops breathing due to whooping cough, it is necessary to urgently induce vomiting. To do this, you need to press on the root of the tongue. Activation of the vomiting center can restore breathing. It’s worth opening the window and taking the child outside. If these measures have no effect, artificial respiration must be performed. Urgent hospitalization is required. Consequences and complications: In children of the first year of life, whooping cough is dangerous due to respiratory arrests during attacks, the duration of which varies from several seconds to several minutes. Due to lack of oxygen, they may develop skeletal muscle cramps and encephalopathy. Other complications of whooping cough are bronchitis, pleurisy, purulent otitis media, and false croup. Occasionally, severe complications arise as a result of strong cough impulses (cerebral hemorrhage, ruptured eardrums, pneumothorax). Against the background of weakened immunity and a reduction in the intensity of lymph movement, stagnation begins in the lung tissue. The most common complication of whooping cough is pneumonia with the addition of staphylococcal, streptococcal, pneumococcal, Haemophilus influenzae and Pseudomonas pathogenic microflora. The disease in its severe form can lead to prolonged hypoxia, which manifests itself in impaired blood supply to the brain and myocardium. This can provoke severe consequences of whooping cough in the form of structural changes, including expansion of the ventricles and atria of the heart, and disruption of brain activity.
Conclusion 6:
after suffering from whooping cough, ask your doctor what infections the child should be vaccinated against in order to avoid further complications (against Haemophilus influenzae, pneumococcal and influenza)
Diagnostics:
The primary diagnosis is established based on the clinical picture and a general blood test. Then, to clarify the diagnosis, a bacteriological culture of sputum or a throat smear is performed. To more quickly establish a final diagnosis, a serological blood test can be performed to detect the presence of specific antibodies.
Treatment of whooping cough in children: what needs to be done and what you need to know?
- Remember about other people - those who were in contact with your child, and those who may be in this contact - isolate the child, tell friends that visits are undesirable.
- To kill a microbe - the choice of antibiotic (there are dozens of possible options), as well as the dose of medicine - is a matter for the doctor. The parents’ task is to ensure that the drug gets inside the patient, to comply with the prescribed doses, frequency and timing of administration. (It is not difficult to kill the whooping cough bacillus, although not all antibiotics work on it. But during the period of spasmodic cough, no effect - in the form of a decrease in the frequency and duration of attacks - can be noticed. And we already understand why - after all, the cough is not due to a microbe, but because for damage to the cells of the cough center. The main purpose of taking antibiotics during this period is to make the patient non-infectious)
- Treat the disease philosophically and realize that whooping cough is controllable only at the prevention stage. But if you get sick, time turns out to be one of the main factors on the path to recovery. In short, until you cough up your own, you shouldn’t really rely on any pills. (Since the cough is of central origin, that is, it does not arise due to inflammation in the respiratory tract, but due to irritation of the cough center in the brain, expectorants are not indicated. Cough stimulants are contraindicated: mustard plasters and cups)
- You should know that coughing attacks can be provoked by: physical activity, sneezing, chewing, swallowing, negative emotions. The conclusions from this knowledge are quite logical: do not arrange active games with running, jumping and rolling; Avoid dust in every possible way, remove the child from the room while cleaning; try to ensure that the food offered to the child does not require much chewing and, at least for the duration of the illness, forget about chewing gum. (Taking into account the previous point, feeding a child with whooping cough is a particular problem. For some children, the very process of absorbing food becomes so scary , that even the mention of food (for example, the phrase uttered by mom: “let's go eat") causes a coughing attack. Fortunately, this is rare, but coughing after eating and vomiting everything that has been eaten is quite common. You should not give a lot of food at once - even if he wants to eat a lot. The longer he chews and the more he eats, the greater the likelihood of an attack and vomiting. Therefore, it is better to feed more often, but little by little. In principle, coughing with vomiting after it rarely happens 2 times in a row - i.e. If there was vomiting after the attack, then the next 2-3 attacks will be easier)
- One of the most important factors in the treatment of whooping cough is the correct answer to the question “what to breathe?” The drier the air and the warmer the room where the child is, the thicker the sputum, the greater the likelihood of an increase in the frequency of attacks and the development of complications. But the traditional action when a child develops a cough is to keep him at home. And it is not surprising that after a month of coughing indoors, without walks and fresh air, the supposed “bronchitis”, which, in fact, was a mild whooping cough, ends with pneumonia. Therefore, it is necessary to remember and understand that fresh air is a prerequisite for proper care for a child not only with whooping cough, but also with other diseases accompanied by cough, bronchitis, tracheitis, allergic lesions of the respiratory tract, and pneumonia. But, since the “other diseases” we mentioned pass incomparably faster than whooping cough, the negative consequences of the home regime do not appear so often. Thus, if whooping cough is diagnosed, then all the patient’s relatives should be mobilized in order to take turns walking with the child. In the summer, of course, it is not advisable to be where it is dry and warm; you need to get up early, while it is humid and cool, and be sure to take a longer walk before going to bed. It is just important not to forget that during the festivities you should avoid communicating with other children. It is very good to walk near bodies of water, if there are any nearby. And if they don’t exist, then it wouldn’t be a bad idea to go to a place where they exist - to the village to visit grandma, to the dacha, etc.
- Any cold, any acute respiratory infection in a child with whooping cough greatly increases the manifestations of whooping cough itself and greatly increases the risk of complications - the same pneumonia. Preventive measures are quite standard - reduce contact with other people as much as possible, even if the child is no longer contagious, avoid hypothermia, isolate adults who have caught a cold.
- In principle, we should never forget about the possibility of developing pneumonia, and the idea that it has begun should appear when: - an increase in body temperature in the second or third week of illness, especially when the temperature has risen, but a runny nose has not appeared; – a sudden increase in coughing and an increase in the duration of attacks after it has been getting better for several days, or at least not getting worse; – changes in general health – weakness, rapid breathing – in the intervals between attacks. It goes without saying that a doctor will diagnose pneumonia if you call him, but whooping cough lasts for several months and is most often treated at home. It often happens that it is not very convenient for parents to frequently disturb the doctor, especially when the diagnosis is quite clear, and it is no less clear that recovery requires quite a lot of time. The above will help parents seek help in a timely manner.
- In the vast majority of cases, whooping cough can be treated quite safely (or goes away on its own) at home. But sometimes you can’t do without a hospital. So when? a) - whooping cough in children of the first year of life and especially (!) the first half of the year - the risk of complications is very high, and the disease at this age is almost always very severe; b) – regardless of age, when complications develop or when respiratory arrest occurs due to coughing. It is quite logical to note the following: no one will ever keep a baby in the hospital until he has fully recovered. But both the hospital doctor and the child’s parents, before saying goodbye to each other, must be confident that the disease has passed its peak (there are no respiratory arrests, complications have passed, within a few days the number of coughing attacks has begun to decrease). Treatment of whooping cough, of course, is not limited to antibiotics and fresh air. Although from the huge arsenal of medications that help with cough, there is not a single one that can significantly alleviate the course of the disease. The choice of a specific medicine is a matter for the doctor, but parents should know the following: even if, from your point of view, the prescribed medicine, for example, bromhexine, does not help at all, this does not mean that it is inappropriate to take it. The fact is that the mechanism of action of most expectorants (including the bromhexine we mentioned) is based on liquefying sputum. The child will not cough less often, but the likelihood of complications will decrease several times, since it is thick mucus, disrupting the patency of the bronchi, that is the main cause of the development of pneumonia
Prevention of whooping cough
Whooping cough in children has recently become increasingly common due to the large number of refusals to vaccinate against this infection. This vaccination is included in the national childhood vaccination schedule. However, many parents consider this event inappropriate and dangerous. In truth, it should be noted that of the three components of this vaccine, pertussis is the most difficult to tolerate - i.e. It is with this that all the unpleasant sensations that a child experiences after vaccination (malaise, fever, loss of appetite) are most often associated. In view of these fabrications, there is a conscious refusal to vaccinate with DPT.... According to the national vaccination calendar, vaccination against whooping cough is carried out three times in 3 times; 4.5 and 6 months, with a single revaccination at the age of 18 months. Vaccination protects against this disease at an early age, when it is most dangerous. In Russia, along with the domestic vaccine DPT (associated pertussis-diphtheria-tetanus toxoid), foreign analogues are registered - acellular vaccines Pentaxim, Tetrakok, Infanrix and Infanrix hexa. Your local doctor will help you decide which vaccine to vaccinate your child with.
Conclusion 7:
Don't refuse to vaccinate your children. Vaccination is the only reliable means of preventing whooping cough! Of course, vaccinated children can get whooping cough at an older age, but the disease is much easier. So much so that the diagnosis of “whooping cough” is made tens of times less often than this disease actually occurs and proceeds as a banal mild acute respiratory infection without the development of complications.
Plenkina L.L.
Karas N.A.
Diagnostic test scheme
The diagnostic scheme differs according to the patient’s age, as well as the presence of vaccination against the disease.
Diagnostic scheme for those who have not been vaccinated:
- in the first two weeks of illness, bacteriological examination or PCR is effective;
- at 3-4 weeks of illness, PCR or serological testing is used;
- more than 4 weeks of illness is an indication for serological examination.
While taking antibiotics, PCR is used.
For vaccinated persons, the following examination scheme is used:
- at 1-2 weeks of illness - PCR method, bacteriological analysis;
- PCR is used at 3-4 weeks;
- illness lasting more than 4 weeks requires serological diagnosis.